The coronavirus disease 2019 (COVID-19) produces severe respiratory symptoms such as bilateral pneumonia associated to a high morbidity and mortality, especially in patients of advanced age. Vitamin D deficiency has been reported in several chronic conditions associated with increased inflammation and dysregulation of the immune system. Vitamin D in modulates immune function too. Vitamin D receptor (VDR) is expressed by most immune cells, including B and T lymphocytes, monocytes, macrophages, and dendritic cells and the signalling of vitamin D and VDR together has an anti-inflammatory effect. Some studies have reported that vitamin D treatment could be useful for the prevention and treatment of COVID-19 because vitamin D plays an important role as a modulator of immunocompetence. Over the last few months, some studies have hypothesized the possible beneficial effect of vitamin D supplementation in patients with COVID-19 in order to improve the immune balance and prevent the hyperinflammatory cytokine storm. Some preliminary studies have already shown promising results with vitamin D supplementation in hospitalized COVID-19 patients. Vitamin D should be administered daily until adequate levels are achieved due to vitamin D behaves as a negative acute phase reactant (APR). Despite the lack of evidence on specific doses of vitamin D to treat COVID-19 in older adults, authors consider it is necessary to standardize the use in clinical practice. These recommendations advice supplement vitamin D in a protocoled fashion based on expert opinions, level of evidence 5.
La enfermedad por coronavirus 2019 (COVID-19) produce síntomas respiratorios graves, como la neumonía bilateral, asociados a una elevada morbilidad y mortalidad, especialmente en pacientes de edad avanzada. La deficiencia de vitamina D se ha reportado en varias condiciones crónicas asociadas con el aumento de la inflamación y la desregulación del sistema inmunológico. La vitamina D también modula la función inmunitaria. El receptor de la vitamina D (VDR) se expresa en la mayoría de las células inmunitarias, incluidos los linfocitos B y T, los monocitos, los macrófagos y las células dendríticas, y la señalización conjunta de la vitamina D y el VDR tiene un efecto antiinflamatorio. Algunos estudios han informado de que el tratamiento con vitamina D podría ser útil para la prevención y el tratamiento de la COVID-19 porque la vitamina D desempeña un papel importante como modulador de la inmunocompetencia. En los últimos meses, algunos estudios han planteado la hipótesis del posible efecto beneficioso de la suplementación con vitamina D en pacientes con COVID-19 para mejorar el equilibrio inmunitario y prevenir la tormenta de citoquinas hiperinflamatorias. Algunos estudios preliminares ya han mostrado resultados prometedores con la suplementación de vitamina D en pacientes con COVID-19 hospitalizados. La vitamina D debe administrarse diariamente hasta que se alcancen los niveles adecuados debido a que la vitamina D se comporta como un reactante de fase aguda (RFA) negativo. A pesar de la falta de evidencia sobre las dosis específicas de vitamina D para tratar la COVID-19 en adultos mayores, los autores consideran que es necesario estandarizar su uso en la práctica clínica. Estas recomendaciones aconsejan suplementar la vitamina D de forma protocolizada en base a opiniones de expertos, nivel de evidencia 5.
The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), produces severe respiratory symptoms such as bilateral pneumonia associated to a high morbidity and mortality, especially in patients of advanced age. At this time, there is not known active treatment for this virus. Corticosteroids and biological immunomodulators are being used to treat the inflammatory phase of the disease.1
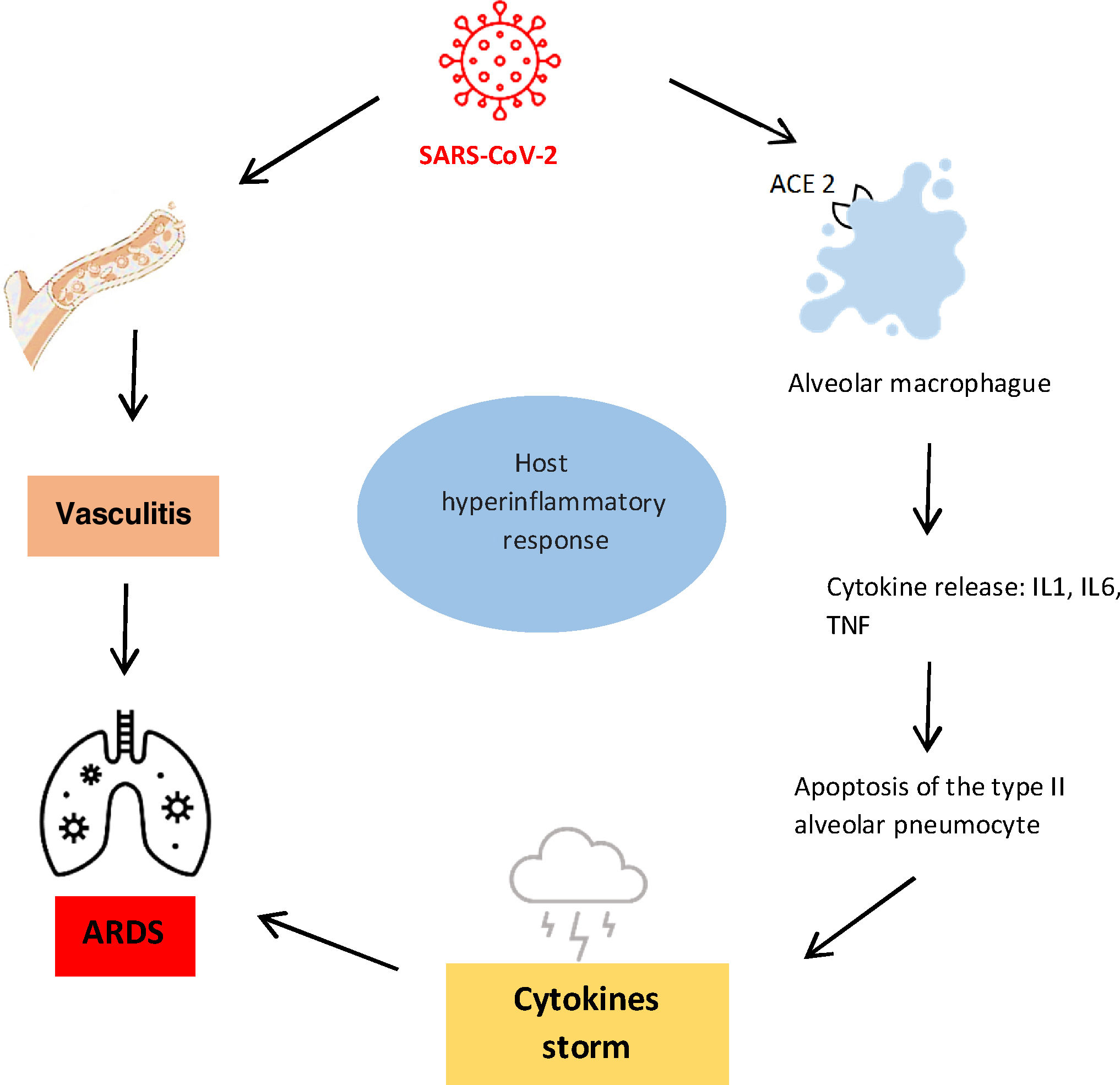
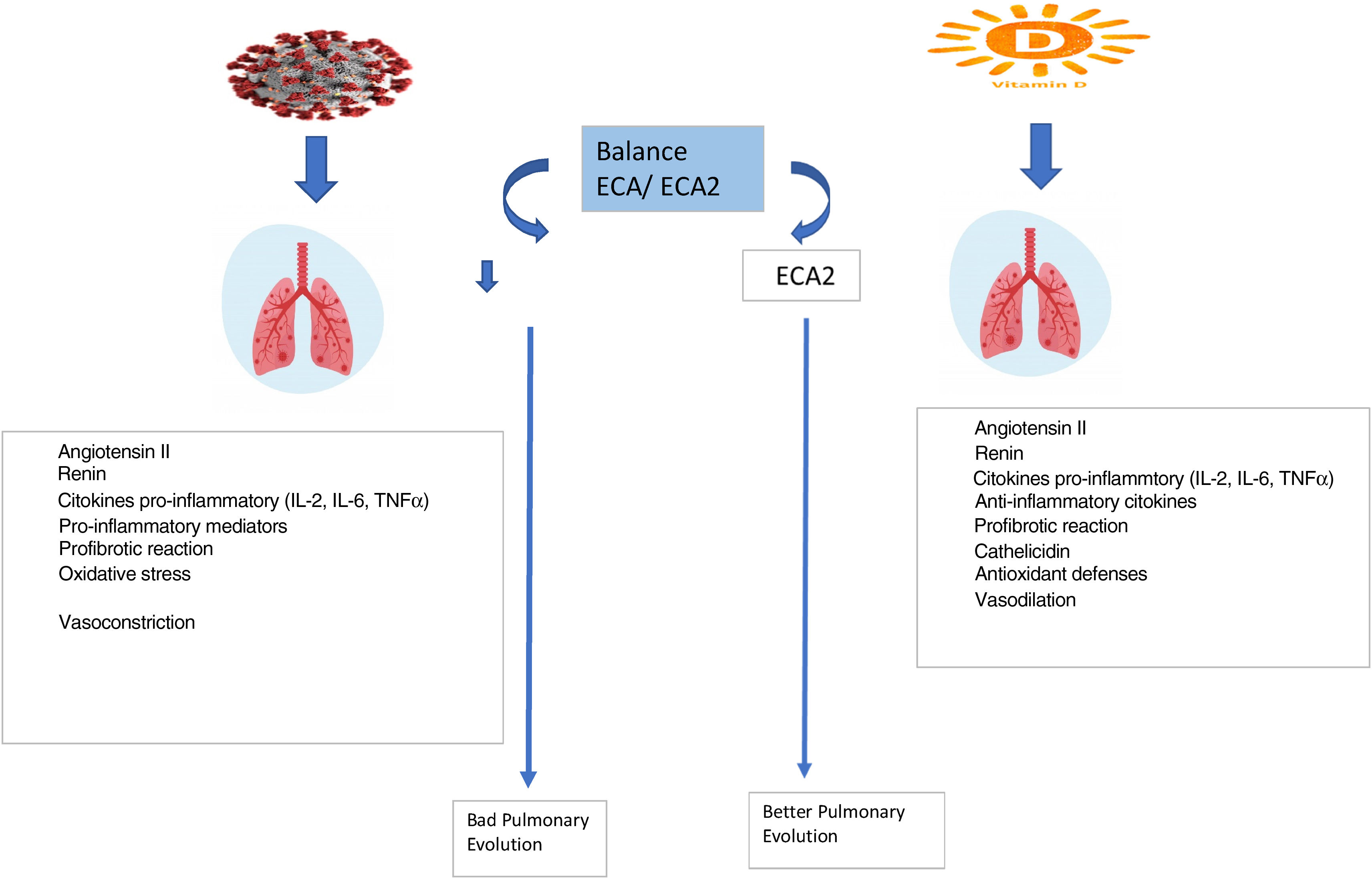
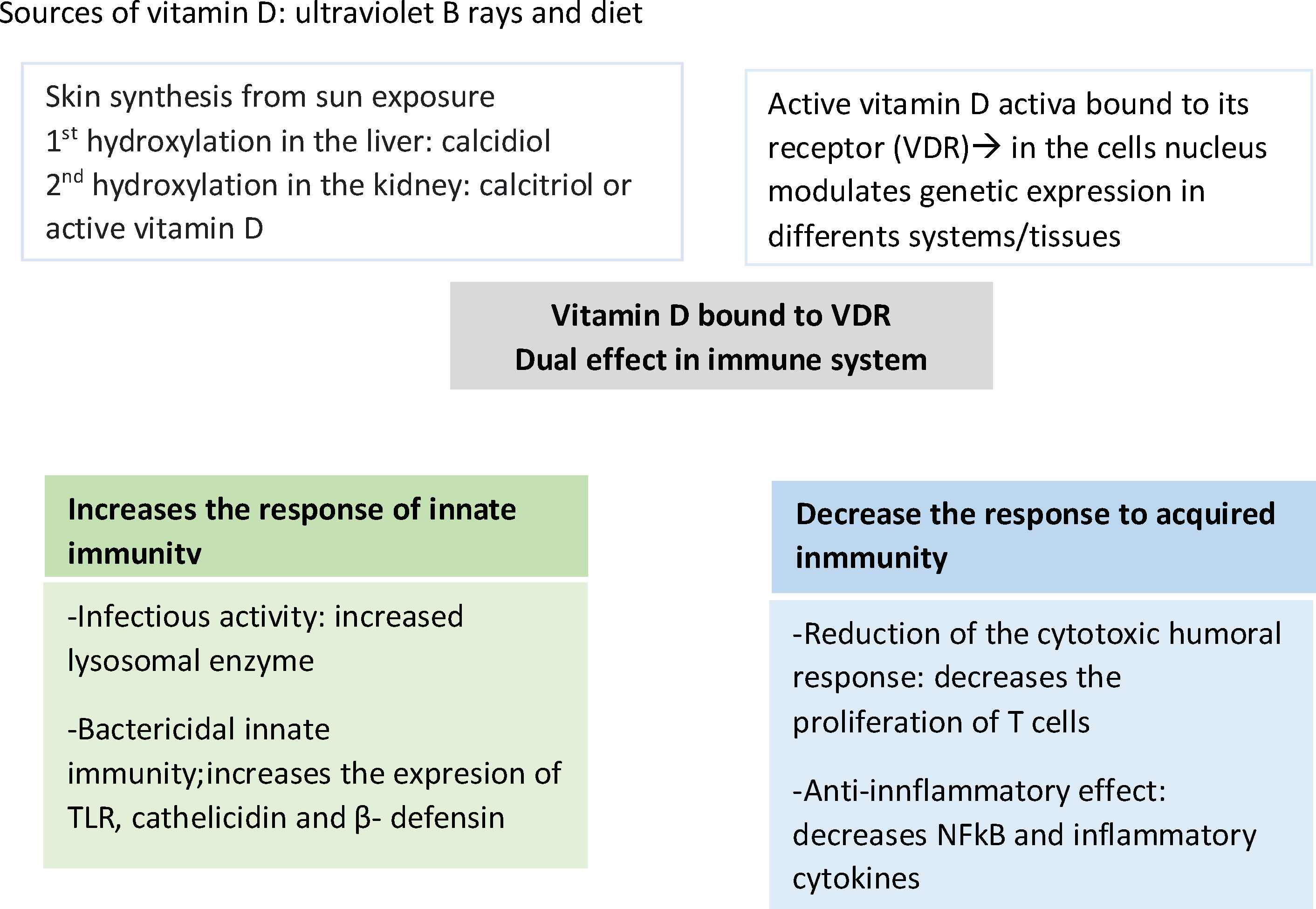
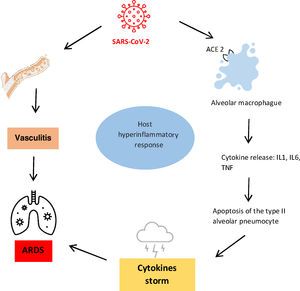
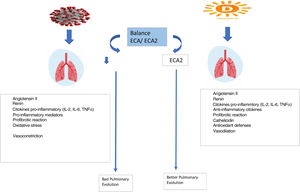
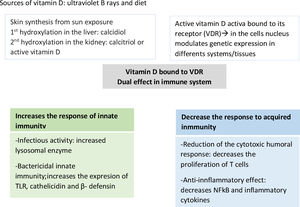
The classic functions of vitamin D (Fig. 1) are to regulate calcium-phosphorus homeostasis and to control bone metabolism. Nevertheless, vitamin D deficiency has been reported in several chronic conditions associated with increased inflammation and dysregulation of the immune system. These observations, together with experimental studies, suggest a critical role for vitamin D in modulating immune function. There are two findings that validate this important non-classical action of vitamin D. First, the vitamin D receptor (VDR) is expressed by most immune cells, including B and T lymphocytes, monocytes, macrophages, and dendritic cells. Second, the signaling of vitamin D and VDR together has an anti-inflammatory effect, promoting the differentiation of dendritic cells and regulatory T cells, reducing the response of T cells and the secretion of inflammatory cytokines. The main cause leading to the increase in mortality rate in people with COVID-19 could be due to acute respiratory distress syndrome (ARDS) by non-antagonized overproduction of pro-inflammatory cytokines2 (Fig. 2).
In this context, some studies have reported that vitamin D treatment could be useful for the prevention and treatment of COVID-19.3 Vitamin D plays an important role as a modulator of immunocompetence (Fig. 3) with respect to both innate and adaptive immunity, and may play a role in the cytokine storm process as well as in the coagulopathy and the cardiac damage of COVID-19.4
Each patient's immune defenses play a major role in mitigating the negative impact of SARS-CoV-2. Vitamin D is an important modulator of the immune system. Although serum 25-hydroxyvitamin D levels can be raised through diet or supplements, most vitamin D in the body is the result of dermal synthesis from ultraviolet radiation. The production of vitamin D in the skin, however, can be limited by latitude, skin-covering clothes, the use of sunblock, and skin pigmentation. Vitamin D deficiency affects a high percentage of the world population. Serum 25-hydroxyvitamin D levels are suboptimal, not only in specific risk groups but also in healthy adults from many countries. Low vitamin D levels, therefore, represent a risk factor for several different pathologies, including SAR-CoV-2. An ecological design study on the association between vitamin D deficiency and COVID-19 incidence, complications, and mortality across 46 countries Reported a population-level association between the prevalence of vitamin D deficiency and the risk of being infected with COVID-19, severity of the disease, and the risk of dying from it.5
COVID-19 is less prevalent in pregnant women, children and in Japanese people,6 whose rates of vitamin D deficiency are lower.7 On the other hand, lower levels of vitamin D have been related to an increased risk of infection,8 as well as poorer short-term prognosis in patients with COVID-19.9 Furthermore it is an evidence that vitamin D insufficiency and deficiency are common in older adults.10,11
Over the last few months, some studies have hypothesized the possible beneficial effect of vitamin D supplementation in patients with COVID-19 in order to improve the immune balance and prevent the hyperinflammatory cytokine storm since immune dysregulation is a key feature of severe COVID-19. The restoration of immune balance could prevent the hyperinflammatory cytokine storm. It is known that vitamin D is necessary for the maintenance of normal immune function. Likewise, in the context of COVID-19, vitamin D could also play a dual role in controlling viral replication initially, and subsequently, dampening hyperinflammation could have beneficial effects.12,13 Vitamin D levels are very low in countries such as Spain, Italy and Switzerland,14 where a correlation has been observed between vitamin D levels, the number of COVID-19 cases and mortality related to this disease.
Some preliminary studies have already shown promising results with vitamin D supplementation in hospitalized COVID-19 patients. A meta-analysis15 has described a lower mortality rate in patients in whom vitamin D was administered (10.6%) compared to controls (23.9%). Two retrospective studies16,17 included in this meta-analysis showed a decrease in the score of the OSCI scale (WHO Ordinal Scale for Clinical Improvement) in the group treated with vitamin D, a third study included demonstrated a lower rate of admission in intensive care units18 and the fourth one showed a significant decrease in serum fibrinogen levels.19 Likewise, in one of the studies,17 administration of vitamin D3 in bolus occurred in the month before admission to hospital.
The vitamin doses administered are heterogeneous across studies ranging from a single dose of 400,000IU of cholecalciferol the day of hospital admission to 50,000IU in patients who did not receive more than 800IU per day during the month prior to the hospital admission.20
Vitamin D should be administered daily until adequate levels are achieved as it is a steroid hormone,21 for that reason we have focused on guidelines that allow better conciliation with daily hospital activity. In this same context of SARS-CoV-2 infection, vitamin D behaves as a negative acute phase reactant (APR),22 therefore a progressive decrease can be generated due to human consumption during the course of the infection.23 Firstly, calcifediol (vitamin D2) is 3–6 times more powerful than cholecalciferol (vitamin D3) although its half-life is shorter; secondly, the objective of treatment should be to achieve quickly the adequate levels and maintain it for a minimum of 3 months; and finally, in case of obesity or malabsorption, the use of higher doses than those suggested in these recommendations should be considered.
Recent studies recommend daily supplementation with 800–1000IU of vitamin D20 to reduce the incidence and severity of symptoms of older patients with acute SARS-CoV-2 infection. However, these recommendations will focus on older patients with acute SARS-CoV-2 virus infection. This is supported by a study with a small sample size (n=76)17 where high doses of calcifediol significantly reduced the need for admission to intensive care units.
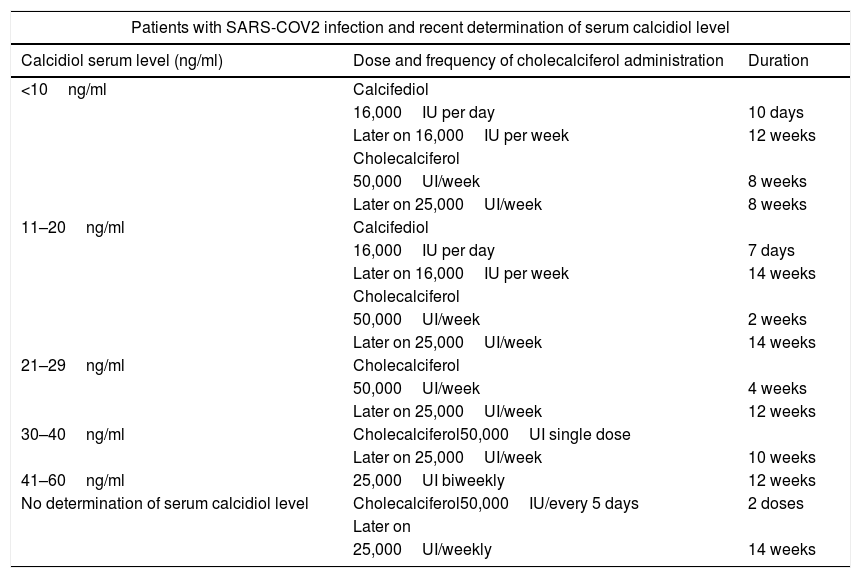
Despite the lack of evidence on specific doses of vitamin D to treat COVID-19 in older adults, we consider it is necessary to standardize the use in clinical practice. In fact, a recent review concluded that, despite limitations and remaining uncertainties, accumulating evidence strongly supports widespread vitamin D supplementation, in particular of high-risk populations, as well as high-dose supplementation of those infected. Given the dynamics of the COVID-19 pandemic, the benefit–risk ratio of such supplementation calls for immediate action even before results of ongoing large-scale randomized trials become available.24 The first step to do that in hospitalized older adults should be to determine the amount of vitamin D on admission together with D-Dimer, C-reactive protein, ferritin, fibrinogen and other APR; and if needed to supplement vitamin D in a protocoled fashion as suggested in Table 1 (based on expert opinions, level of evidence 5). The doses of calcifediol and cholecalciferol have been detailed to facilitate vitamin D supplementation regardless of the presentations available in the hospital pharmacies of each clinical center.
Recommended dose of vitamin D supplementation.
| Patients with SARS-COV2 infection and recent determination of serum calcidiol level | ||
|---|---|---|
| Calcidiol serum level (ng/ml) | Dose and frequency of cholecalciferol administration | Duration |
| <10ng/ml | Calcifediol | |
| 16,000IU per day | 10 days | |
| Later on 16,000IU per week | 12 weeks | |
| Cholecalciferol | ||
| 50,000UI/week | 8 weeks | |
| Later on 25,000UI/week | 8 weeks | |
| 11–20ng/ml | Calcifediol | |
| 16,000IU per day | 7 days | |
| Later on 16,000IU per week | 14 weeks | |
| Cholecalciferol | ||
| 50,000UI/week | 2 weeks | |
| Later on 25,000UI/week | 14 weeks | |
| 21–29ng/ml | Cholecalciferol | |
| 50,000UI/week | 4 weeks | |
| Later on 25,000UI/week | 12 weeks | |
| 30–40ng/ml | Cholecalciferol50,000UI single dose | |
| Later on 25,000UI/week | 10 weeks | |
| 41–60ng/ml | 25,000UI biweekly | 12 weeks |
| No determination of serum calcidiol level | Cholecalciferol50,000IU/every 5 days | 2 doses |
| Later on | ||
| 25,000UI/weekly | 14 weeks | |
Alternative administration of cholecalciferol in daily regimen:
11-20 ng/mL: cholecalciferol “4,000” IU/daily for 120 days.
21-30 ng/mL: cholecalciferol “3,000” IU/daily for 120 days.
31-40 ng/mL: cholecalciferol “2,000” IU/daily for 120 days.
41-60 ng/mL: cholecalciferol “1,000” IU/daily for 120 days.
Cite: authors’ note.
Finally, clinicians should be aware that supplementation with high doses of vitamin D can cause toxicity, especially hypercalcemia, which can manifest as irreversible cardiovascular and renal damage such as kidney stones25 and the calcification of soft tissues and vascular territories, likewise patient may experience symptoms such as nausea, vomiting; likewise patients may experience increased thirst and depression during treatment.26 However, the therapeutic window of vitamin D is wide and the toxicity associated with its supplementation is rare, with less than 0.1% of hypercalcemia associated with hypervitaminosis D.27 For this reason, we consider it is convenient to measure calcium levels on a regular basis or when toxicity is suspected due to vitamin D supplementation.
Recently, a NICE28 guideline concluded that there was not enough evidence to recommend the use of vitamin D to prevent or treat SARS-CoV-2 infection alone. We recommend the use of calcifediol or cholecalciferol alone with those used to treat COVID-19 stated in international guidelines and protocols. Likewise, the aforementioned NICE guideline has received a wide response.29–31 One of this responses29 indicates the results of a meta-analysis on the benefits of the administration of vitamin D in the prevention of respiratory infections. The second of the cited responses30 emphasizes the presence of five ongoing clinical trials (NCT04579640, NCT04476680; NCT04483635; NCT04386850; NCT04535791) on the effects of vitamin D in the treatment of patients with COVID-19, one of them compared to the British national recommendations of 400IU per day (NCT04579640) and two of them to placebo arm (NCT04386850, NCT04535791). As the pandemic situation continues to get worse (and will possibly continue to worsen during the winter months before the effects of the vaccines are noticeable), additional evidence could come too late.31 We know that in an ideal world, health decisions must be made based on overwhelming evidence, but a time of crisis such as the current one may require a slightly different set of rules.32 In this sense, knowing the responsibility that absence forces based on resounding evidence, we offer these recommendations being aware that in the near future we must review them with the evidence generated.
Conflict of interestThe authors declare that they have no conflicts of interest for this manuscript.
The authors would like to thank Juan María de la Cámara de las Heras, librarian and archivist of Hospital Universitario de la Ribera, for his help in carrying out the necessary literature search for this review.