The aim of this work is to evaluate and compare the radiographic results and complications of the surgical treatment in adolescents with idiopathic scoliosis greater than 75 degrees, using a double approach (DA) or an isolated posterior approach with hybrid instruments (posterior hybrid [PH]), or with “all-pedicle screws” (posterior screws [PS]).
Materials and methodsA retrospective review was performed on 69 patients with idiopathic scoliosis greater than 75°, with a follow-up of more than 2 years, to analyze the flexibility of the curves, the correction obtained, and the complications depending on the type of surgery.
The Kruskal–Wallis test for non-parametric variables was used for the statistical analysis.
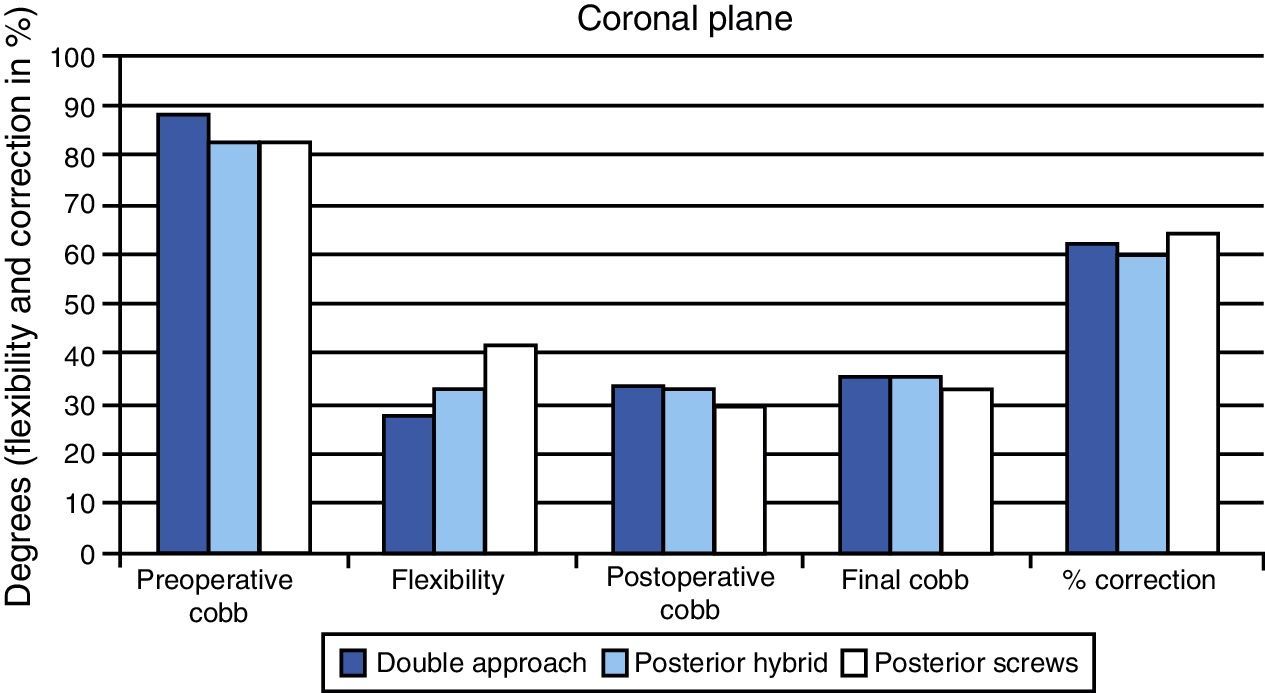
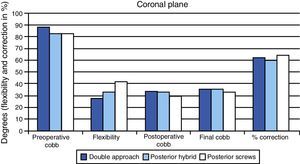
ResultsThere were no statistically significant differences between the 3 patient groups in the pre-surgical Cobb angle values (DA=89°, PH=83°, PS=83°), in the immediate post-surgical (DA=34°, PH=33°, PS=30°), nor at the end of follow-up (DA=36°, PH=36°, PS=33°) (P>.05). The percentage correction (DA=60%, PH=57%, PS=60%) was similar between groups (P>.05).
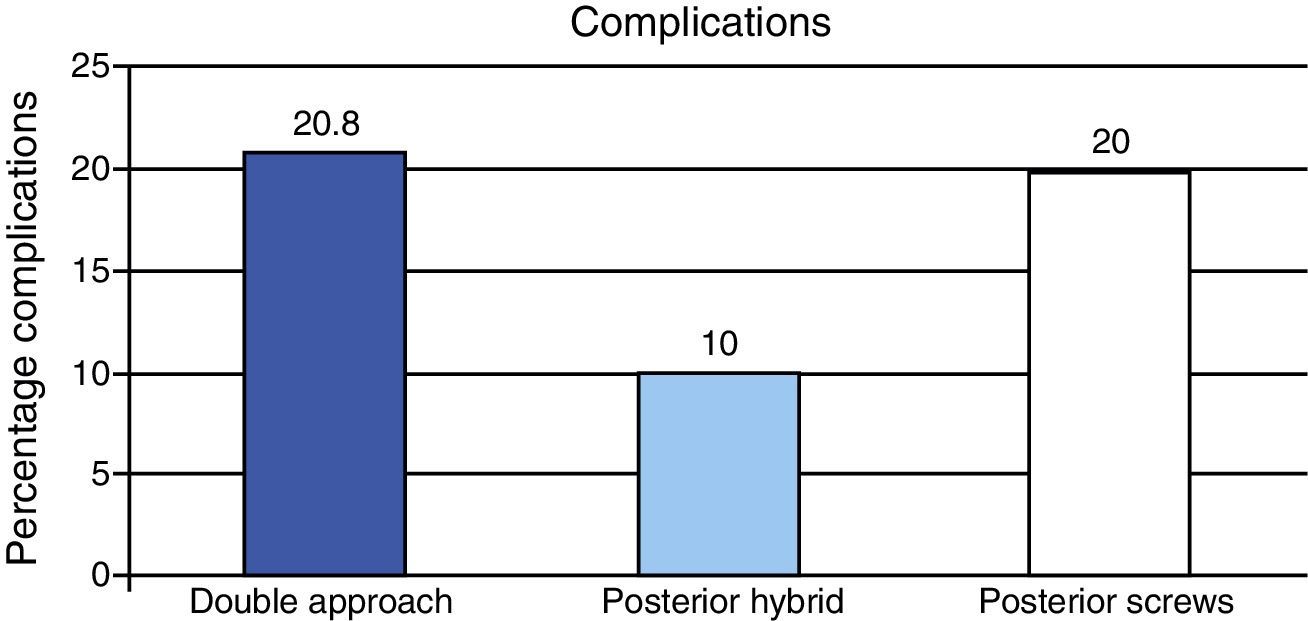
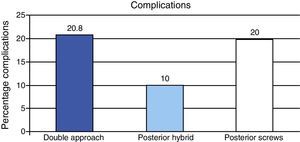
The percentage of complications associated with the procedure was 20.8% in DA, 10% in PH and 20% in PS. Two patients in the PS group showed changes, with no neurological lesions, in the spinal cord monitoring, and one patient in the same group suffered a delayed and transient incomplete lesion.
Discussion and conclusionsNo significant differences were observed in the correction of severe idiopathic scoliosis between patients operated using the double or isolated posterior approach, regardless of the type of instrumentation used.
El objetivo de este trabajo es evaluar y comparar los resultados radiográficos y las complicaciones del tratamiento quirúrgico de escoliosis idiopáticas del adolescente mayores de 75° mediante doble abordaje (DA) o vía posterior aislada con instrumentación híbrida (PH) o «todo-tornillos» (PT).
Material y métodoSe realiza una revisión retrospectiva de 69 pacientes con escoliosis idiopática del adolescente mayor de 75° y seguimiento superior a los 2 años para analizar la flexibilidad de las curvas, la corrección obtenida y las complicaciones en función del tipo de cirugía.
El análisis estadístico se realizó mediante el test de Kruskal–Wallis para variables no paramétricas.
ResultadosNo existen diferencias estadísticamente significativas entre los 3 grupos en los valores del ángulo de Cobb preoperatorio (DA=89°, PH=83°, PT=83°), en el postoperatorio inmediato (DA=34°, PH=33°, PT=30°) ni al final del seguimiento (DA=36°, PH=36°, PT=33°) (p>0,05). El porcentaje de corrección (DA=60%, PH=57%, PT=60%) fue similar entre grupos (p>0,05).
El porcentaje de complicaciones relacionadas con el procedimiento fue del 20,8% en DA, del 10% en PH y del 20% en PT. Dos pacientes en el grupo PT experimentaron cambios en la monitorización medular sin lesión neurológica y un paciente del mismo grupo experimentó una lesión incompleta diferida y temporal.
Discusión y conclusionesNo se aprecian diferencias significativas en la corrección de las escoliosis idiopáticas graves entre los pacientes intervenidos mediante doble abordaje o por vía posterior aislada, independientemente del tipo de instrumentación utilizada.
For many years, the combined surgical approach, consisting in anterior release and posterior arthrodesis (or fusion) followed by instrumented vertebral arthrodesis has been the treatment of choice for cases of severe and rigid scoliosis or those with significant alteration of the sagittal profile, as well as in skeletally immature patients in order to prevent the crankshaft phenomenon.1 However, recent publications have questioned the need for a combined approach, reporting satisfactory results in severe scoliosis using only a posterior arthrodesis.1–4
Release and anterior arthrodesis can be performed through an open approach, by thoracotomy/thoracolumbotomy or through a thoracoscopic approach,5 with similar results. Both the open and thoracoscopic approaches have a negative impact on lung function compared to an isolated posterior approach6 and may require a longer surgical and anesthesia time.
Instrumentation with screws in the lumbar spine has been shown to improve correction compared to the use of hooks.7,8 The use of pedicled screws in the thoracic spine, which provides better segmental fixation, has also increased in recent years. Different studies have shown greater correction of the deformity and less loss of correction, allowing shorter arthrodeses2,7 to be performed compared to the use of constructs with hooks.7–9 On the other hand, other studies have found no differences between hybrid assemblies and those using only screws regarding their capacity to correct the deformity.10,11 The literature is not homogeneous regarding the incidence of complications using hybrid instrumentations or those employing only screws.3,9,10
The objective of this work was to evaluate and compare the radiographic results and complications of surgical treatment for severe idiopathic scoliosis (>75°) regarding the approach and instrumentation used (double approach, only through a posterior approach with hybrid instrumentation and only through a posterior approach with instrumentation using only screws).
Materials and methodsWe conducted a retrospective review of 69 patients suffering severe adolescent idiopathic scoliosis of Lenke types 1 and 212 who underwent surgical treatment. The inclusion criteria were: (1) angular value of the main curve greater than 75° and (2) minimum postoperative follow-up period of 2 years.
All patients were treated at our center between 2000 and 2011, by 3 types of surgical procedure: (1) anterior/posterior double approach (DA) consisting in release and anterior arthrodesis by thoracotomy or thoracoscopy, followed by posterior instrumented spinal fusion; (2) posterior approach with hybrid instrumentation (PH), defined as those cases in which the main corrective force was not applied through screws, but was generally applied through the use of pedicled screws at a caudal level, sublaminar wires at an apical level and hooks and/or screws at a cephalic level; (3) posterior approach with instrumentation consisting only of screws (PS). The distribution of patients into the different groups followed a time criterion, as these were 3 consecutive series of patients treated over a period of 12 years.
Patients with curves less than 75° or with a follow-up period less than 2 years were excluded from this study.
Radiographic assessmentThe preoperative radiographic assessment included posteroanterior and lateral radiographs of the entire spine whilst standing in all cases, along with tilt tests performed in the supine position on the radiographic table. Postoperative radiographs consisted of posteroanterior and lateral images of the entire column in the immediate postoperative period and at 2 years after surgery. Radiographic analysis included measurement of the Cobb angle of the main curve (from the superior plate of the upper limit vertebra to the lower plate of the lower limit vertebra) and identification of the type of curve according to the Lenke classification,12 their flexibility in tilt tests, and the value of the Cobb angle in the immediate postoperative period and at 2 years after surgery. On the lateral radiograph, overall kyphosis was measured from the superior T2 endplate to the inferior T12 endplate. Lumbar lordosis was measured from the superior T12 endplate to the superior S1 endplate.
Surgical procedureIn the DA group (n=24) we performed release and anterior arthrodesis of the main curve by thoracotomy or thoracoscopy, with complete resection of the discs and vertebral endplates and placement of an autograft from the resected rib and allograft from the tissue bank, followed by an instrumented posterior vertebral fusion with a hybrid system. All double approach procedures were performed in 2 stages, with a period of around 1 or 2 weeks between the anterior and posterior approaches. Temporary traction with cranial halo was only used between the 2 surgical stages in 3 of the 24 cases.
In the PH group (n=20) we performed an instrumented posterior vertebral fusion using pedicled screws, hooks and sublaminar wires. This group was different in that the main corrective force was not applied by pedicled screws, but rather by sublaminar wires in the concave side at the apex of the deformity. All screws were placed using the freehand technique.13
In the PS group (n=25) we performed an instrumented posterior vertebral fusion using pedicled screws exclusively.
In all 3 study groups, during the later stage we performed spacious lower facetectomies in all levels to be fused prior to implant placement, and in certain patients we also carried out posterior V-shaped Smith-Petersen osteotomies or costoplasties of the convex side, so as to obtain greater release and flexibility of the spine.
We used electrophysiological monitoring of the spinal cord through motor and sensory evoked potentials and electromyography in all patients. Those screws with a threshold lower than 6mA were removed to palpate the pedicle channel, and reimplanted if this was satisfactory. Cases where the pedicle wall broke were left without a screw.
In addition to the radiographic parameters, we recorded demographic variables, levels of arthrodesis, surgery time (except in the DA group) and complications.
The statistical analysis was performed using the software package SPSS 11.0, applying the Kruskal–Wallis test for nonparametric variables. Statistical significance was established for values of P<.05.
ResultsA total of 69 patients were included in this study. The DA group included 24 patients with a mean age of 13.8 years (CI: 12.7 to 14.8) at the time of surgery. Of these, 20 patients presented Lenke type 1 curves, whilst the other 4 presented type 2 curves. The anterior approach was performed by thoracotomy in 17 patients and by thoracoscopy in 7. The PH group consisted of 20 patients with a mean age of 14 years (CI: 13.1 to 14.9). Of these, 18 patients presented a Lenke type 1 pattern and 2 patients presented a type 2 pattern. The PS group included 25 patients with a mean age of 14.1 years (CI: 13.6 to 14.6), of which 15 patients presented a Lenke type 1 curve and 10 patients a type 2 curve.
Apical Smith-Petersen osteotomies were performed in 3 patients in the DA group, 5 patients in the PH group and 6 patients in the PS group (P=.591). The number of fused levels with posterior instrumentation was similar in the 3 groups: a mean total of 12.9 levels in the DA group, 12.6 in the PH group and 11.8 in the PS group (P>.05). The mean number of levels released through the anterior approach in the DA group was 6.5 levels. Statistically significant differences were observed in the number of costoplasties in the convexity performed in each group: costoplasty was performed in 9 patients in the DA group (representing 39% of the patients in this group), 12 patients in the PH group (60% of patients) and in only 5 patients in the PS group (20% of patients) (P=.023). The indication for costoplasty was the existence of severe angular humps with an unacceptable esthetic impact.
Surgical time was similar in the 2 isolated posterior approach groups, with a mean value of 248min (245min in the PS group and 252min in the PH group; P=.282). The surgical time was not recorded in the double approach group.
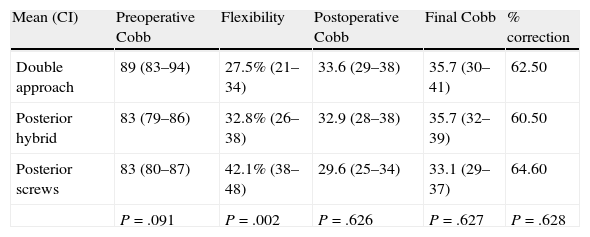
Radiographic resultsIn the DA group, the mean preoperative Cobb angle of the main curve was 89° (CI: 83.9 to 94), in the immediate postoperative period it was 34° (CI: 28.7 to 38.5) and at 2 years follow-up it was 36° (CI: 30.1 to 41.2) (Table 1). In the PH group, the mean preoperative Cobb angle was 83.10° (CI: 79.6 to 86.5), in the immediate postoperative period it was 32.9° (CI: 28.1 to 37.6) and at 2 years follow-up it was 35.7° (CI: 32.1 to 39.3). In the PS group, the mean preoperative Cobb angle of the main curve was 83.2° (CI: 79.8 to 86.7), in the immediate postoperative period it was 29.6° (CI: 25 to 34.2) and at 2 years follow-up it was 33.1° (CI: 28.8 to 37.5).
Coronal plane. Mean values (range in brackets) of the Cobb angle of the main curve preoperatively, in the immediate postoperative period and at the end of the follow-up period in the 3 study groups. The flexibility of the curves in the tilt tests and the percentage of correction obtained are also included.
| Mean (CI) | Preoperative Cobb | Flexibility | Postoperative Cobb | Final Cobb | % correction |
| Double approach | 89 (83–94) | 27.5% (21–34) | 33.6 (29–38) | 35.7 (30–41) | 62.50 |
| Posterior hybrid | 83 (79–86) | 32.8% (26–38) | 32.9 (28–38) | 35.7 (32–39) | 60.50 |
| Posterior screws | 83 (80–87) | 42.1% (38–48) | 29.6 (25–34) | 33.1 (29–37) | 64.60 |
| P=.091 | P=.002 | P=.626 | P=.627 | P=.628 |
The mean flexibility of the main curve of the deformity, as assessed by the tilt tests, was 27.5% (CI: 21 to 34) in the DA group, 32.8% (CI: 26.7 to 38.9) in the PH group and 43.1% (CI: 38.1 to 48) in the PS group.
The correction obtained at the end of the 2 years follow-up period relative to the preoperative value of the deformity, expressed as a percentage, was 62.5% in the DA group, 60.5% in the PH group and 64.6% in the PS group.
The differences observed in the value of the deformity between the 3 study groups were not statistically significant in the preoperative period (P=.091), immediate postoperative (P=.415) and at 2 years follow-up (P=.492) (Fig. 1). Similarly, differences in the percentage of correction obtained at the end of the follow-up period in each group were not statistically significant (P=.628). In contrast, statistically significant differences (P=.002) were observed in the flexibility of the curves, being significantly higher in the PS group.
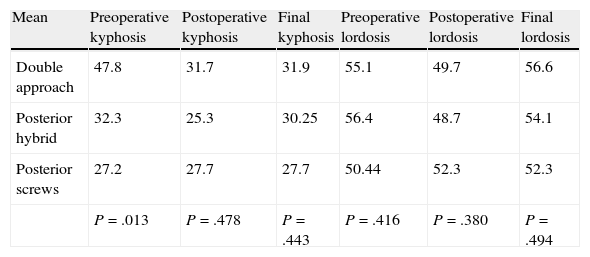
In the analysis of the sagittal plane (Table 2): in the DA group, the mean preoperative overall kyphosis was 47.8° (CI: 34.9 to 60), in the immediate postoperative period it was 31.7° (CI: 25.7 to 37.7), and at 2 years follow-up it was 31.9° (CI: 25.1 to 38.7). In the PH group, the mean preoperative overall kyphosis was 32.3° (CI: 25.7 to 38.8), in the immediate postoperative period it was 25.3° (CI: 21.8 to 28.8) and at 2 years follow-up it was 30.2° (CI: 26.9 to 33.5). In the PS group, the mean preoperative overall kyphosis was 27.2° (CI: 22.4 to 32), in the immediate postoperative period it was 27.7° (CI: 24.1 to 31.2) and at 2 years follow-up it was 27.7° (CI: 24 to 32).
Sagittal plane. Mean values (range in brackets) of thoracic kyphosis and lumbar lordosis preoperatively, in the immediate postoperative period and at the end of the follow-up period.
| Mean | Preoperative kyphosis | Postoperative kyphosis | Final kyphosis | Preoperative lordosis | Postoperative lordosis | Final lordosis |
| Double approach | 47.8 | 31.7 | 31.9 | 55.1 | 49.7 | 56.6 |
| Posterior hybrid | 32.3 | 25.3 | 30.25 | 56.4 | 48.7 | 54.1 |
| Posterior screws | 27.2 | 27.7 | 27.7 | 50.44 | 52.3 | 52.3 |
| P=.013 | P=.478 | P=.443 | P=.416 | P=.380 | P=.494 |
The differences observed between groups regarding the value of preoperative kyphosis were statistically significant (P=.013). No significant differences were observed in the value of kyphosis between groups in the immediate postoperative period or at 2 years follow-up. As for correction of kyphosis, we observed that modification of kyphosis after surgery was significantly higher in the DA group than in the PH and PS groups (P=.012).
In the DA group, the mean value of preoperative lordosis was 55.1° (CI: 49.1 to 61), in the immediate postoperative period it was 49.7° (CI: 46.2 to 53.3), and at 2 years follow-up it was 56.6° (CI: 52.4 to 60.8). In the PH group, the mean value of preoperative lordosis was 56.4° (CI: 51.4 to 61.4), in the immediate postoperative period it was 48.7° (CI: 43.6 to 53.7) and at 2 years follow-up it was 54.1° (CI: 48.3 to 59.9). In the PS group, the mean value of preoperative lordosis was 50.4° (CI: 44.1 to 56.7), in the immediate postoperative period it was 52.3° (CI: 46.4 to 58.2) and at 2 years follow-up it was 52.3° (CI: 46.4 to 58.2). No significant differences in the value of lordosis were observed between the 3 study groups at the different periods.
ComplicationsThe rate of complications (Fig. 2) related to the surgical procedure was different in each group. Complications occurred in 20.8% of patients in the DA group (n=5), 10% of patients in the PH (n=2) group and 20% of patients in the PS group (n=5). In the DA group there were 2 cases of pneumothorax which required placement of chest tubes, 1 case of chylothorax in the immediate postoperative period, 1 patient who developed crankshaft phenomenon and 1 case of implant mobilization. In the PH group there were 2 cases of pneumothorax which were resolved by placement of chest tubes. In the PS group there were complications in 5 cases: 1 case of excessive bleeding, 1 case of implant mobilization and 3 cases of changes in the neurophysiological monitoring of the spinal cord; 2 of which were fully resolved upon removal of the last implant placed (apex screw in concavity) and in 1 of them there was a temporary, incomplete neurological deficit.
Therefore, the lowest complication rate was obtained in the PH group. Despite not being statistically significant (P=.584), possibly due to the sample size, this difference in complications does have particular clinical relevance.
DiscussionThe treatment of idiopathic scoliosis has undergone a considerable evolution since the introduction of the Harrington system. The arrival of the Cotrel-Dubousset system (C-D) popularized the concept of segmental fixation with multiple points of attachment, allowing better results than with the Harrington bar,14 improving the rates of correction of the curves and preserving a normal sagittal profile. The improvement in the corrections obtained, together with the maintenance over time of these corrections, as well as the low frequency of pseudoarthrosis (or nonunion) and low incidence of neurological complications, helped to establish the C-D system as the gold standard for many years.2,14,15
Despite the improvements offered by the introduction of the C-D system, there was a perception of a limited capacity to correct severe and rigid curves. The introduction and application of lumbar pedicle screws made it possible to achieve a greater bone anchorage of the implants in order to allow greater correction of deformity; however, hooks and sublaminar wires were still being used at the thoracic level. Anterior releases began to be used in an attempt to improve the flexibility of the curves and enable anterior arthrodesis of the spine. These were initially performed by thoracotomy and subsequently by thoracoscopy.16,17 Unfortunately, these anterior release procedures entail an increase in surgery and hospitalization time, higher costs and a negative impact on lung function.1,2
Despite the good results registered with pedicle screws in the lumbar spine, the implantation of screws at the level of the thoracic spine was slow, due to safety problems often caused by extrapedicular placement. At present, most surgeons are able to obtain very good results in the placement of pedicle screws in the thoracic spine using the freehand technique with a minimum amount of training, since, in spite of the fact that the rate of extrapedicular placement can reach 25%, very few patients present neurological complications.18
In this work, we aim to evaluate the radiographic results and complications derived from the surgical treatment of patients with severe adolescent idiopathic scoliosis (Cobb angle greater than 75°), comparing the results of 3 surgical strategies: DA, PH and PS. We did not observe statistically significant differences among the 3 groups in terms of the angles measured before and after surgery or the percentages of correction registered. Correction in the DA group was 60%, in the PH group it was 57%, and in the PS group it was 60% (Fig. 3).
Representative figure of 3 patients with severe idiopathic scoliosis operated by 3 different strategies. The patient on the left was operated by a double approach consisting of release and anterior arthrodesis by thoracolumbotomy and instrumented posterior arthrodesis. The patient in the center was operated using hybrid instrumentation through an isolated posterior approach, and the patient on the right through an isolated posterior approach using only screws. Note the good results obtained in all 3 cases, regardless of the instrumentation and the approach employed.
Various studies have shown that there are no differences in the correction obtained through a DA or through an exclusively posterior approach using pedicle screws. Doobs et al.1 analyzed the results of DA and isolated posterior approach with pedicle screws in patients with idiopathic scoliosis of over 90°. They did not observe significant differences in angular values, flexibility or the correction obtained in both groups, nor in the rate of complications. In contrast, a negative effect on lung function was noted among patients who underwent anterior release. Luhmann et al.2 analyzed the results of treatment using a double approach or an isolated posterior approach in curves between 70° and 100° and observed greater correction in the coronal plane in the DA group compared to the PH instrumentation. Nevertheless, they found no differences when PS assemblies were used. Similar results were reported by Kuklo et al.3 and even in patients suffering adult scoliosis.4
Another source of controversy is the comparison of results between PH and PS through an isolated posterior approach. In our study, the results revealed no significant differences, showing a lower incidence of complications with the PH option. Different publications7–9 have reported better results using PS instrumentation, compared with PH. In a total of 66 patients with severe neuromuscular scoliosis, Mattila et al.7 reported greater correction, shorter surgical time and less bleeding using PS instrumentation. In idiopathic scoliosis over 80°, Di Silvestre et al.8 reported greater correction and less postoperative loss of the correction obtained when using PS assemblies compared to PH. On the other hand, the incidence of complications associated with surgery was significantly higher in the PS group (44% vs 25%). Kim et al.9 and Cheng et al.10 also obtained better results with pedicle screws than with hybrid assemblies, but they found no difference in the complication rate.
Nevertheless, certain publications have reported no differences between PH and PS regarding their ability to correct thoracic curves. Vora et al.11 and Crawford et al.19 did not observe better results with PS assemblies, although they did describe better correction in the sagittal plane using PH, with less lordosing effect on the thoracic spine.
One of the obstacles preventing the widespread use of pedicle screws in the thoracic spine was the incidence of complications associated with their malposition, especially by less experienced surgeons. Various series20,21 reported an incidence of malposition of pedicle screws of approximately 11%, which increased to 15–25% when analyzed systematically with CT. Other complications include loss of correction, intraoperative fracture of the pedicles, dural injury and neurological injury.
One of the drawbacks of the double approach through thoracotomy or thoracoscopy is the negative effect on lung function.5,6,22,23 Gitelman et al.22 observed a reduction in forced vital capacity and forced expiratory volume in the first second compared to the theoretical value when the chest was opened, either by thoracotomy or by thoracoscopy. In contrast, the group undergoing isolated posterior vertebral arthrodesis registered an improvement of respiratory parameters. This negative effect of thoracotomy can be mitigated using thoracoscopy to carry out the release and anterior arthrodesis.23 Some authors even question the efficacy of the anterior approach to obtain greater flexibility of the thoracic spine.24
In our study, the incidence of complications was 2 times greater using a double approach (DA) or an isolated posterior approach using only screws (PS) than using hybrid instrumentation through a posterior approach (PH). Although not statistically significant due to the small number of cases, this difference was of particular clinical relevance.
According to the results of our work, in this population group, which often suffers a restrictive lung function pattern, and since no differences were observed regarding the ability to correct scoliosis, the isolated posterior approach has the advantage of providing the same correction as the combined approach, preventing respiratory complications associated with the opening of the chest. Therefore, we could say that the combined approach is no longer the gold standard for the treatment of severe deformities.
The PH can offer similar results to PS assemblies, with a lower complication rate and lower costs. Our recommendation is that hooks and sublaminar wires are included among the resources available to spinal surgeons and also to avoid a fixation with placing pedicle screws in the thoracic spine when there are doubts regarding their intrapedicular location, especially in the concave region of the apex, since that is the most likely position to produce an alteration of spinal cord function. Faced with uncertainty regarding the correct location of intrapedicular screws, we prefer to replace them with hooks or sublaminar wires, as their correction power is similar.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sánchez-Márquez JM, Sánchez Pérez-Grueso FJ, Pérez Martín-Buitrago M, Fernández-Baíllo N, García-Fernández A, Quintáns-Rodríguez J. Escoliosis idiopáticas graves. ¿El abordaje y la instrumentación modifican los resultados?. Rev Esp Cir Ortop Traumatol. 2014;58:144–151.