Fungal infections have been commonly diagnosed in individuals with advanced HIV disease. Cryptococcosis, pneumocystosis, and histoplasmosis are the most frequent systemic mycoses in people suffering from HIV/AIDS.
Case reportWe report a case of multiple fungal infections in an advanced AIDS-patient. A 33-year-old HIV-positive man from Brazil was hospitalized due to diarrhea, dyspnea, emaciation, hypoxemia, extensive oral thrush, and a CD4+ T lymphocyte count of 20cells/mm3. Honeycombed-structures consistent with Pneumocystis jirovecii were observed by direct immunofluorescence in induced sputum. Cryptococcus neoformans was recovered from respiratory secretion and cerebrospinal fluid cultures. Histopathology of the bone marrow also revealed the presence of Histoplasma capsulatum. Molecular assays were performed in a sputum sample. Nested-PCR confirmed the presence of P. jirovecii and H. capsulatum; qPCR multiplex was positive for C. neoformans and H. capsulatum. With the treatment of antifungal drugs the patient progressed satisfactorily.
ConclusionsThe diagnosis of several systemic mycoses demonstrates the vulnerability of advanced AIDS-patients. Thus, the detection of AIDS cases in the early stages of infection is necessary for a prompt and adequate introduction of HAART therapy, and the use of prophylaxis to control opportunistic infections.
Las infecciones fúngicas se han diagnosticado comúnmente en individuos con enfermedad avanzada por VIH. La criptococosis, la neumocistosis y la histoplasmosis son las micosis sistémicas más frecuentes en personas con VIH/sida.
Caso clínicoEn este trabajo se describe un caso de múltiples infecciones fúngicas en un paciente con sida avanzado. Un hombre de 33 años, brasileño, con serología positiva para VIH, fue hospitalizado con pérdida de peso, diarrea, disnea, caquexia, hipoxemia, extensa candidiasis oral y recuento de linfocitos CD4+ de 20 cél./mm3. La inmunofluorescencia directa puso de manifiesto estructuras típicas compatibles con Pneumocystis jirovecii. En el cultivo de las muestras de secreción respiratoria y de líquido cefalorraquídeo creció Cryptococcus neoformans. En el análisis histopatológico de una muestra de médula ósea se observó Histoplasma capsulatum. Se llevaron a cabo ensayos de marcadores moleculares en una muestra de esputo. Se realizó un ensayo de PCR anidada que fue positivo para P. jirovecii y H. capsulatum, y una qPCR multiplex que fue positiva para C. neoformans e H. capsulatum. Con un tratamiento con antimicóticos el paciente evolucionó satisfactoriamente.
ConclusionesEl diagnóstico de las micosis sistémicas demuestra la vulnerabilidad de los pacientes con sida avanzado. El diagnóstico de la infección por VIH en sus etapas iniciales es fundamental para la introducción precoz y adecuada de la terapia antirretroviral altamente activa y la profilaxis de las infecciones oportunistas.
The highly active antiretroviral therapy (HAART) has considerably changed the characteristics of the HIV epidemic. However, many patients still present to health services with advanced HIV-related immunosuppression, particularly in developing countries.3 Although pulmonary tuberculosis remains as the main opportunistic infection in HIV-patients, systemic mycoses have been commonly diagnosed in this population, particularly in individuals who live in endemic areas of these mycoses.6,16
In the early 1980s, Pneumocystis jirovecii pneumonia was the most common pulmonary infection associated with advanced HIV disease. However, cryptococcal meningitis (CM) accounts nowadays for the majority of worldwide deaths from HIV-related fungal infection.3,16 In the sub-Saharan Africa and Latin America, cryptococcosis, pneumocystosis, and histoplasmosis are the most frequent systemic mycosis in people with HIV/AIDS (PHA).7,8 These infections are acquired by inhalation of propagules, and can occur as an acute pulmonary infection or as an endogenous reactivation of a latent infection in immunocompromised individuals.12
P. jirovecii infection is usually characterized by interstitial pneumonia leading to respiratory failure.3,12Cryptococcus and Histoplasma capsulatum infections can affect only the lungs. However, systemic dissemination to the central nervous system and lymphomonocytic system can also occur, leading to several and fatal cases of CM or disseminated histoplasmosis, respectively.8,16 Here we report a case of multiple fungal infections in an individual with advanced HIV disease.
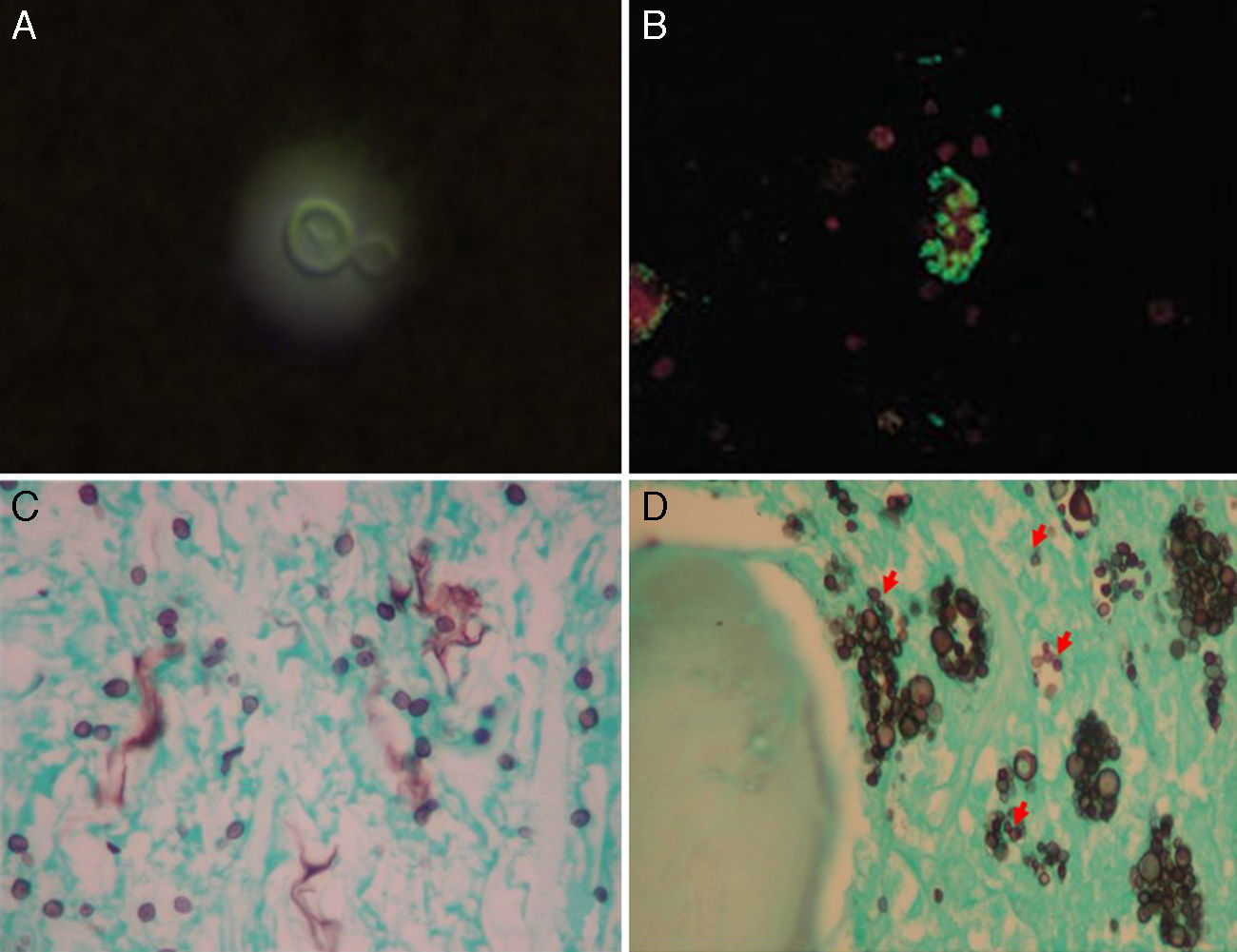
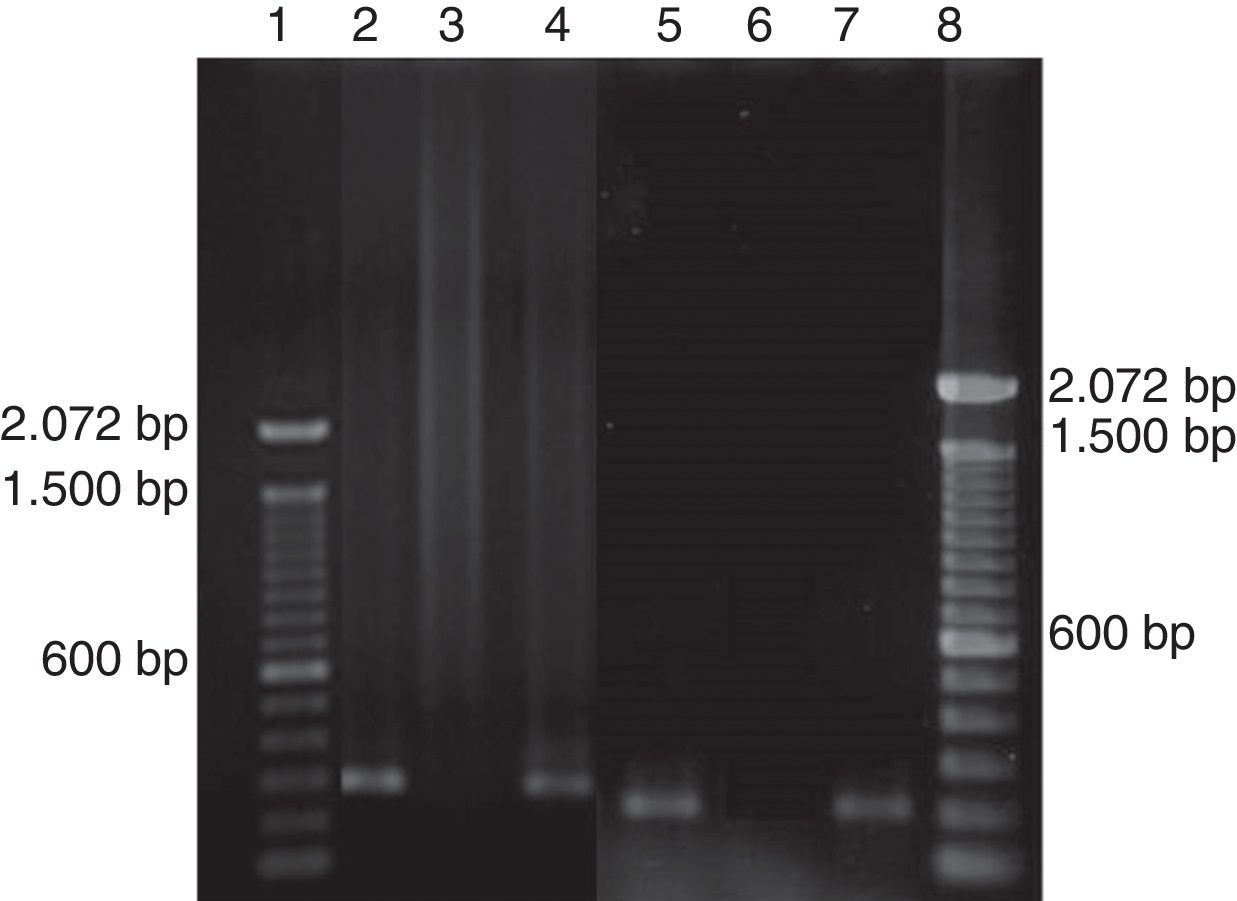
Case reportThe 33-year-old, HIV-positive male patient from Brazil was hospitalized in August 2013 due to diarrhea and dyspnea. At the moment of hospitalization, the patient presented emaciation, tachypnea, hypoxemia, extensive oral thrush, and a CD4+ T lymphocyte count of 20cells/mm3. Chest tomography showed ground-glass opacity, particularly in the lung apices. The induced sputum sample was submitted to microbiological tests. Microscopical examination of a cerebrospinal fluid sample was made in order to diagnose or rule out CM. India ink preparation confirmed the presence of yeast-like Cryptococcus (Fig. 1A). Direct immunofluorescence showed the presence of typical honeycombed-structures compatible with P. jirovecii (Fig. 1B). Culture of respiratory secretion on agar Sabouraud and modified Middlebrook 7H9 broth base (MGIT – Mycobacteria Growth Indicator Tube) showed the growth of Cryptococcus sp., and Mycobaterium tuberculosis complex, respectively. The species Cryptococcus neoformans was identified by Cryptococcus inoculum on canavanine-glycine-bromothymol blue (CGB) medium. The patient received a treatment with trimethoprim-sulfametoxazole, amphotericin B, fluconazole, and tuberculostatic drugs. After 20 days of hospitalization, HAART was started with tenophovir, lamivudine, lopinavir and ritonavir. Immunological improvement (CD4+ T lymphocytes count=291cells/mm3) was observed in October 2013. However, the patient developed intermittent fever, pancytopenia, hepatomegaly and splenomegaly. In the examination of induced sputum sample, yeast cells with single budding, compatible with H. capsulatum, were observed (Fig. 1C). Bone-marrow histopathology showed fungal structures compatible with H. capsulatum and C. neoformans stained by Gomori-Grocott silver stain (Fig. 1D). Molecular assays were also performed in the sputum for diagnostic confirmation. Nested-PCR confirmed the presence of P. jirovecii19 and H. capsulatum5 (Fig. 2). A multiplex real-time PCR assay (qPCR Multiplex)9 for detecting simultaneously P. jirovecii, C. neoformans and H. capsulatum was performed, and a positive result for C. neoformans and H. capsulatum was obtained. After four months of hospitalization, the patient improved satisfactorily and was discharged.
Fungal agents. (A) India ink preparation of cerebrospinal fluid showing an encapsulated yeast-like Cryptococcus neoformans (1000x). (B) Direct immunofluorescence in induced sputum showing the honeycombed-structures consistent with Pneumocystis jirovecii (400x). (C) Gomori-Grocott silver stain in induced sputum showing small fungal cells consistent with Histoplasma capsulatum (400x). (D) Bone marrow histopathology showing yeasts consistent with Histoplasma capsulatum (arrows) and Cryptococcus neoformans (Gomori-Grocott silver stain, 400x).
It is estimated that a late diagnosis of HIV infection can occur in up to 60% of all patients.2 In Brazil, although the health public policies have considerably contributed to a most extensive access of the population to serological tests and HAART, with remarkable impact on the mortality rate, it is estimated that approximately 40,000 new cases of HIV infection still occur annually.14 Therefore, the late diagnosis is still a reality, which favors the identification of AIDS cases in an advanced stage (CD4+ T lymphocyte count below 200cells/mm3 or AIDS clinical symptoms).10
It is estimated that CM affects almost one million PHA with approximately 650,000 deaths per year.16 Pneumocystosis and histoplasmosis affect to more than 300,000 PHA annually.6,7 In Brazil, the systemic mycoses are not subjected for epidemiologic surveillance. The real prevalence and incidence of these diseases are unknown. However, the main fungal infections associated with AIDS mortality in Brazil are cryptococcosis, candidiasis and histoplasmosis.17 To date, only a seroprevalence study has been performed in a histoplasmosis endemic area of northeastern Brazil in PHA with CD4+ count >350cells/mm3, by means of a skin test with histoplasmin. The results showed a histoplasmosis prevalence of 12% in this region.4
Fungal infections also are favored by immune response inflammatory syndrome (IRIS), which is due to an intense and exacerbated inflammatory response associated with the immune reconstitution caused by HAART.18 A CD4+ T lymphocyte count below 100cells/mm3, a rapid decrease in viral load and the institution of HAART during the first month of treatment of opportunistic infections are the risk factors strongly associated with IRIS.13 It is characterized by paradoxical clinical deterioration, when the patient develops a worsening of the infection under treatment or develops new opportunistic infections. Fungi most commonly related to IRIS are C. neoformans and H. capsulatum.11,15 In the case herein reported, disseminated histoplasmosis was diagnosed after the start of HAART and, thus, we believe this mycosis occurred due to IRIS.
The diagnosis of systemic mycosis is time consuming and laborious because usually requires the identification of the fungus in biological samples by culture, histopathological or direct examination with proper stainings.12 The lack of proper facilities and medical supplies to perform the diagnosis of these opportunistic fungal infections such as specific culture media, specialized professionals to perform invasive procedures (lumbar puncture and bone marrow biopsy) or immunofluorescence techniques, may delay the diagnosis of these infections and, therefore, avoid the appropriate treatment. Molecular techniques show improved sensitivity and specificity when compared to conventional diagnostic methods; nevertheless, these tests are only standardized in some research institutions and are not commercially available.1
In conclusion, the detection of several systemic mycoses demonstrates the vulnerability of advanced AIDS-patients. The introduction of HAART and primary prophylaxis to opportunistic infections has promoted better quality of life in these individuals. Thus, it is necessary to improve the detection of HIV infection in the early stages. In addition, it is indispensable a major investment in health services, laboratories and reference hospitals for the care of PHA to improve the time of diagnosis, allowing a correct and adequate treatment of these patients.
Conflict of interestThe authors declare that there is no conflict of interest among them or with any financial organization regarding the material discussed in the present manuscript.
This work was supported by FAPERJ/Rio de Janeiro, Brazil [grant proc. E-26/110.619/2012] and PAPES VI – CNPq/Fiocruz [grant proc. 407693/2012-2]. R.M.Z.-O. was supported in part by CNPq [304976/2013-0] and FAPERJ [E-26/103.157/2011].