Dermatophytic pseudomycetoma is a subcutaneous fungal infection by Microsporum canis.
AimsThis work describes a case of dermatophytic pseudomycetoma in a Persian cat.
Patient and methodsA 3-year old female Persian cat showing alopecia, scaling and ulcerated nodules throughout the body, with presence of ulcerated nodules with yellow granular discharges on the dorsum, close to the tail. Mycological and histopathological examinations were realized.
ResultsDiagnosis of dermatophytic pseudomycetoma was established. The cat was treated with griseofulvin, and surgical excision was carried out. Response to therapy was effective during the first months, during which a reduction in nodule frequency was observed. However, despite maintaining the therapy levels, the lesions relapsed and progressed to the point of causing the animal's death.
ConclusionThe clinic evolution showed the progressive and recurrent character of dermatophytic pseudomycetoma.
El pseudomicetoma dermatofítico es una infección fúngica subcutánea causada por Microsporum canis.
ObjetivosEste trabajo describe un caso de pseudomicetoma dermatofítico presentado por un gato persa.
Paciente y métodoUna gata de raza Persa, de 3 años de edad, con signos de alopecia, eritema y nódulos ulcerados, los dos primeros distribuidos en todo el cuerpo, presentó exudado granuloso de color amarillento en los nódulos ulcerados de la región dorsal, próxima a la cola. Fueron realizados exámenes micológicos e histopatológicos.
ResultadosEl diagnóstico de pseudomicetoma dermatofítico fue confirmado a través del cultivo y examen histopatológico de las muestras extraídas. El tratamiento se basó en el suministro de griseofulvina y extirpación quirúrgica, obteniéndose una respuesta eficaz durante los primeros meses con reducción en el número de nódulos observados. Con el transcurso del tiempo, y aún bajo tratamiento, fue constatada la reincidencia de las lesiones que finalmente llevaron a la muerte del animal.
ConclusionesLa evolución clínica evidenció el carácter progresivo y recurrente del pseudomicetoma dermatofítico.
Dermatophytic pseudomycetoma is a subcutaneous fungal infection by Microsporum canis, during which the epidermal stratum corneum is invaded, causing granuloumatous dermatitis and panniculitis. In the majority of cases the lesions are characterized clinically by the presence of firm or soft nodules, which can be ulcerated and show granular discharges.1,5,7,10
A 3-year old female Persian cat showing alopecia, scaling and ulcerated nodules was studied. When clinically examined, the feline was considered to be in good condition and remained alert but presented focal areas of alopecia throughout the body. The dorsum region showed small nodules with one of a larger size (3cm ∅) near the tail, ulcerated and presenting a yellow granular discharge. After the clinical examination, exudates were vacuum collected directly from the lesions. Tests were run to determine the hematological profile as well as for the detection of the feline leukemia virus. Isolates of M. canis were obtained from exudates, skin and hair specimens.
The results from the hematological profile were found to be within the normal range of values, whilst the feline leukemia virus tested negative, all of which confirmed the dermatophytic pseudomycetoma diagnosis. Therapy with griseofulvin 25mgkg−1 every 12h and weekly immersions with ketoconazole reduced the frequency of lesions within 2 months, but they did not disappear completely.
After approximately 5 months of therapy the clinical symptoms became more severe and the animal showed an evident discomfort, due essentially to scaling and the formation of several coalescent nodules. The latter were of various diameters (2.5–5.0cm), whether on the rear dorsum (Fig. 1) or at the tail's base, from which yellow granular exudates were discharged. The adjacent ventral region had a non-ulcerated nodule close to the left inguinal tit.
Surgery therapy was recommended for the excision of the larger nodules, after which they underwent fungal culture and histopathological examination. Fragments and exudates from the inner parts of nodules were collected and cultured on Sabouraud agar mixed with cyclohexamide and chloramphenicol and incubated at 37°C for 10 days, after which macroscopic and microscopic isolate identifications were carried out. The specimens were stained with haemotoxylin-eosin, the periodic acid Schiff (PAS) and silver-metenamine Gomori to identify the fungal elements.
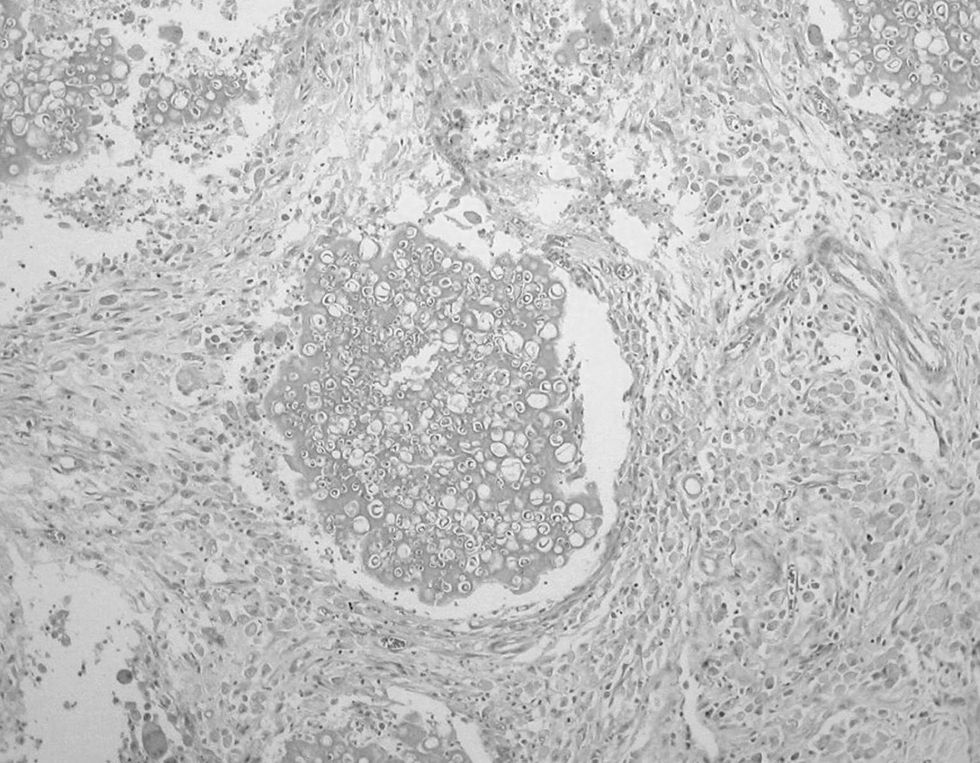
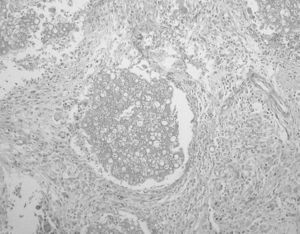
Histopathological examinations showed granuloumatous inflammation with presence of giant foreign cells, neutrophils and lymphocytes, which surrounded fungal masses with irregular hyphea and bulbous dilatations resembling spores. All these were suspended within an abundant amorphic eosinophilic matrix, typical of the Splendore–Hoeppli reaction (Fig. 2). In the cultures, flat, cottony and white with yellow reverse colonies were obtained. In the microscopic examination, hyaline, septate and branched hyphae with plenty of spindle-shaped macroconidia were observed, with asymmetrical apexes and thick walls with thin septa, containing 6–15. These findings made the identification of M. canis possible.
After surgical excision and with the results from the mycological and histopathological tests, griseofulvin therapy was resumed (25mgkg−1) and within 30 days the animal showed clear symptoms of clinical recovery. Weight gain, decrease in scaling, better hair appearance and complete healing of the surgery scar were observed. The antifungal agent was administered for 4 months and pulse therapy on griseofulvin (25mgkg−1 12/12h, 1 week per month) and weekly immersions with ketoconazole to control dermatophytes on skin and hair were established.
Approximately 6 months after surgery several small nodules reappeared on the dorsum region, from the cervical region across to the base of the tail (Fig. 3). These did not respond to therapy and due to their large number surgical excision was considered impractical. The clinical symptoms progressed to weight loss, apathy, fever and the appearance of several ulcerated, coalesced nodules on the rear dorsum region and the base of the tail (2.5–5.0cm ∅), which showed yellow granular exudates. Scaling was so severe that it eventually led to auto-mutilation. Once again granular discharge specimens were collected and delivered for mycological examination, which confirmed the pseudomycetoma diagnosis.
Hematological examinations indicated left deviation leukocytosis. Neutraceuticals were employed and therapy involving cephalexine (20mgkg−1 12/12h, 10 days) and griseofulvin (25mgkg−1 12/12h, 90 days) was recommended, but did not yield positive results. Thus, the prescription was shifted to therapy with itraconazole (10mgkg−1 every 24h, 30 days), which did not result in improvement, either. The mycosis progressed, with the animal showing obvious discomfort, inappetence and progressive weight loss, eventually leading to the animal's death. Necropsy was performed but no further alterations could be observed.
The majority of studies on this pathology have involved Persian cats2,3,6,8,10; however, some studies have dealt with common, short-haired domestic cats.9 Skin lesions are most commonly located on the dorsum region and on the base of the tail3,6,9 and it has been suggested that pseudomycetoma in cats may reflect immunodeficiency or aberrant immune response.4 In this work the feline tested negative for the feline leukemia virus, which was also the outcome reported in other works and likewise for the feline immunodeficiency virus.2,6
The results from the mycological and histopathological examinations are in agreement with much of the reviewed information regarding the identification of M. canis, presence of histiocytic giant cells and the Splendore–Hoeppli reaction.2,6,9,10 Isolations of M. canis from hair and skin specimens were observed,6 which identified ectothrix arthroconidia through direct hair examination.
For the majority of cases of follow up therapy, lesion relapse occurred after variable time periods, even in cases where surgical excision was performed. Similar results were reported for therapies based on antifungal agents, e.g. griseofulvin, itraconazole and/or terbinafine.2,9 The presence of granulomas may make difficult drug access to the inner nodule, rich in fungi structures difficult, which may result in a reduction of the efficacy of these antifungals on M. canis. Its use combined with antibiotic therapy was successful in the case of secondary piodermitis, resulting in reduced number of lesions.9 However, progression to death or euthanasia has been common.2,9 A recent case of sublumbar pseudomycetoma leading to mechanical obstruction of the colon and rectum was recorded.8
The clinic evolution showed the progressive and recurrent character of dermatophytic pseudomycetoma.
We thank CNPq for award of a scholarship and Capes for financial support.