To determine the risk factors associated with prosthetic dislocation and simulate a finite element model to determine the safe range of movement of various inclination and anteversion cup positions.
Material and methodsRetrospective case control study with 46 dislocated patients from 1994 to 2011. Control group: 83 randomly selected patients. Dislocation risk factors described in the literature were collected. A prosthetic model was simulated using finite elements with 28, 32, 36mm heads, and a 52mm cup. Acetabular position was 25°, 40°, and 60° tilt and with 0°, 15° and 25° anteversion. In extension of 0° and flexion of 90°, internal and external rotation was applied to analyze the range of movement, maximum resisting moment, and stress distribution in the acetabulum to impingement and dislocation.
ResultsThere was greater dislocation in older patients (p=0.002). Higher dislocation in fractures than in osteoarthritis (p=0.001). Less anteversion in dislocated patients (p=0.043). Longer femoral neck in dislocated patients (p=0.002). Finite element model: lower dislocation when there is more anteversion, tilt and bigger femoral heads.
Discussion-conclusionsAdvanced age and fractures are the major risk factors for dislocation. “Safe zone” of movement for dislocation avoidance is 40–60° tilt and 15–25° anteversion. Both the defect and excess of soft tissue tension predispose to dislocation. Bigger femoral heads are more stable.
Determinar los factores de riesgo asociados a la luxación protésica y simular un modelo mediante elementos finitos que determine los arcos de movimiento seguros en cada angulación y anteversión del cotilo.
Material y métodosCasos-control retrospectivo con 46 pacientes luxados desde 1994 hasta 2011. Grupo control: 83 pacientes elegidos de forma aleatoria. Se recogieron los factores de riesgo de luxación descritos en la literatura. Se simuló un modelo protésico mediante elementos finitos con cabezas de 28, 32, 36mm y cotilo de 52mm. Posición acetabular de 25°, 40° y 60° de inclinación y 0°, 15° y 25° de anteversión. Para cada combinación se estudió la flexión de 90° y la extensión de 0° aplicando rotación interna y externa midiendo el rango de movimiento y el momento resistente hasta el choque-luxación y la distribución de tensiones en la superficie del cotilo.
ResultadosMayor edad en luxados (p=0,002). Mayor luxación en fracturas respecto artrosis (p<0,001). Menor anteversión en luxados (p=0,043). Mayor longitud de cuello femoral en luxados (p=0,002). Simulación de finitos: menor luxación cuanto mayor inclinación, anteversión y diámetro de cabeza femoral.
Discusión-conclusionesLa edad avanzada y la fractura son los principales factores favorecedores de la luxación. El área de seguridad libre de luxación comprende 40°-60° de inclinación y 15°-25° de anteversión. Tanto el defecto como el exceso de tensión de las partes blandas predisponen a la luxación. Las cabezas de mayor tamaño son más estables.
Total hip arthroplasty (THA) is a very frequent procedure in Traumatology and Orthopedic Surgery Services, and although its effectiveness is very high, it is not without complications such as aseptic loosening, dislocations, infections and periprosthetic fractures.
Despite the advances in prosthetic techniques and models, dislocation is still the second most common complication in total hip arthroplasties, following aseptic loosening. It appears in 0.3–10% of primary hip arthroplasties and in up to 28% of revision arthroplasties.1
There are various classifications of THA dislocation; according to the time: early (<3 months) and belated (>3 months); according to their number: simple or recurrent; according to their direction: anterior (clinical observation of the affected limb in external rotation and extension) and posterior (lower limb in internal rotation and flexion); according to the mechanism of the lesion: traumatic or spontaneous; according to the etiology, following the Dorr classification,2 which is important as knowledge of the cause of dislocation will help to decide the therapeutic attitude (positional: no radiographic alteration of components without soft tissue imbalance [10%]; malposition of components [33%]; imbalance of soft tissues: musculature, major trochanter, offset, [33%]; combination of II and III).
On the other hand, the risk factors considered associated to a greater probability of prosthetic dislocation have been extensively studied; factors relating to the patient such as age, gender, cognitive or neuromuscular alterations, initial diagnosis, prior surgery; factors related to the surgical procedure, such as approach routes, characteristics of the components, pre- and postoperative radiographic measurements. However, there is still significant controversy surrounding many of them.
Considering the high incidence of dislocation in total hip arthroplasties and the lack of consensus in relation to some of the risk factors that favor it, this clinical–computational research work is designed with the following objectives: clinical: to determine the risk factors associated to prosthetic dislocation and categorize them by order of relevance, and computational: to simulate a prosthetic model with different sizes of components and their maximum ranges of movement before the impingement between components and dislocation takes place, in addition to correlating the computational with the clinical findings to determine the safe ranges of movement in each angulation and anteversion of the cup.
Materials and methodsClinical studyPopulation and sampleWe collected the episodes of dislocation of the THA diagnosed and treated at our center since 1994 until 2011. A total of 2227 arthroplasties were implanted in this period, of which 1338 were cemented, Exeter-Müller model, and 889 were uncemented, Zweymüller model, which as of 2004 was called SL-Plus.
A total of 46 patients, 35 cases with Exeter-Müller and 11 with Zweymüller/SL-Plus, suffered a prosthetic dislocation, so they comprised the group of cases.
The inclusion criteria were arthroplasties that had been implanted at our center and which corresponded to the previously described models. These criteria were selected in order to have all the data regarding the cause that determined the need for an arthroplasty, as well as surgical protocol, clinical history and radiographic studies.
The control group was formed by 83 patients (39 cemented THA and 44 uncemented) with the same models of arthroplasty, with ages matching those of our group of cases, who were randomly selected and who had undergone implantation of a total hip arthroplasty at our center with a matching history to that of the case group.
Variables collectedWe collected the risk factors for dislocation described in the literature for all the patients included in the study.
- 1.
Factors related to the patient: gender, age, underlying diagnosis (categorized as arthrosis, fracture, pathological fracture, rheumatoid arthritis, and avascular necrosis), prior hip surgery, neuromuscular dysfunction (Parkinson, Alzheimer), non-fulfillment of all the prophylactic anti-dislocation rules, cognitive dysfunction, abuse of alcohol and drugs.
- 2.
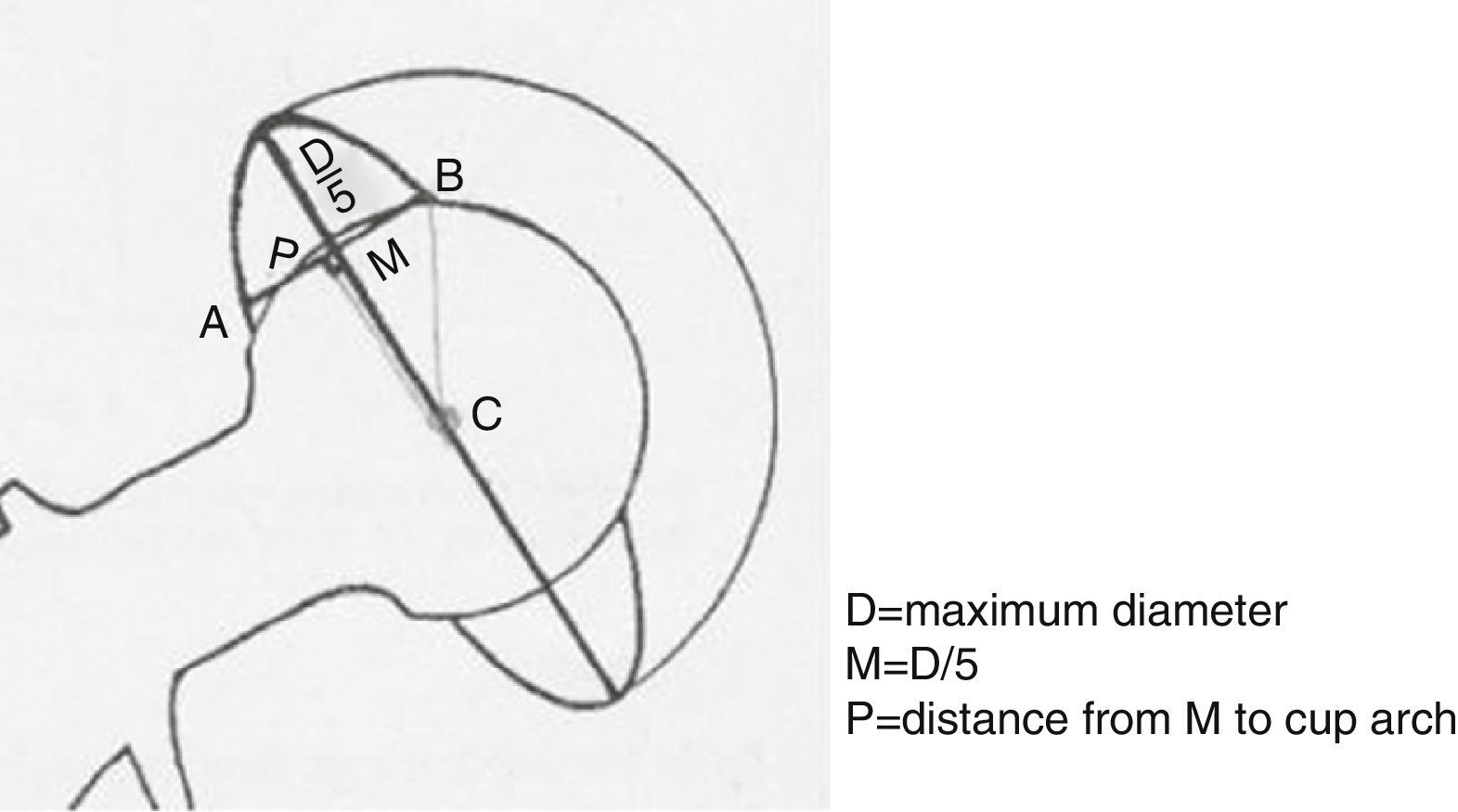
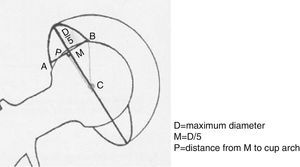
Factors related to the surgical technique: approach route (all the patients were intervened through a Hardinge-Bauer anterolateral approach), orientation of the components as measured on anteroposterior pelvic radiographs (angle of abduction or inclination/tilt and angle of version of the cup according to the Riten Pradhan3 method: anteversion=arcsen [p/0.4×D], [Fig. 1]), tension of the soft parts (pre- and postoperative Voss effect, pre- and postoperative offset, pre- and postoperative length of the femoral neck), experience of the surgeon (categorized into 2 groups as surgeons with more or less than 10 years of experience) and infection (both of the surgical wound and deep).
- 3.
Factors related to the design of the implant: size of the head (all the implants had a femoral head size of 28mm, except for 1 single case in which the size was of 32mm), head–neck size ratio, head–acetabulum size ratio, design of the acetabular component.
All the patients who underwent THA received antibiotic prophylaxis with 1g cefazolin or 600mg dalacin phosphate (in case of allergy) during anesthetic induction and antithrombotic prophylaxis with low molecular weight heparin at least 12h before the surgical intervention.
We conducted a mean follow-up of 5 years of the patients in both groups, at the outpatient clinic of our center, in order to detect any possible complications.
Statistical analysisThe statistical data were processed with the software package SPSS (version 15.0; SPSS Inc, Chicago, IL, USA) and with a level of significance of P<.05.
Computational studyWe simulated a prosthetic model through the method of finite elements to study the effect of the diameter of the head of the prosthesis, the angle of inclination and anteversion in the impingement of the components and the posterior dislocation of the THA.
The head sizes considered for the study were 28, 32 and 36mm as these are the most frequently used in clinical practice. We used an outer diameter of the cup of 52mm in all the models as this is the minimum size required in most implants for 36mm heads.
The inclination and anteversion angles were established according to the Lewinnek4 safety area (inclination 40±10°, anteversion 15±10°) with inclination values of 25°, 40° and 60° and anteversion values of 0°, 15° and 25°.
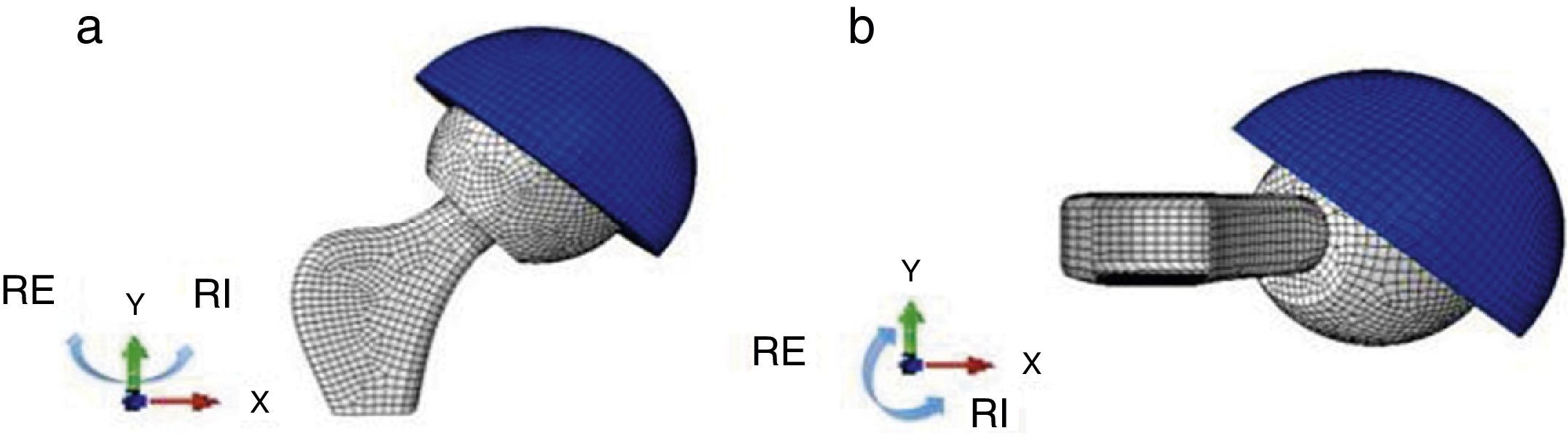
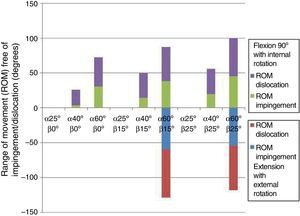
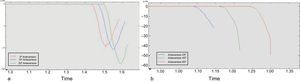
We studied 2 positions for each combination of the previous factors, flexion of 90°, equivalent to the patient sitting, and extension of 0°, equivalent to the patient standing. In each of them we analyzed the effect of the external and internal rotation until the impingement between the components and prosthetic dislocation took place. We considered that the maximum movement ranges in internal and external rotation of the hip were 40° and 60°, respectively, as described in the literature (Fig. 2).
The geometry and dimensions of the implant were obtained through the CT images of an Exeter prosthesis developed in Abaqus CAE v6.11 formed by two parts. The acetabulum was simulated as a deformable solid based on a surface of revolution. The head and stem were simulated as a normal rigid shell. In the case of the head it was designed as a surface of revolution and in the case of the stem as an extruded surface.
The acetabulum was rendered with 10164 C3D8R-type hexahedral elements and the head and the stem with 2900 triangular and quadrilateral elements, of R3D3 and R3D4 types, respectively.
Properties of material and non-linearity of the simulated problemThe acetabular component was simulated as ultra-high molecular weight polyethylene (UHMWPE) and assigned an elastic module of E=940MPa, a Poisson coefficient of ν=0.3 and a yield limit of 26.26MPa, thus simulating the plastic properties of polyethylene.5
Regarding the interaction properties we assigned the head and the neck as master surfaces and the internal hemisphere of the acetabulum and circular crown as the slave surfaces. We introduced an isotropic tangential mechanical behavior, with a friction coefficient of 0.038.6
We studied the range of movement (ROM) and the resistance momentum until the impingement and dislocation for each of the previous combinations, as well as the tension distribution in the surface of the cup.
ResultsThe incidence of THA dislocation in our sample was of 2.07%, with 2.62% in the case of cemented arthroplasties and 1.24% in the case of uncemented arthroplasties.
The dislocation was early (<3 months) in the majority of the cases (87%), with just 1 single case of belated dislocation (>5 years) and 5 cases of dislocations in the intermediate period.
Analysis of the risk factors associated to dislocation- 1.
Factors related to the patient:
- -
Gender: the analysis separating the sample into cemented and uncemented arthroplasties revealed statistically significant differences in the group of cemented arthroplasties (P<.001), with dislocation being more frequent among males.
- -
Age: the mean age at which the arthroplasties were implanted was 67 years, with statistically significant differences (P=.002) being observed with a higher mean age (71 years) in the group of dislocated patients, versus the non-dislocated (64 years).
- -
Underlying diagnosis: we observed statistically significant differences (P<.001) between the percentage of dislocation and the diagnosis that led to the implantation of the arthroplasty. Within the group of patients requiring a THA due to fracture, the percentage of dislocation was of 68% versus only 16% in the case of coxarthrosis. Likewise, the 5 patients with pathological fractures suffered dislocations, as did the only case of rheumatoid arthritis.
- -
Prior hip surgery: although no statistically significant differences were obtained (P=.095) the percentage of dislocation was higher among the group of patients who had undergone a prior surgery in the same hip before the implantation of the prosthesis.
- -
Neuromuscular dysfunction – cognitive dysfunction: the analysis of the relationship between neurological alterations and dislocation returned significant differences (P<.001), with dislocation being more frequent in the presence of neurological deterioration.
- -
Alcohol and drug abuse: the association between alcohol/drug abuse and prosthetic dislocation resulted significant (P=.019), with all patients who consumed these substances suffering dislocation.
- -
- 2.
Factors related to the surgical technique:
- (a)
Orientation of the components:
- -
Angle of abduction/inclination: no statistically significant differences were obtained. However, we observed that the mean value of the inclination angle in dislocated patients was partially smaller (38°) than in non-dislocated patients (40°).
- -
Angle of version: we found statistical significance (P=.043) in the relationship between the version angle of the cup and prosthetic dislocation. Those patients who suffered dislocation had a smaller mean cup version (11.54°), than patients who did not suffer dislocation (14.19°).
- -
- (b)
Tension of soft tissues:
- -
Voss effect: the relationship between dislocation and the postoperative Voss effect did not show statistically significant differences (P=.128), although we observed a negative Voss more frequently among dislocated patients.
- -
Offset: we observed statistical significance (P=.005) in the group of cemented arthroplasties, with a greater offset (59mm versus 55mm) in the patients who suffered dislocation.
- -
Length of the femoral neck: we observed a statistically significant difference (P=.002) in the fact that patients with longer femoral heads suffered postoperative prosthetic dislocation. The mean length of the femoral neck among non-dislocated patients was of 62.82mm, whilst that of dislocated patients was 66.67mm.
- -
- (c)
Experience of the surgeon: this factor showed no statistically significant differences (P=.128). However, it was worth noting that the percentage of surgeons with less experience was higher in the group of dislocated patients (28% versus 17%).
- (d)
Infection: all the infections that took place were a priori superficial, of the surgical wound (8/129). However, the statistical analysis revealed significant differences (P<.001), whereby all the patients with infection were in the group who suffered prosthetic dislocation.
- (e)
Factors related to the design of the implant:
- -
Size of the head: the only head with a size of 32mm did not suffer dislocation.
- -
Head–neck size ratio: no statistically significant differences were observed.
- -
Head–acetabulum size ratio: since all the heads were of 28mm, except for 1 which was of 32mm, we related the dislocation to the size of the cup. We did not obtain statistically significant differences.
- -
- (a)
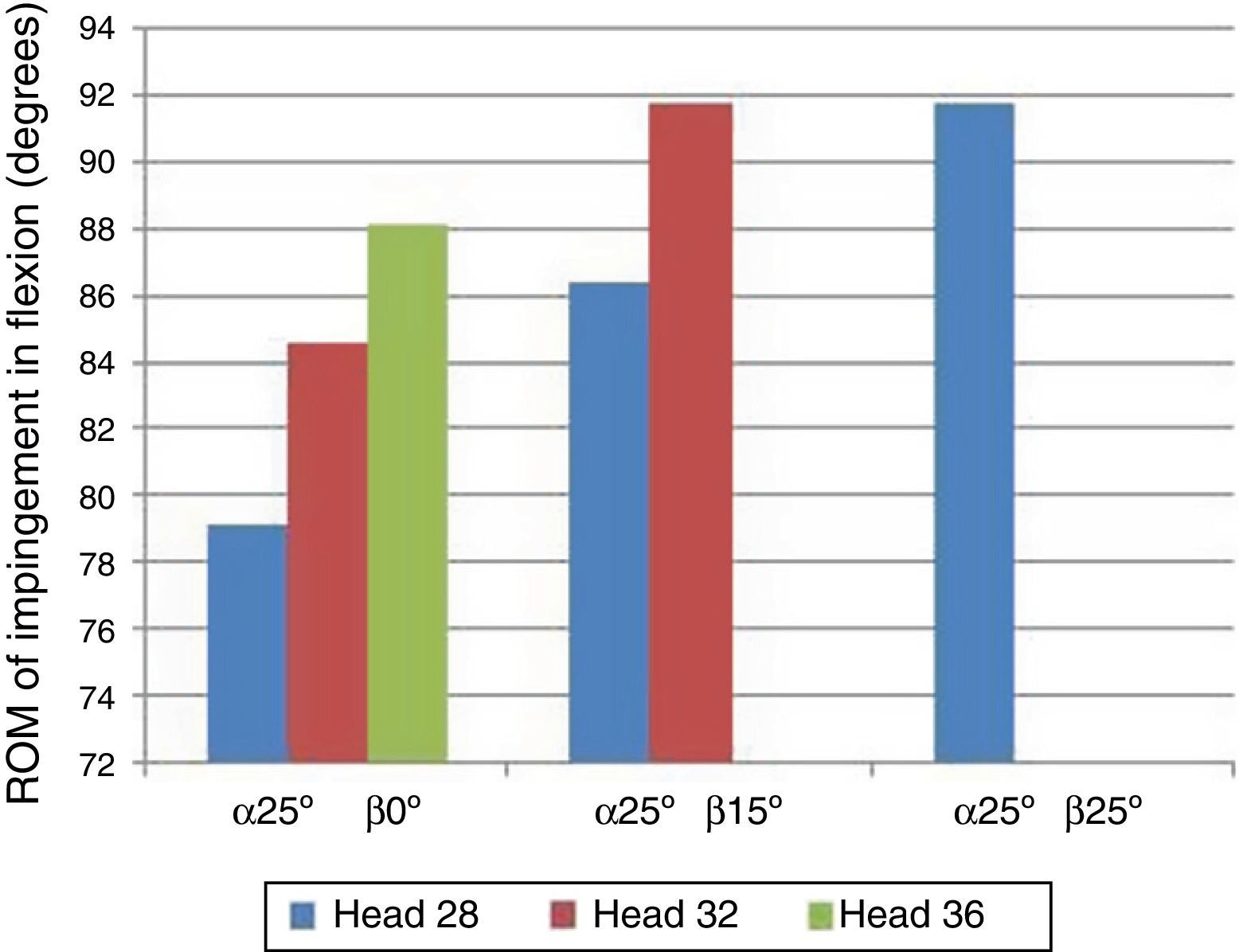
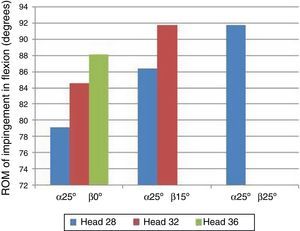
We observed that when the inclination (α) of the cup was of 25° regardless of the level of anteversion (β) there was an impingement between components before reaching a flexion of 90°, so it was no longer necessary to carry out the rotations. This happened with any anteversion in the heads of 28mm. However, for the head of 32mm it was only observed in anteversion of 0° and 15°, and with the head of 36mm only in anteversion of 0°.
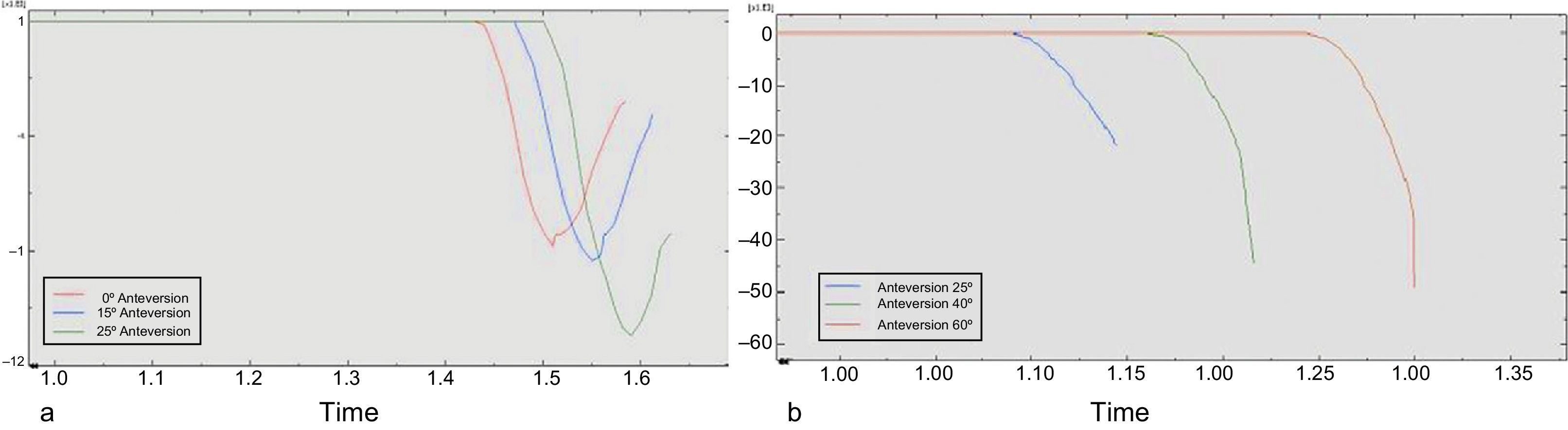
In addition, a progressively greater flexion took place until impingement as the diameter of the femoral head was increased on one side, and anteversion on the other (Fig. 3).
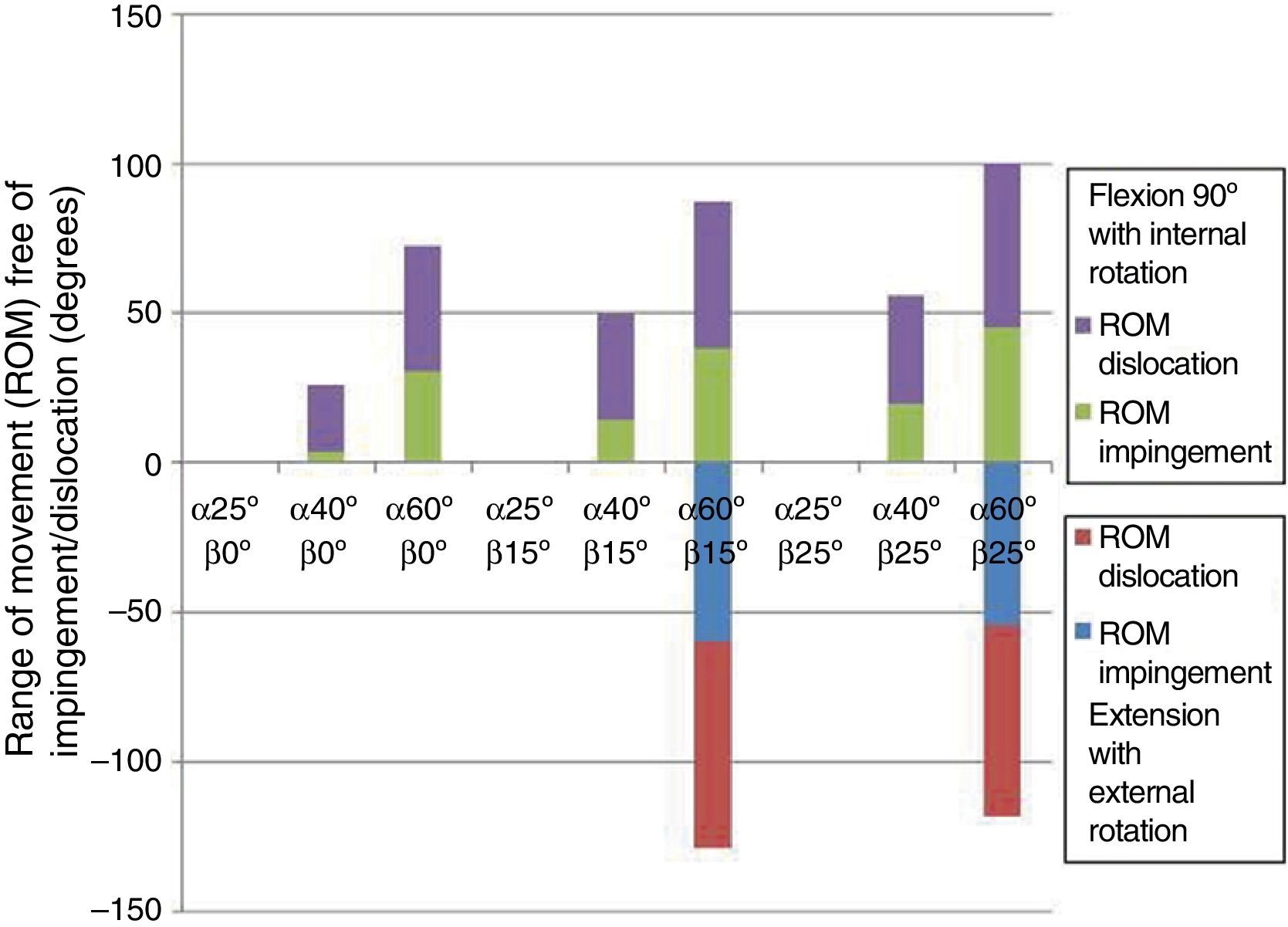
The analysis revealed 2 opposing positions which favored dislocation. On the one hand, the greater the inclination (α) and anteversion (β) the greater the risk of anterior dislocation in extension and external rotation. On the other hand, the lower the inclination (α) and the anteversion (β) the greater the risk of posterior dislocation in flexion and internal rotation (Fig. 4). The 28mm head was the only one that presented an anterior dislocation with the previously described characteristics, in addition to posterior dislocation, which also took place in the 32mm and 36mm heads.
The ROM of impingement and dislocation was proportional both to the degree of inclination (α) and anteversion (β) of the cup and to the major diameter of the femoral head, with dislocation being less frequent in the larger heads, i.e. taking place at more extreme degrees of rotation, practically at the limit of the movement capacity of the arthroplasty.
Regarding the ROM, we observed that this increased together with the diameter of the femoral head when considering the same cup position. The same relationship was found between the ROM and anteversion on the one hand and the ROM and inclination on the other. Considering a single size of femoral head and maintaining a constant inclination and anteversion, respectively, the ROM and the anteversion/inclination increased proportionally (Fig. 5).
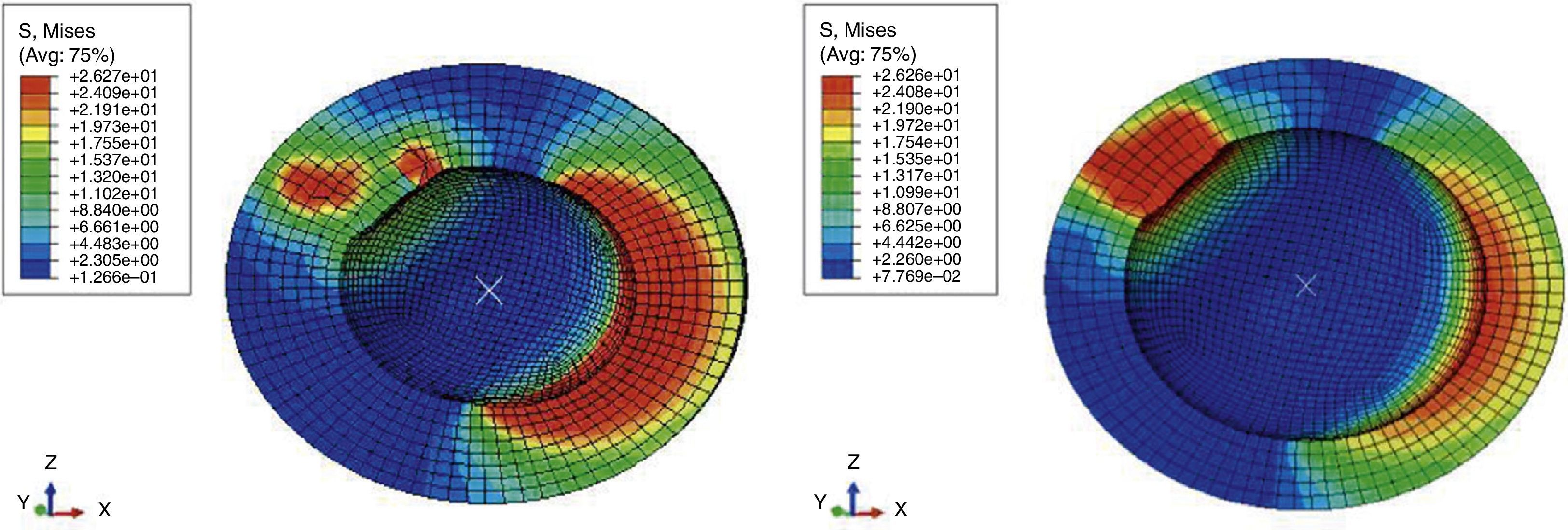
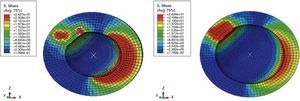
The tensions in the surface of the cup in the area of contact of the neck during the impingement and the dislocation were high regardless of the size of the head. However, in the area of dislocation of the femoral head (egress site) they were lower as the diameter of the head increased (Fig. 6).
DiscussionThe incidence of THA dislocation in the sample was of 2.07%, with 2.62% taking place in cemented arthroplasties and 1.24% in uncemented arthroplasties. The data published in this regard range between rates of 0.5% and 9.2%, as mentioned in previous reviews.1 This places our work in a good range within the literature. Regarding the incidence of dislocation according to cemented or uncemented prosthetic models, our results were very similar to those published in our country on low-friction cemented THA with an incidence of 2.97% (2.62%) and uncemented THA with 2.8% (1.24%).7
Our own findings, along with those reported by these publications regarding a lower rate of dislocation among uncemented arthroplasties are in contrast with the results obtained by Conroy et al.,8 who published a higher rate of dislocation in uncemented versus cemented cups with a relative risk of 1.59, especially if the uncemented cup was used with femoral heads with a diameter of less than 28mm. Although without data to support their hypothesis, these authors postulated that the orientation of cemented cups was more precise because the surgical technique allowed them to be better adapted whilst the cement polymerized, whereas uncemented cups sought their own adjustment within the acetabulum, which may not have coincided with the optimal position sought by the surgeon.
Dislocation was early (<3 months) in the majority of cases (87%), with only 1 case of belated dislocation (>5 years), in the group of uncemented arthroplasties, and 5 cases of dislocations in the intermediate period. The data published in the literature indicate that the majority of the dislocations take place within the first 3 months after the surgery, as was the case in our study. Approximately 50–70% of the dislocations took place between the first 5 weeks and 3 months after the intervention and more than three quarters of all the dislocations within the first year. In 26% of the cases, the first episode of dislocation took place 2 years after the operation, with this period extending more than 5 years in 0.8% of the patients.9
Some authors have proposed progressive wear of the polyethylene of the acetabular nucleus as the cause of the “belated” instability,10 but this is probably not the only reason, and we should add others, at least in a coadjutant role, such as a decrease in soft tissue tension and muscle tone and as well as the modifications in posture, coordination and balance experienced by patients with the passage of time, as mentioned by Fernández-Fairen et al.,11 in their review article of the bibliography published in this respect.
In the group of cemented arthroplasties we observed that dislocation was more frequent among males in a statistically significant manner. The scientific literature adds to the controversy on this issue. Studies such as that by Woo and Morrey12 report that the risk of dislocation among females is 2 times higher than among males. The same finding was reported by Kim et al.,13 with a risk of dislocation among females 2.5 times higher than that of males. On the other hand, Masaoka et al.14 found no differences between both genders.
The factors proposed as causative of a higher rate of dislocation among females are less strength and muscle tone, and a greater elasticity of soft tissues.15 This fact could explain the lack of correlation between the risk of prosthetic dislocation in the female gender in the case of revision arthroplasty. In this case, the involvement of muscle function following revision arthroplasty which is also present in the male gender makes the incidence of dislocation equal between the two genders.16
This study found statistically significant differences with higher mean age (71 years) in the group of dislocated patients versus the non-dislocated (64 years). The literature contains publications, such as those by Morrey17 and Masaoka et al.,14 that did not find a relationship between age and prosthetic dislocation. On the other hand, Ekelund et al.18 published that the risk of dislocation was multiplied by 2 in octogenarians. Likewise, Byström et al.19 published a risk of dislocation 4.5 times higher among those aged over 80 years, whilst Berry et al.20 published a relative risk of dislocation 1.3 times higher in patients aged over 70 years. Advanced age entails increased frailty, loss of muscle tone, inability to comply with anti-dislocation advice and an increased incidence of cognitive problems, all of which entail a higher risk of prosthetic dislocation, which leads us to consider whether age is an independent risk factor or a confusion bias.
Dislocation was more common among cases who had suffered fractures than coxarthrosis, in a statistically significant manner. Similar data have been published in the literature, with a rate of dislocation in THA due to fractures of 14% versus 4% in cases due to arthrosis.21 The 2 circumstances that could explain this are capsular hypertrophy observed in patients with coxarthrosis, which could act as stabilizer element for the hip, and the greater range of movement of the arthroplasty in patients with hip fractures compared to those with coxarthrosis.
Although no statistically significant differences were obtained, dislocation was more frequent in the group of patients who had undergone prior surgery in the same hip. There are some publications in this respect that place the rate of dislocation of the hips with previous surgery at double that of those that had not been intervened previously.22 This is probably due to the lassitude, scarring and other soft tissue lesions caused by the previous surgery.
Dislocation was more frequent when there was neurological impairment, with a significant difference, and also all those patients who consumed alcohol suffered prosthetic dislocation. This figure coincides with that observed by Woolson and Rahimtoola,23 who published an incidence of 12.7% dislocations among patients with a history of dementia, confusion and/or alcoholism versus 3% of patients who did not have a prior history of such alterations.
In our series we did not find statistically significant differences in the relationship between dislocation and the inclination angle of the cup. However, we did find them in the case of anteversion, with a lower value (11.54±6.05°) in dislocated cups than in non-dislocated cups (14.19±8.61°). Similar data were published by Nishii et al.,24 who reported that 181 hips without dislocation had an anteversion ≥20°, whilst 9 dislocated hips had an anteversion <20°.
Regarding the 2 opposing positions that were revealed as favoring dislocation, these were very similar to the findings of the clinical part of the study and the literature. As mentioned previously, on the one hand, the greater the inclination and anteversion, the higher the risk of anterior dislocation in extension and external rotation. These same findings were published by Scifert et al.,25 who considered that an increase of anteversion and inclination improved prosthetic stability in terms of posterior dislocation, although they predisposed toward anterior dislocation and wear. A more recent study by Kluess et al.5 made the same observation following a simulation of total hip arthroplasty through finite elements. As shown by our simulation, the cup should be placed at an inclination of between 40° and 60° and an anteversion of between 15° and 25°.
The findings obtained in this study related a higher soft tissue tension with a higher risk of dislocation, which a priori goes against the widely extended concept that patients with a loss of femoral offset have more unstable hips.26 However, Ameneiro et al.27 published that the offset of dislocated patients was slightly higher than that of non-dislocated patients (42.2mm versus 40.7mm) and the same was true about the length of the femoral neck.
It was worth noting that there was a higher percentage of surgeons with less experience in the group of dislocated patients. This factor has been confirmed by a recent systematic review.28
The statistical analysis revealed significant differences, with all the patients with infection being part of the group who suffered prosthetic dislocation. The joint collection could have produced an increase of the hydrostatic pressure that could have distracted the joint, making it more vulnerable to dislocation.
The ROM of “impingement” and dislocation was proportional to a greater diameter of the femoral head, with dislocation being less frequent among larger heads, i.e. taking place in more extreme degrees of rotation. In relation to the diameter of the head, many publications have supported a stability of larger heads.29 In this respect, it is worth noting the work with finite elements by Scifert et al.25 The importance of a greater diameter of the femoral head in terms of prosthetic stability can also be observed when analyzing the resistance momentum, which increased together with the diameter of the femoral head. A high resistance momentum involves greater stability and greater resistance to dislocation. These findings closely match those published by other authors.5,25
Regarding the distribution of tensions in the surface of the cup during impingement and dislocation, we observed that, regardless of the size of the head, all the tensions were high in the area of neck impingement. However, in the area of dislocation of the femoral head (egress site) they were lower as the diameter of the head increased. These findings suggest that larger heads could have less polyethylene wear, a factor that is associated to instability due to the greater penetration of the femoral head into the acetabular component, favoring impingement of the prosthetic neck and due to the formation of granulomas from polyethylene particles that would condition a loosening and even migration of the acetabular component.30
ConclusionsAdvanced age, cognitive deterioration and prior fracture are the main factors favoring prosthetic dislocation. Implantation of the cup with an anteversion under 10–15° is most important factor of the surgical technique in determining the onset of prosthetic dislocation. The methodology with finite elements allows us to study the stability of a total hip arthroplasty, being especially useful to evaluate the resistance momentum. The safety area free of dislocation entails a position of the cup with an inclination between 40° and 60° and an anteversion of between 15° and 25°. Restoring soft tissue tension is crucial in obtaining a stable arthroplasty, as both a lack and an excess of tension will predispose toward dislocation. Larger heads were more stable, as long as adequate proportions regarding the size of the neck and cup were maintained. Although no statistically significant differences were obtained, greater surgeon experience represented a progressively smaller risk of prosthetic dislocation.
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ezquerra-Herrando L, Seral-García B, Quilez MP, Pérez MA, Albareda-Albareda J. Inestabilidad de la artroplastia total de cadera: estudio clínico y computacional de sus factores de riesgo. Rev Esp Cir Ortop Traumatol. 2015;59:287–294.