Although the management of invasive fungal infection (IFI) has improved, a number of controversies persist regarding the approach to invasive fungal infection in non-neutropenic medical ward patients.
AimsTo identify the essential clinical knowledge to elaborate a set of recommendations with a high level of consensus necessary for the management of IFI in non-neutropenic medical ward patients.
MethodsA prospective, Spanish questionnaire, which measures consensus through the Delphi technique, was anonymously answered and e-mailed by 30 multidisciplinary national experts, all specialists (intensivists, anesthesiologists, microbiologists, pharmacologists and specialists in infectious diseases) in IFI and belonging to six scientific national societies. They responded to five questions prepared by the coordination group after a thorough review of the literature published in the last few years. For a category to be selected, the level of agreement among the experts in each category had to be equal to or greater than 70%. In a second round, 73 specialists attended a face-to-face meeting held after extracting the recommendations from the chosen topics, and validated the pre-selected recommendations and derived algorithm.
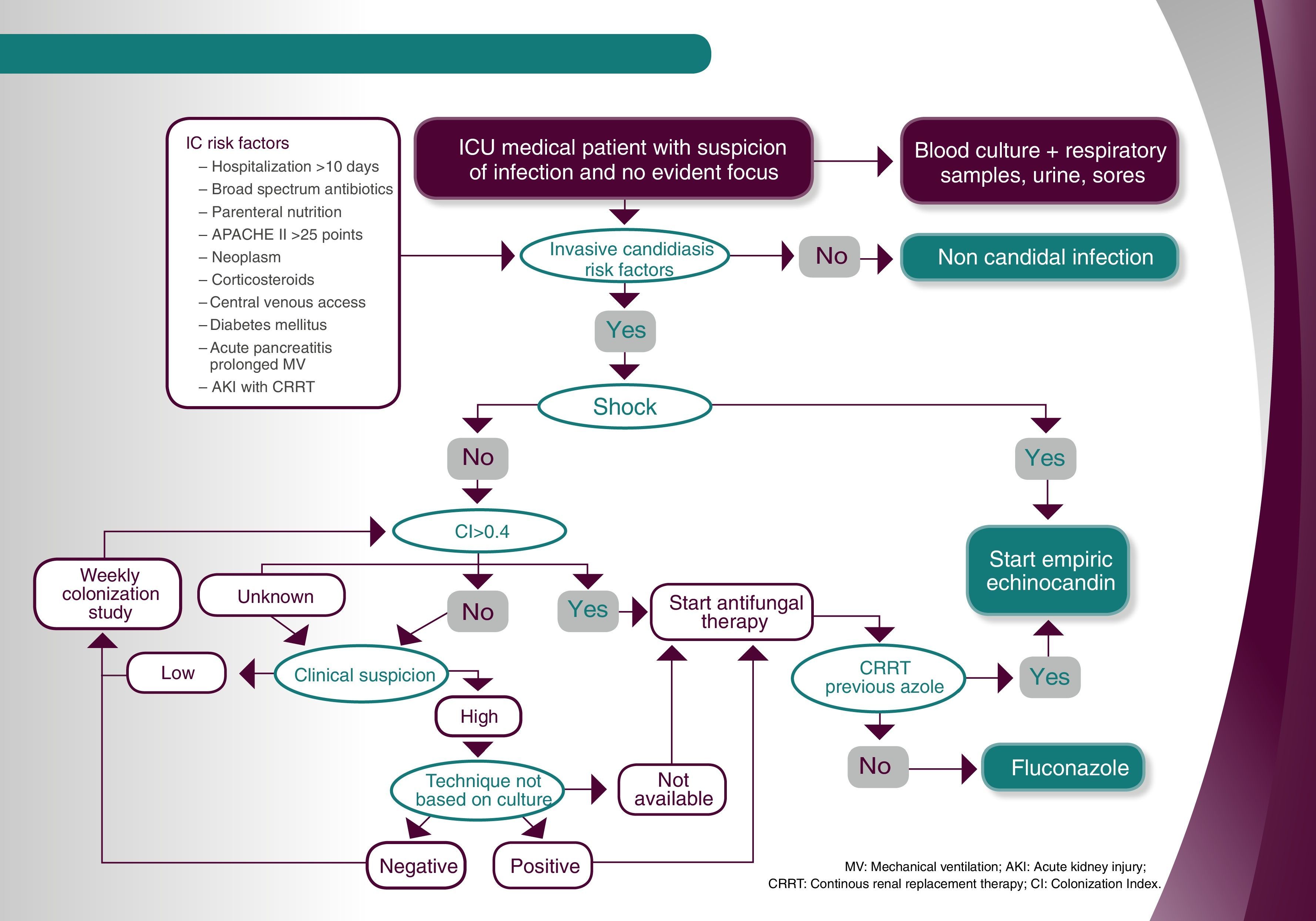
ResultsThe following recommendations were validated and included in the algorithm: 1. several elements were identified as risk factors for invasive candidiasis (IC) in non-hematologic medical patients; 2. no agreement on the use of the colonization index to decide whether prescribing an early antifungal treatment to stable patients (no shock), with sepsis and no other evident focus and IC risk factors; 3. agreement on the use of the Candida Score to decide whether prescribing early antifungal treatment to stable patients (no shock) with sepsis and no other evident focus and IC risk factors; 4. agreement on initiating early antifungal treatment in stable patients (no shock) with a colonization index>0.4, sepsis with no other evident focus and IC risk factors; 5. agreement on the performance of additional procedures in stable patients (no shock) with sepsis and no other evident focus, IC risk factors, without colonization index>0.4, but with a high degree of suspicion.
ConclusionsBased on the expert's recommendations, an algorithm for the management of non-neutropenic medical patients was constructed and validated. This algorithm may be useful to support bedside prescription.
A pesar de que el manejo de la micosis invasiva ha mejorado, persisten ciertas controversias en su tratamiento en pacientes no neutropénicos.
ObjetivosIdentificar el conocimiento clínico esencial y elaborar, con un alto nivel de consenso, las recomendaciones necesarias para el manejo de la micosis invasiva en pacientes no neutropénicos.
MétodosTreinta expertos multidisciplinarios españoles en micosis invasiva (intensivistas, anestesistas, microbiólogos, farmacólogos y especialistas en enfermedades infecciosas) pertenecientes a 6 sociedades científicas contestaron anónimamente un cuestionario que evaluaba el grado de consenso mediante la técnica Delphi. Los expertos respondieron a 5 preguntas elaboradas por los coordinadores después de una revisión exhaustiva de la bibligorafía reciente. El grado de acuerdo necesario para seleccionar una categoría fue igual o superior al 70%. Posteriormente, 73 especialistas asistieron a una reunión en que se extrajeron las recomendaciones que se utilizaron en la elaboración de un algoritmo para la ayuda en la toma de una decisión clínica.
ResultadosLas recomendaciones validadas e incluidas en el algoritmo fueron las siguientes: 1) varias situaciones se definieron como factores de riesgo para la candidiasis invasiva (CI) en pacientes no hematológicos; 2) no hubo acuerdo sobre el uso del índice de colonización para decidir la prescripción de tratamiento antifúngico precoz en pacientes estables (sin shock) con septicemia, sin foco evidente y con factores de riesgo para CI; 3) hubo acuerdo en el uso del Candida Score para decidir la prescripción de tratamiento antifúngico precoz en pacientes estables (sin shock) con septicemia, sin foco evidente y con factores de riesgo para CI; 4) hubo acuerdo en el inicio de tratamiento antifúngico precoz en pacientes estables (sin shock) con sepsis, sin foco evidente e índice de colonización >0,4 y con factores de riesgo para CI; 5) hubo acuerdo para realizar los procedimientos diagnósticos adicionales en pacientes estables (sin shock) con septicemia, sin foco evidente, factores de riesgo para CI e índice de colonización <0,4, pero con alto índice de sospecha.
ConclusionesSe ha elaborado un algoritmo de manejo de la CI en pacientes no neutropénicos basado en las recomendaciones de expertos. Este algoritmo puede ser útil como soporte a la prescripción a pie de cama.
The diagnostic and therapeutic approaches to invasive fungal infection (IFI) are still nowadays relevant challenges in Intensive Care Units (ICUs).27 This is due to an increasing incidence of IFI in ICUs,3 as well as, in comparison with the rest of the hospital services, to a higher complexity of its diagnosis and treatment in critically-ill patients.29
Candidemia stands as the most prevalent fungal infection in ICUs.11 In fact, in ICUs, the number of IFI due to Candida is 10 times more frequent than those due to Aspergillus. Moreover, these infections are associated to a higher rate of mortality, a longer period of hospitalization and higher healthcare costs.26
Early diagnosis and treatment of invasive candidiasis (IC) leads to a significant decrease in mortality and other associated consequences.13 In this context, the use of predictive models for IC may contribute to the identification of risk patients who can benefit from an appropriate treatment against infection.18,24 Nevertheless, in spite of the positive clinical impact associated to the employment of tools, such as the Candida Score,17 there are a large number of professionals who do not use or do not consider using it in their daily clinical practice.5
The primary goal of the current study is to analyze the current situation of the management of IFI in non-neutropenic patients from medical areas in the Spanish hospitals, and also to give a set of therapeutic recommendations for different scenarios through the use of the DELPHI methodology.
For this purpose, a panel was formed including 30 specialists from different geographic locations in our country from six scientific societies involved in this research: Spanish Society of Mycology (AEM), as the promoter; the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC); the Spanish Society of Anesthesiology, Resuscitation and Pain Therapeutics (SEDAR); the Spanish Society of Intensive Care, Critical Care and Coronary Units (SEMICYUC); the Spanish Society of Chemotherapy (SEQ); the Spanish Society of Hospital Pharmacy (SEFH). All the specialists have extensive experience in the treatment of critically-ill patients. They were requested to answer a questionnaire developed by the seven coordinators responsible for this research, who had previously carried out a thorough review of the existing literature, as done in the two previous editions of this project.30,31
In a second round, subsequent to the elaboration of the resulting recommendations by the coordinators group, a second analysis was requested in a face-to-face meeting in which 73 specialists from throughout the country who care for non-neutropenic patients in medical wards, validated the pre-selected recommendations and the derived algorithm through a voting procedure.
The Delphi methodology was used for the development of this study to optimize the enquiry process. More specifically, thanks to the Delphi methodology, we were able to know the group opinion; not just that of an individual, but the opinion of a group formed by experts in different areas of information suggested by the coordinators. The level of consensus required in each category had to be equal or higher than 70% (21 out of 30) in Top 4 (score of 7 points or more) of all experts consulted, in each question. A total of five questions, all posed by the coordinators (Annex 1) were evaluated by the experts using a metric scale.
The study methodology was based on the development of just one phase aimed to reveal the level of consensus of the questions. For this purpose, on May 19 and 26, 2014, the 30 participating specialists (Annex 2) responded to an online and anonymous questionnaire of five questions. The coordinators responsible for the systematic research of the literature to elaborate the questions, did not answer the questionnaire. Thereafter, as previously mentioned, some recommendations and an algorithm were produced and validated by 73 experts in a face-to-face meeting held on 25 September 2014 (Annex 3).
Results1. Choose those variables that may be considered risk factors for IC in non-hematologic patients
The following answers were provided by the coordinators: Multifocal colonization by Candida, parenteral nutrition, high degree of severity (APACHE>25 points), severe acute pancreatitis, extended hospitalization (>10 days in ICU or hospital), kidney failure with hemodialysis, central venous access, corticosteroid treatment, broad spectrum antibiotic treatment for more than 72h, venous femoral catheter, existence of solid neoplasia, prolonged mechanical ventilation (>7 days), and diabetes mellitus.
Rationale. Recent studies published on candidemia or invasive candidiasis have not been able to accurately differentiate the risk factors associated with this entity when affecting patients with underlying medical conditions4,25 (discarding patients suffering from oncohematological diseases and hematopoietic stem cell transplant recipients), in those admitted to critical care units,19 as well as those to conventional units.7
However, these studies have well established that certain factors, such as a central venous catheter (CVC), either temporary or permanent, especially when employed for the administration of parenteral nutrition, previous colonization by the same species of Candida, the existence of specific comorbidities (such as solid tumors currently or recently treated with chemotherapy or kidney failure requiring external replacement therapy, and also receiving certain prolonged drug regimens (especially corticosteroids and broad spectrum antibiotics)8,28 contribute clearly to the development of this infection. Once the diagnosed cases upon hospital admission have been discarded, the average hospital stay of patients with candidemia is approximately 3 weeks.2
The vast majority of the specialists (96.4%) considered multifocal colonization by Candida and parenteral nutrition as risk factors in this population. Particularly, on a scale from 0 to 10, in which 10 represents the highest level of agreement, 27 out of 28 participants granted 7 or more points to both variables, thus determining a consensual agreement (Top 4≥70%). Likewise, consensus was also reached when considering as risk factors for IC in non-neutropenic medical patients the high degree of severity (26 answers with 7 or more points (Top 4: 92.9%); prolonged hospitalization (25; 89.3%); severe acute pancreatitis (25; 89.3%); broad spectrum antibiotic treatment for more than 72hours (24; 85.7%); corticosteroid therapy (24; 85.7%) and the presence of a central venous access (24; 85.7%), kidney failure requiring hemodialysis (24; 85.7%), a femoral venous catheter (23; 82.1%), or the presence of a solid tumor (22; 78.6%).
In contrast, consensus was not reached (Top 4<70%) when considering prolonged mechanical ventilation (19 answers with 7 or more points; Top 4: 67. 9%) and diabetes mellitus (18; 64.3%) as risk factors.
2. Agreement on the use of the colonization index to decide whether prescribing an early antifungal treatment to stable patients (no shock) with sepsis and no other evident focus and risk factors associated to IC
Rationale. Although multi-colonization is a commonly accepted risk factor for the diagnosis of systemic candidiasis in high risk surgical patients, to date its role in the management of non-neutropenic medical patients has still not been correctly determined.6
Even though most of the members of the panel (66.7%) believed it is necessary to use the colonization index to decide the early administration of antifungal treatment in these patients, no consensus was reached (Top 4<70%). Specifically, on a scale from 0 to 10 points, in which 10 is the highest degree of agreement, only 18 out of 27 experts granted this regard 7 or more points.
3. Agreement on the use of the Candida Score to decide whether prescribing early antifungal treatment to stable patients (no shock) with sepsis and no other evident focus and risk factors associated to invasive IC
Rationale. Many studies have proven the usefulness of the Candida Score, a risk classification system validated in case of based suspicion of IC or candidemia, to decide whether establishing early treatment in patients hospitalized in ICUs with specific risk factors.1,9,17,18 Actually, a Candida Score value higher than 2.5 increases up to 7 times the risk of suffering documented invasive infection by Candida.16 Unfortunately, a perfect stratification risk model has not yet been developed for patients admitted to conventional units, and for a great number of those hospitalized in ICUs, whereas the use of the Candida Score in patients with non-neutropenic medical conditions may be significantly more difficult.
Most of the experts (70.4%) agreed on using the Candida Score to decide whether or not to administer an antifungal treatment in this situation. Specifically, and on a scale from 0 to 10 points in which 10 represents the highest degree of agreement, 19 specialists out of 27 granted this regard 7 or more points, thus reaching a consensual agreement (Top 4≥70%).
4. Agreement on initiating early antifungal treatment in stable patients (no shock) with sepsis and no other evident focus and risk factors associated to IC, and with a colonization index>0.4
Rationale. The so-called Pittet colonization index, both in its initial and corrected versions, is applied uniformly to patients admitted to the ICU after a surgical procedure (in most cases of the abdominal cavity).22,23 Its main drawback is the need for previous surveillance cultures to detect Candida in mucous membranes or fluids, and in case of the corrected version, the need for performing quantitative cultures of these samples.14 The detection of values superior to 0.4 between the ratios of cultures equal or greater than 105CFU/ml of Candida spp. in all cultures already performed (for the corrected version of the index), offers sensitivity and specificity values of 100% to determine the risk of IC in these patients.23 Nevertheless, these index values for diagnosis and clinical management have not yet been established in medical patients.6
Most participants (78.6%) considered necessary to start an early treatment with antifungals in patients with sepsis and IC risk factors that are stable and have a colonization index higher than 0.4. Specifically, and in a scale from 0 to 10 points in which 10 stands for the highest degree of agreement, 22 out of 28 experts granted 7 or more points to this regard, achieving a high rate of consensus (Top 4≥70%).
5. Agreement on the performance of the following procedures in stable patients (no shock) with sepsis and no other evident focus, and with risk factors associated to invasive candidiasis, without colonization index>0.4, but with high degree of clinical suspicion
The following answers were provided by the coordinators: Start antifungal therapy in the absence of non-culture based microbiologic techniques, start antifungal therapy in the event of a positive culture by a non-culture based method, determination of non-culture based microbiological techniques to diagnose IC (if possible) were considered necessary.
Rationale. Microbiological techniques, other than conventional cultures, aimed to detecting biomarkers of fungal infection, have shown encouraging results to further progress in the diagnosis of invasive candidiasis.15,20 The most studied are the detection of Candida mannan antigens, antibodies against Candida mannan antigens, anti-mycelium antibodies (especially in patients admitted to critical care units), and (1→3)-β-d-glucan. Specifically, by combining mannan antigens with anti-mannan antibody, levels of sensitivity and specificity exceeding 80% in critically-ill hematologic patients can be obtained.
Likewise, the detection of anti-mycelium antibodies in critically-ill patients provides high rates of sensitivity and specificity for which it is an important tool for patients’ follow-up.21,32,33 Lastly, the determination of (1→3)-β-d-glucan has been the most studied biomarker for the early diagnosis of candidiasis, offering a sensitivity exceeding 65%, specificity greater than 80% and a negative predictive value of 95%. While some of these techniques are not frequently used in most microbiology laboratories and they can be expensive, the clinical practice guide published in 2012 by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), recommends using these biomarkers for the diagnosis of IC with very moderate degree of evidence.10 Also, the Surviving Sepsis Campaign establishes recommendations whereas the use of these techniques is useful to treat patients with severe sepsis and a strong suspicion of IC.12
The degree of consensus among the experts was high (Top 4≥70%) as regards the need to use IC non-culture based diagnostic methods or to initiate treatment in case any of the techniques show a positive result. Concretely, in a scale from 0 to 10 in which 10 represents the highest degree of agreement, 26 out of 28 specialists (92.9%) granted 7 points or more to the use of techniques for the diagnosis of IC; 23 members of the panel (82.1%) agreed with this valuation in case of starting treatment because of a positive result.
In contrast, the need to start antifungal treatment in case of not having non-culture based microbiological techniques was taken into account by just 67.9% of the specialists, thus consensus was not reached (Top 4<70%).
Recommendations and algorithmOnce the results obtained with the Delphi methodology applied to IFI in non-neutropenic medical patients were known, the recommendations exhibited in Table 1 were extracted. They were based on questions, which reached a degree of agreement equal or greater than 70%. Thereafter, the recommendations and algorithm derived from these questions (Fig. 1) were validated in a meeting with the hospital experts. This algorithm may be useful to support bedside prescription.
Recommendations derived from the questions about the best procedures for the management of IFI in non-neutropenic medical ward patients.
| 1. The following variables were considered risk factors for invasive candidiasis: multifocal colonization by Candida, parenteral nutrition, prolonged hospitalization, severe acute pancreatitis, broad spectrum antibiotic treatment for more than 72h, corticosteroid therapy, the presence of a central venous access, kidney failure requiring hemodialysis, a femoral venous catheter, and the presence of a solid tumor. |
| 2. There was no agreement on the use of the Colonization Index to determine whether prescribing an early antifungal treatment to stable patients with sepsis (no shock) and no other evident focus and risk factors associated to invasive candidiasis. |
| 3. Use the Candida Score to determine prescribing early antifungal treatment to stable patients with sepsis (no shock) and no other evident focus and risk factors associated to invasive candidiasis. |
| 4. Start early antifungal treatment in stable patients with sepsis (no shock) and no other evident focus and risk factors associated to invasive candidiasis. |
| 5. Use invasive candidiasis non-culture based diagnostic methods or start antifungal treatment in case any of the techniques reveal a positive result in stable patients with sepsis (no shock) and no other evident focus and with risk factors associated to invasive candidiasis. In the absence of non-culture based microbiological techniques there's no need to start antifungal treatment. |
The study has been sponsored by MSD Laboratories, Spain.
Rafael Zaragoza Crespo
Intensive Care Department, Dr. Peset University Hospital. Valencia, Spain
Ricard Ferrer Roca
Intensive Care Department, Vall d¿Hebron University Hospital. Barcelona, Spain
Alejandro Hugo Rodríguez
Intensive Care Department, Joan XXIII University Hospital. Tarragona, Spain
Emilio Maseda Garrido
Department of Anesthesiology and Surgical Critical Care, La Paz University Hospital. Madrid, Spain
Pedro Llinares Mondéjar
Infectious Diseases Department, A Coruña University Complex. A Coruña, Spain
Santiago Grau Cerrato
Pharmacy Department, Hospital del Mar. Barcelona, Spain
José María Aguado García
Infectious Diseases Department, 12 de Octubre University Hospital. Madrid, Spain
Gerardo Aguilar Aguilar
Department of Anesthesiology and Surgical Critical Care, Valencia Clinical University Hospital. Valencia, Spain
Benito Almirante Gragera
Infectious Diseases Department, Vall d’Hebron University Hospital. Barcelona, Spain
Francisco Álvarez Lerma
Intensive Care Department, Hospital del Mar. Barcelona, Spain
César Aragón González
Intensive Care Department, Carlos Haya University Hospital. Málaga, Spain
María Izaskun Azcárate Egaña
Intensive Care Department, Donostia University Hospital. Donostia, Spain
Marcio Borges Sa
Sepsis Unit Coordinator, Son Llàtzer Hospital. Palma de Mallorca, Spain
Mercedes Bouzada Rodríguez
Anaesthesia, Resuscitation and Pain Therapy Department, University Hospital Clinic of Santiago. Santiago de Compostela, Spain
Juan Carlos del Pozo Laderas
Intensive Care Department, Reina Sofía University Hospital. Córdoba, Spain
Carmen Fariñas Álvarez
Intensive Care Department, Marqués de Valdecilla University Hospital. Santander, Spain
Jesús Fortún Abete
Infectious Diseases Department, Ramón y Cajal University Hospital. Madrid, Spain
Beatriz Galván Guijo
Intensive Care Department, La Paz University Hospital. Madrid, Spain
José Garnacho Montero
Intensive Care Department, Virgen del Rocío University Hospital. Sevilla, Spain
José Ignacio Gómez Herreras
Department of Anesthesiology and Surgical Critical Care, Valladolid Clinical University Hospital. Valladolid, Spain
Rafael Huarte Lacunza
Pharmacy Department, Miguel Servet University Hospital. Zaragoza, Spain
Cristóbal León Gil
Intensive Care Department, Valme University Hospital. Sevilla, Spain
Rafael León López
Intensive Care Department, Reina Sofía University Hospital. Córdoba, Spain
Patricia Muñoz García
Microbiology and Infectious Diseases Department, Gregorio Marañón University Hospital. Madrid, Spain
Jordi Nicolás Picó
Pharmacy Department, Son Llàtzer Hospital. Palma de Mallorca, Spain
Pedro Olaechea Astigarraga
Intensive Care Department, Galdakao Usansolo Hospital. Vizcaya, Spain
Javier Pemán García
Microbiology Unit, La Fe University and Polythecnic Hospital. Valencia, Spain
María Luisa Pérez del Molino Bernal
Microbiology and Parasitology Unit, Santiago de Compostela University Hospital Complex. Santiago de Compostela, Spain
Leonor Periañez Párraga
Pharmacy Department, Son Espases University Hospital. Palma de Mallorca, Spain
Guillermo Quindós Andrés
Microbiology Unit, Faculty of Medicine and Dentistry, Basque Country University. Vizcaya, Spain
Jesús Rico Feijoo
Department of Anesthesiology and Surgical Critical Care, Río Hortega University Hospital. Valladolid, Spain
María Rodríguez Mayo
Microbiology Unit, A Coruña University Hospital Complex. A Coruña, Spain
Eva Romá Sánchez
Pharmacy Department, La Fe University and Polythecnic Hospital. Valencia, Spain
Isabel Ruiz Camps
Infectious Diseases Department, Vall d’Hebron University Hospital. Barcelona, Spain
Miguel Salavert Lleti
Infectious Diseases Department, La Fe University and Polytechnic Hospital. Valencia, Spain
Juan Carlos Valía Vera
Department of Anesthesiology and Surgical Critical Care, General University Hospital Consortium. Valencia, Spain
César Aldecoa Álvarez-Santullano
Department of Anesthesiology and Surgical Critical Care, Río Hortega University Hospital. Valladolid, Spain
Rosa Ana Álvarez Fernández
Department of Anesthesiology and Surgical Critical Care, Asturias Central University Hospital. Asturias, Spain
Rocío Armero Ibáñez
Department of Anesthesiology and Surgical Critical Care, Doctor Peset University Hospital. Valencia, Spain
Fernando Armestar Rodríguez
Intensive Care Department, Germans Trias i Pujol University Hospital. Badalona, Barcelona, Spain
Miguel Ángel Arribas Santamaría
Intensive Care Department, Arnau de Vilanova Hospital. Valencia, Spain
José Ignacio Ayestarán Rota
Intensive Care Department, Son Espases University Hospital. Palma de Mallorca, Spain
María Ángeles Ballesteros Sanz
Intensive Care Department, Marqués de Valdecilla University Hospital. Santander, Spain
María José Bartolomé Pacheco
Department of Anesthesiology and Surgical Critical Care, Marqués de Valdecilla University Hospital. Santander, Spain
Unai Bengoetxea Uriarte
Department of Anesthesiology and Surgical Critical Care, Basurto Hospital. Bilbao, Vizcaya, Spain
Eva Benveniste Pérez
Intensive Care Department, Germans Trias i Pujol University Hospital. Badalona, Barcelona, Spain
José Blanquer Olivas
Intensive Care Department, Valencia Clinical University Hospital. Valencia, Spain
Felipe Bobillo del Amo
Intensive Care Department, San Carlos Clinical University Hospital. Madrid, Spain
Ángel Caballero Sáez
Intensive Care Department, San Millán Hospital Complex- San Pedro Hospital. Logroño, La Rioja, Spain
Andrés Carrillo Alcaraz
Intensive Care Department, Morales Meseguer University General Hospital. Murcia, Spain
José Castaño Pérez
Intensive Care Department, Virgen de las Nieves University Hospital. Granada, Spain
Pedro Castro Rebollo
Intensive Care Department, Clínic i Provincial of Barcelona Hospital. Barcelona, Spain
Milagros Cid Manzano
Department of Anesthesiology and Surgical Critical Care, Complex of Ourense University Hospital. Ourense, Spain
Belén Civantos Martín
Intensive Care Department, La Paz University Hospital. Madrid, Spain
María Victoria de la Torre Prados
Intensive Care Department, Virgen de la Victoria University Hospital. Málaga, Spain
David Domínguez García
Department of Anesthesiology and Surgical Critical Care, Nuestra Señora de la Candelaria University Hospital. Santa Cruz de Tenerife, Spain
Juan Ramón Fernández Villanueva
Intensive Care Department, Complex of Santiago Compostela University Hospital. A Coruña, Spain
Rafael García Hernández
Department of Anesthesiology and Surgical Critical Care, Puerta del Mar University Hospital. Cádiz, Spain
Rafael Franco Llorente
Department of Anesthesiology and Surgical Critical Care, Virgen de las Nieves University Hospital. Granada, Spain
Luis Gajate Martín
Department of Anesthesiology and Surgical Critical Care, Ramón y Cajal University Hospital. Madrid, Spain
Emilio García Prieto
Intensive Care Department, Asturias Central University Hospital. Oviedo, Asturias, Spain
Pau Garro Martínez
Intensive Care Department, Granollers General Hospital. Barcelona, Spain
Carolina Giménez-Esparza Vic
Intensive Care Department, Vega Baja Hospital. Orihuela, Alicante, Spain
Ricardo Gimeno Costa
Intensive Care Department, La Fe University and Polytechnic Hospital. Valencia, Spain
Francisco Javier González de Molina Ortiz
Intensive Care Department, Mutua de Terrassa University Hospital. Barcelona, Spain
Marta Gurpegui Puente
Intensive Care Department, Miguel Servet University Hospital. Zaragoza, Spain
María José Gutiérrez Fernández
Intensive Care Department, San Agustín Hospital. Avilés, Asturias, Spain
Joaquín Lobo Palanco
Intensive Care Department, Navarra Hospital Complex. Pamplona, Navarra, Spain
Mauro Loinaz Bordonabe
Intensive Care Department, Navarra Hospital Complex. Pamplona, Navarra, Spain
Esther María López Ramos
Intensive Care Department, Príncipe de Asturias University Hospital. Alcalá de Henares, Madrid, Spain
María Pilar Luque Gómez
Intensive Care Department, Lozano Blesa Clinic University Hospital. Zaragoza, Spain
Juan Francisco Machado Casas
Intensive Care Department, Jaén Hospital Complex. Jaén, Spain
José Miguel Marcos Vidal
Department of Anesthesiology and Surgical Critical Care, Virgen Blanca Hopital Complex. León, Spain
Fernando Maroto Monserrat
Intensive Care Department, San Juan de Dios del Aljarafe Hospital. Bormujos, Sevilla, Spain
Juan Carlos Martínez Cejudo
Intensive Care Department, Infanta Elena University Hospital. Huelva, Spain
María del Carmen Martínez Ramagge
Intensive Care Department, La Línea Hospital (AGSCampo of Gibraltar). La Línea de la Concepción, Cádiz, Spain
Ignacio Moreno Puigdollers
Department of Anesthesiology and Surgical Critical Care, La Fe University and Polytechnic Hospital. Valencia, Spain
Lorena Mouríz Fernández
Department of Anesthesiology and Surgical Critical Care, Lucus Augusti University Hospital. Lugo, Spain
Luis Alberto López Olaondo
Department of Anesthesiology and Surgical Critical Care, Navarra University Clinic. Pamplona, Navarra, Spain
Sergio Ossa Echeverri
Intensive Care Department, Burgos University Hospital. Burgos, Spain
Juan Carlos Pardo Talavera
Intensive Care Department, Reina Sofía General University Hospital. Murcia, Spain
Inés María Parejo Cabezas
Department of Anesthesiology and Surgical Critical Care, San Pedro de Alcántara Hospital. Cáceres, Spain
Jorge Pereira Tamayo
Department of Anesthesiology and Surgical Critical Care, Álvaro Cunqueiro University Hospital. Vigo, Pontevedra, Spain
Miguel Ángel Pereira Loureiro
Department of Anesthesiology and Surgical Critical Care, Álvaro Cunqueiro University Hospital. Vigo, Pontevedra, Spain
Ana Pérez Carbonell
Department of Anesthesiology and Surgical Critical Care, Elche General University Hospital. Alicante, Spain
Marcos Pérez Carrasco
Intensive Care Department, Vall d’Hebron University Hospital. Barcelona, Spain
Demetrio Pérez Civantos
Intensive Care Department, Infanta Cristina University Hospital. Badajoz, Spain
María José Pérez-Pedrero Sánchez-Belmonte
Intensive Care Department, Virgen de la Salud Hospital. Toledo, Spain
David Pestaña Lagunas
Department of Anesthesiology and Surgical Critical Care, Ramón y Cajal University Hospital. Madrid, Spain
Pedro Picatto Hernández
Department of Anesthesiology and Surgical Critical Care, Asturias Central University Hospital. Oviedo, Asturias, Spain
Rosa Poyo-Guerrero Lahoz
Intensive Care Department, Son Llàtzer Hospital. Palma de Mallorca, Spain
Luis Quecedo Gutiérrez
Department of Anesthesiology and Surgical Critical Care, La Princesa University Hospital. Madrid, Spain
Roberto Reig Valero
Intensive Care Department, Castellón General Hospital. Castellón, Spain
Manuel Rodríguez Carvajal
Intensive Care Department, Juan Ramón Jiménez Hospital. Huelva, Spain
Enrique Samsó Sabé
Department of Anesthesiology and Surgical Critical Care, Hospital del Mar. Barcelona, Spain
Catalina Sánchez Ramírez
Intensive Care Department, Doctor Negrín of Gran Canaria University Hospital. Las Palmas de Gran Canaria, Spain
Margarita Sánchez Castilla
Department of Anesthesiology and Surgical Critical Care, Puerta de Hierro-Majadahonda University Hospital. Madrid, Spain
Susana Sancho Chinesta
Intensive Care Department, Doctor Peset University Hospital. Valencia, Spain
Juan Carlos Sotillo Díaz
Intensive Care Department, Gregorio Marañón General University Hospital. Madrid, Spain
José Manuel Soto Blanco
Intensive Care Department, San Cecilio University Hospital. Granada, Spain
Luis Suárez Gonzalo
Department of Anesthesiology and Surgical Critical Care, La Paz University Hospital. Madrid, Spain
Teresa Tabuyo Bello
Intensive Care Department, A Coruña University Hospital. A Coruña, Spain
Eduardo Tamayo Gómez
Department of Anesthesiology and Surgical Critical Care, Valladolid Clinic University Hospital. Valladolid, Spain
Luis Mariano Tamayo Lomas
Intensive Care Department, Río Hortega University Hospital. Valladolid, Spain
Gonzalo Tamayo Medel
Department of Anesthesiology and Surgical Critical Care, Cruces University Hospital. Bilbao, Vizcaya, Spain
Vicente Torres Pedrós
Department of Anesthesiology and Surgical Critical Care, Son Espases University Hospital. Palma de Mallorca, Spain
Montserrat Vallverdú Vidal
Intensive Care Department, Arnau de Vilanova University Hospital. Lleida, Spain
Marina Varela Durán
Department of Anesthesiology and Surgical Critical Care, Pontevedra University Hospital Complex. Pontevedra, Spain
Paula Vera Artazcoz
Intensive Care Department, Santa Creu i Sant Pau Hospital. Barcelona, Spain
María Elena Vilas Otero
Department of Anesthesiology and Surgical Critical Care, Álvaro Cunqueiro University Hospital. Pontevedra, Spain