The clinical significance of the filamentous basidiomycetes isolated from clinical samples is not always clear. Thus, these fungi have been considered environmental contaminants traditionally.
AimsTo review those clinical cases in which filamentous basidiomycetes from respiratory samples had been isolated.
MethodsThe retrospective study was carried out in a single tertiary care hospital. We recovered all culture-confirmed isolations of filamentous basidiomycetes from respiratory samples (bronchial aspirate [BAS], bronchoalveolar lavage [BAL] and sputum) analyzed between the years 2020 and 2023. Isolates were identified by ITS region sequencing.
ResultsIn six patients a filamentous basidiomycete had been isolated from a respiratory sample. The species identified were all different: Fomitopsis sp. (BAS), Trametes ljubarskyi (BAL), Stereum gausapatum (BAS), Porostereum spadiaceum (BAS), Phlebia subserialis (sputum) and Inonotus levis (BAL). All the patients were immunosuppressed or had an underlying disease with pulmonary involvement. None of them received any specific antifungal treatment (in relation with the fungus isolated) and all six improved clinically and were discharged.
ConclusionsThe isolation of filamentous basidiomycetes in these patients had uncertain clinical significance. However, the isolation of any filamentous basidiomycete in respiratory samples from immunosuppressed patients or patients with chronic pulmonary disease is an emerging situation that should be carefully assessed in the context of chronic allergic episodes or suspicion of invasive fungal infections.
La importancia clínica de los basidiomicetos filamentosos procedentes de muestras clínicas no siempre es clara. Por ello, estos hongos se han considerado tradicionalmente como contaminantes ambientales.
ObjetivosDescribir las características de los pacientes con aislamientos de basidiomicetos filamentosos en muestras respiratorias para intentar aclarar el significado clínico de estos hallazgos.
MétodosSe realizó un estudio retrospectivo en nuestro hospital de tercer nivel; fueron incluidos pacientes con el aislamiento de un basidiomiceto filamentoso confirmado en cultivo a partir de una muestra respiratoria (aspirados bronquiales [BAS], lavados broncoalveolares [BAL] y esputos) procesadas entre los años 2020 y 2023. Realizamos la identificación molecular del aislamiento mediante la secuenciación de la región ITS.
ResultadosEn seis pacientes se obtuvo un aislamiento de basidiomiceto filamentoso de una muestra respiratoria, y los seis aislamientos pertenecían a diferentes géneros: Fomitopsis sp. (BAS), Trametes ljubarskyi (BAL), Stereum gausapatum (BAS), Porostereum spadiaceum (BAS), Phlebia subserialis (esputo) e Inonotus levis (BAL). Todos los pacientes sufrían inmunosupresión o alguna enfermedad de base con afectación pulmonar. Ninguno de ellos recibió tratamiento antifúngico específico (en relación con el aislamiento recuperado de la muestra) y finalmente fueron dados de alta tras la mejoría clínica.
ConclusionesLos aislamientos de basidiomicetos filamentosos en nuestros pacientes tuvieron un significado clínico incierto. Sin embargo, en los pacientes inmunodeprimidos o con enfermedades pulmonares crónicas, el aislamiento de un basidiomiceto filamentoso en el tracto respiratorio inferior representa una situación emergente que debe evaluarse cuidadosamente en el contexto de un episodio alérgico crónico o ante la sospecha de una infección fúngica invasiva.
Filamentous basidiomycetes isolated from clinical samples usually grow as nonsporulating cottony white colonies.5 Their clinical significance is not clear11 and, traditionally, have been considered environmental contaminants, although in some cases they have been reported as the cause of invasive fungal infections in immunocompromised patients (hematological malignancies, solid-organ transplant recipients, neutropenic patients, among others).3–10 Some species, such as Hormographiella aspergillata and Volvariella volvacea, have been associated with case fatality.10,12 Morphological identification is not possible in many cases due to the lack of both sporulation and distinctive morphological features,5 so the reference method is molecular identification.11 This is usually done by sequencing the ribosomal operon internal transcribed spacer regions (ITS) or the D1/D2 domain of the large subunit ribosomal DNA.2
In order to gain insight into the clinical significance of the presence of these fungi in the respiratory system, we review the clinical characteristics of patients in our hospital whose respiratory samples had yielded the growth of a filamentous basidiomycete.
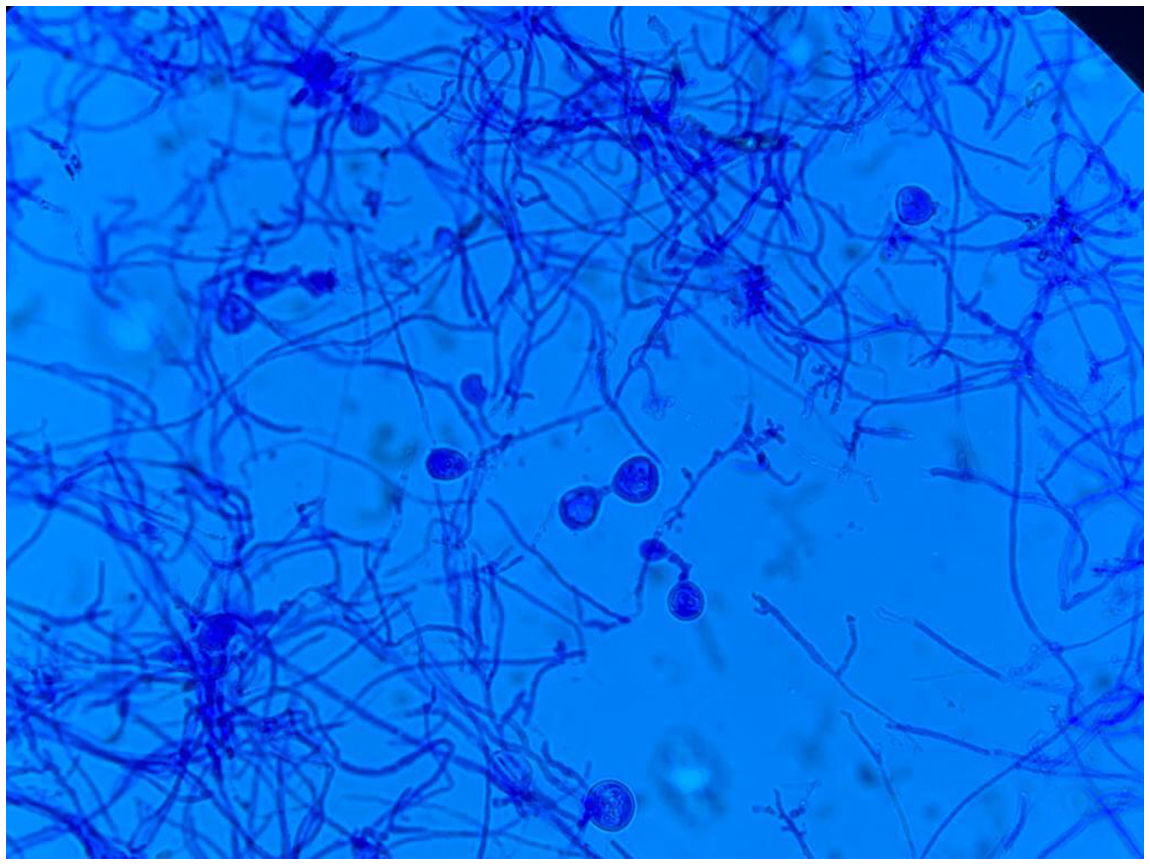
A retrospective study including all adult patients that had a filamentous basidiomycete isolated from a respiratory sample between February 2020 and February 2023 was carried out. Respiratory samples were bronchoalveolar aspirate (BAS), bronchoalveolar lavage (BAL) and sputum. Patients demographic and clinical data were recovered from the clinical records; microbiological data were recovered from the Microbiology Department database. Respiratory samples had been cultured in conventional media for bacterial and fungal analyses. Saboraud dextrose agar with chloramphenicol and gentamicin (Becton Dickinson, Franklin Lakes, NJ) was used for fungal culture, and plates were incubated at 30°C and 37°C for 7 days. When the culture yielded atypical filamentous fungi that could not be identified by mass spectrometry or conventional methods (morphology, lactophenol blue stain), molecular identification was done. For PCR amplification of the ITS1 and ITS2 regions, the primers ITS1 and ITS4 (5′-TCCGTAGGTGAACCTGCGG-3′ and 5′-TCCTCCGCTTATTGATATGC-3′) were used.13 PCR products were sequenced with ABI 3130XL or SeqStudio analyzers (Applied Biosystems, Foster City, CA). The sequences were cleaned and assembled with Sequencing Analysis software (Applied Biosystems) and BLAST-searched against GenBank and MycoBank public databases.
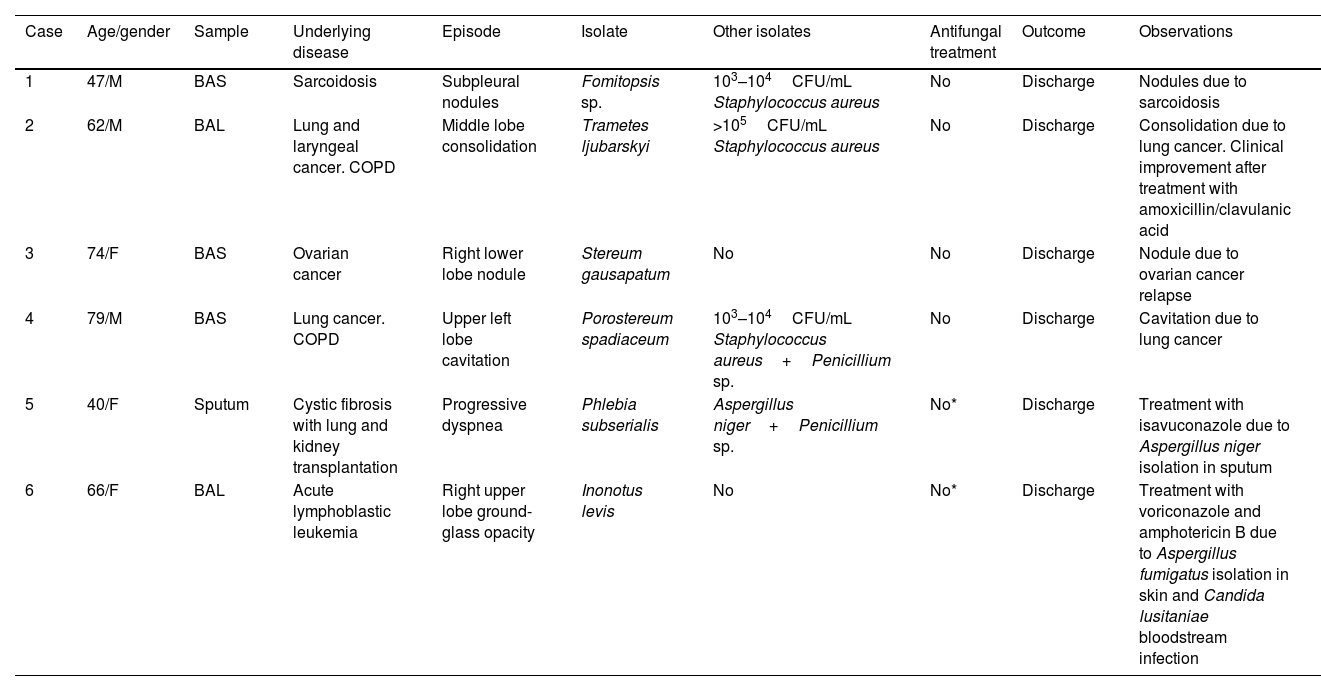
During the study period, filamentous basidiomycetes were isolated from the respiratory samples of six patients. In all the cases a single basidiomycete species was obtained from a single sample. Demographic, clinical and microbiological characteristics are shown in Table 1. Three patients were male and three females with a median age of 64 years (IQR 74-47). All the patients were immunosuppressed or had an underlying disease with pulmonary involvement (cancer, cystic fibrosis, leukemia and sarcoidosis). In five patients, BAS and BAL samples were obtained by bronchoscopy performed to study nodules, consolidations and other lung lesions seen by imaging techniques. In the sixth patient, a spontaneous sputum was obtained. The six samples yielded six different species: Fomitopsis sp. (BAS), Trametes ljubarskyi (BAL), Stereum gausapatum (BAS), Porostereum spadiaceum (BAS), Phlebia subserialis (sputum) and Inonotus levis (BAL). All the isolates had moderate-abundant growth, however direct microscopic examination of the samples was negative in all of them. A lactophenol blue stain of the Inonotus levis colonies (case number 6) is shown in Fig. 1. Four patients had mixed cultures with bacteria or other fungal species: Staphylococcus aureus in two cases, S. aureus and Penicillium sp. in another, and Aspergillus niger and Penicillium sp. in the fourth one. In the last two patients an antifungal treatment against the non-basidiomycete fungal isolate was administered during the episode. No antifungal therapy was administered specifically to treat the basidiomycetes. Finally, all patients recovered and were discharged.
Demographic, clinical and microbiological characteristics of patients with filamentous basidiomycetes isolates in respiratory samples.
| Case | Age/gender | Sample | Underlying disease | Episode | Isolate | Other isolates | Antifungal treatment | Outcome | Observations |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 47/M | BAS | Sarcoidosis | Subpleural nodules | Fomitopsis sp. | 103–104CFU/mL Staphylococcus aureus | No | Discharge | Nodules due to sarcoidosis |
| 2 | 62/M | BAL | Lung and laryngeal cancer. COPD | Middle lobe consolidation | Trametes ljubarskyi | >105CFU/mL Staphylococcus aureus | No | Discharge | Consolidation due to lung cancer. Clinical improvement after treatment with amoxicillin/clavulanic acid |
| 3 | 74/F | BAS | Ovarian cancer | Right lower lobe nodule | Stereum gausapatum | No | No | Discharge | Nodule due to ovarian cancer relapse |
| 4 | 79/M | BAS | Lung cancer. COPD | Upper left lobe cavitation | Porostereum spadiaceum | 103–104CFU/mL Staphylococcus aureus+Penicillium sp. | No | Discharge | Cavitation due to lung cancer |
| 5 | 40/F | Sputum | Cystic fibrosis with lung and kidney transplantation | Progressive dyspnea | Phlebia subserialis | Aspergillus niger+Penicillium sp. | No* | Discharge | Treatment with isavuconazole due to Aspergillus niger isolation in sputum |
| 6 | 66/F | BAL | Acute lymphoblastic leukemia | Right upper lobe ground-glass opacity | Inonotus levis | No | No* | Discharge | Treatment with voriconazole and amphotericin B due to Aspergillus fumigatus isolation in skin and Candida lusitaniae bloodstream infection |
BAL: bronchoalveolar lavage; BAS: bronchial aspirate; COPD: chronic obstructive pulmonary disease; F: female; M: male.
Basidiomycota molds, as other filamentous fungi, can colonize chronically the respiratory tree in patients with lung disorders or immunosuppression.11 This may cause a sensitization to fungal antigens and the development of hypersensitivity disorders such as allergic sinusitis, allergic asthma, and chronic eosinophilic pneumonia, among others.6 Invasive fungal infections have been reported,3,10,12 though they are uncommon. Some reports have suggested a link between the use of caspofungin and the development of secondary infections by basidiomycetes in highly immunosuppressed hosts.7 One of our patients had cystic fibrosis and had received isavuconazole to treat Aspergillus niger in the sputum, even though the clinical significance was unclear. Another patient suffered from leukemia and had received voriconazole and amphotericin B to treat Aspergillus fumigatus in skin lesions and candidemia by Candida lusitaniae, but none of the patients had received caspofungin previously.
The combined use of ITS and D1/D2 regions has been reported as a protocol bearing higher identification rates for filamentous basidiomycetes than ITS alone.8,9 Except for Fomitopsis sp., which was identified to the genus level only in both GenBank and MycoBank databases, the rest of the isolates were identified to the species level using ITS sequencing. This confirms that the databases have still certain limitations, in particular concerning basidiomycetes.1,9
The isolation of filamentous basidiomycetes in respiratory samples is an emerging phenomenon in clinical mycology laboratories. Its clinical relevance is unknown. However, an accurate identification of these species from respiratory samples is important to trace outbreaks and detect potential sources, in particular when assessing this type of results in complex patients with risk factors for developing an invasive fungal infection.
In conclusion, we have described the isolation of filamentous basidiomycetes from the respiratory samples of patients with immunosuppression or respiratory diseases, but the clinical significance of these findings is still uncertain. In addition, our study has certain limitations due to the retrospective design and the single-center setting that limited the number of cases. Nevertheless, the isolation of a filamentous basidiomycete in the lower respiratory tract of immunosuppressed patients or patients with chronic pulmonary diseases should be carefully assessed due to the chance of developing a chronic allergy or fungal invasive infection.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone of the authors has a conflict of interest to disclose.