Infection misdiagnosis is common in older adults since infections may present differently than in the general population1 COVID-19 is typically signalled by three symptoms: fever, cough and dyspnoea and is particularly fatal for older adults.2,3 Atypical symptoms recognition in these extremely vulnerable populations is critical for early detection, screening and intervention. However, atypical symptoms in older adults are not well established. We report clinical characteristics and presenting symptoms of COVID-19 in advanced age patients attended in a specialized geriatric hospital in Madrid, a city where the SARS-CoV-2 pandemic was particularly bad. The study protocol was approved by the Ethics Committee, under the ID: PI-4131.
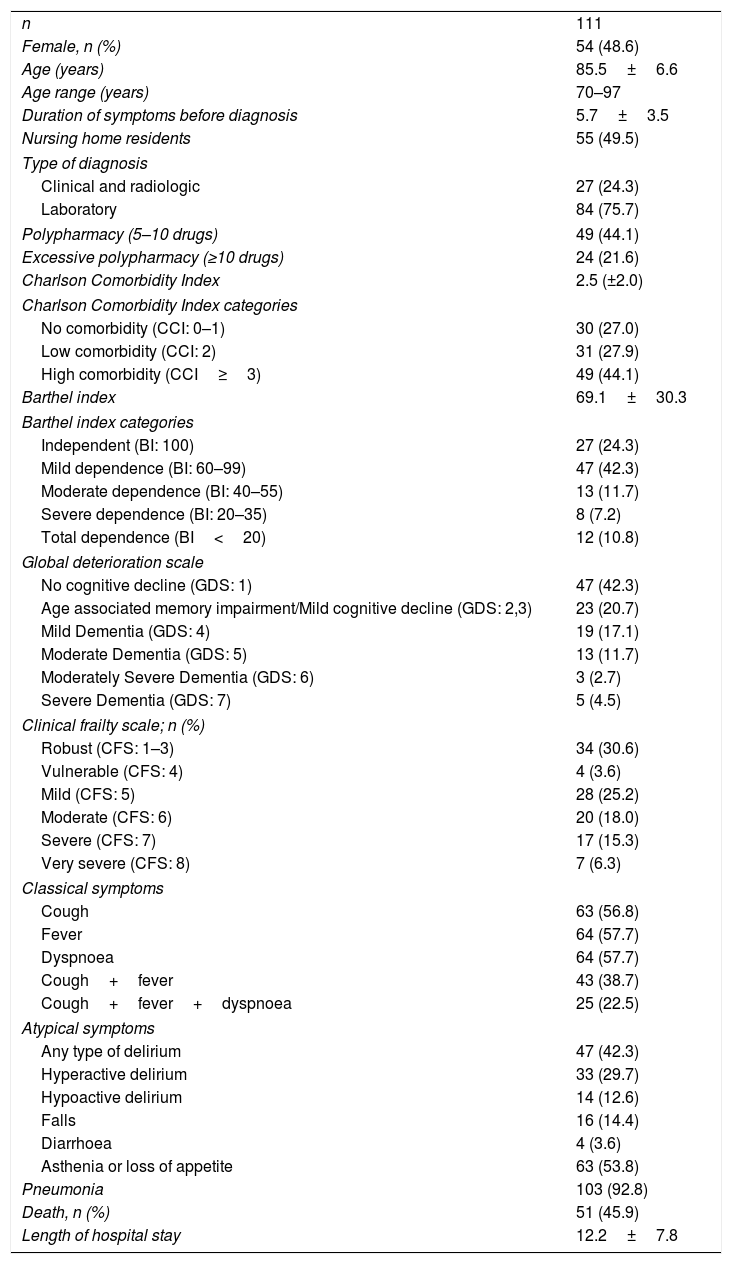
Between March 20 and April 30, 2020, we attended 111 patients with probable or definitive COVID-19 diagnosis.4Table 1 shows demographic and clinical characteristics, including geriatric assessments. Mean age (85.5±6.6y) is higher than in studies, which defined COVID-19 clinical characteristics.5 Many patients were frail with significant co-morbidities. However, a high proportion had no or only mild functional or cognitive impairment (Table 1). 47 patients (42.3%) did not present fever and 27 (24.3%) neither fever nor cough. Amongst atypical symptoms stands out the delirium (hyperactive or hypoactive) assessed by Confusion Assessment Method (CAM),6 present in more than 40% of patients, and high prevalence of falls as presenting symptom (14.4%). Fever absence was significantly more frequent in patients with falls compared to patients with other presenting symptoms (68.5%, vs. 37.9%; p=0.021). Nearly 93% of patients had radiographically confirmed pneumonia.
Demographic characteristics and symptoms at admission.
| n | 111 |
| Female, n (%) | 54 (48.6) |
| Age (years) | 85.5±6.6 |
| Age range (years) | 70–97 |
| Duration of symptoms before diagnosis | 5.7±3.5 |
| Nursing home residents | 55 (49.5) |
| Type of diagnosis | |
| Clinical and radiologic | 27 (24.3) |
| Laboratory | 84 (75.7) |
| Polypharmacy (5–10 drugs) | 49 (44.1) |
| Excessive polypharmacy (≥10 drugs) | 24 (21.6) |
| Charlson Comorbidity Index | 2.5 (±2.0) |
| Charlson Comorbidity Index categories | |
| No comorbidity (CCI: 0–1) | 30 (27.0) |
| Low comorbidity (CCI: 2) | 31 (27.9) |
| High comorbidity (CCI≥3) | 49 (44.1) |
| Barthel index | 69.1±30.3 |
| Barthel index categories | |
| Independent (BI: 100) | 27 (24.3) |
| Mild dependence (BI: 60–99) | 47 (42.3) |
| Moderate dependence (BI: 40–55) | 13 (11.7) |
| Severe dependence (BI: 20–35) | 8 (7.2) |
| Total dependence (BI<20) | 12 (10.8) |
| Global deterioration scale | |
| No cognitive decline (GDS: 1) | 47 (42.3) |
| Age associated memory impairment/Mild cognitive decline (GDS: 2,3) | 23 (20.7) |
| Mild Dementia (GDS: 4) | 19 (17.1) |
| Moderate Dementia (GDS: 5) | 13 (11.7) |
| Moderately Severe Dementia (GDS: 6) | 3 (2.7) |
| Severe Dementia (GDS: 7) | 5 (4.5) |
| Clinical frailty scale; n (%) | |
| Robust (CFS: 1–3) | 34 (30.6) |
| Vulnerable (CFS: 4) | 4 (3.6) |
| Mild (CFS: 5) | 28 (25.2) |
| Moderate (CFS: 6) | 20 (18.0) |
| Severe (CFS: 7) | 17 (15.3) |
| Very severe (CFS: 8) | 7 (6.3) |
| Classical symptoms | |
| Cough | 63 (56.8) |
| Fever | 64 (57.7) |
| Dyspnoea | 64 (57.7) |
| Cough+fever | 43 (38.7) |
| Cough+fever+dyspnoea | 25 (22.5) |
| Atypical symptoms | |
| Any type of delirium | 47 (42.3) |
| Hyperactive delirium | 33 (29.7) |
| Hypoactive delirium | 14 (12.6) |
| Falls | 16 (14.4) |
| Diarrhoea | 4 (3.6) |
| Asthenia or loss of appetite | 63 (53.8) |
| Pneumonia | 103 (92.8) |
| Death, n (%) | 51 (45.9) |
| Length of hospital stay | 12.2±7.8 |
BI: Barthel index. CCI: Charlson Comorbidity Index. CFS: Clinical Frailty Scale. GDS: Global Deterioration Scale. Longitudinal data are shown as mean (±standard deviation).
Global in-hospital mortality was 45.9%. Patients with delirium had nearly double in-hospital death risk compared to those with other presenting symptoms (61.7% vs. 34.4%; p=0.004). Interestingly, patients with delirium presented lower functional status (Barhtel Index: 58.5±30 vs. 77.2±27.7; p=0.001), more frailty (proportion of at least moderate frailty: 54.3% vs. 29.6%; p=0.009) and more cognitive impairment (proportion of at least moderate dementia: 28.3% vs. 12.5%; p=0.038) than patients without delirium. Fever is the key method for COVID-19 screening.7 However, in older adults awareness of other clinical features is mandatory, including falls and delirium, which may coincide with infection onset.1,8 Cardinal delirium manifestations are cognitive disturbances with impaired orientation, temporal fluctuation, and onset in few hours or days.9,10 In our series it is associated to poorer prior functional and cognitive status, and higher mortality.
Physicians and general population must gain knowledge of the COVID-19 special and unique aspects in geriatric populations lowering thus suspicion and testing thresholds for SARS-CoV-2 in older adults.