To assess the status of the sexual education approach with spina bifida (SB) patients.
Materials and methodsAn online survey was sent to 223 pediatric urologists from Latin countries, all contacted using email or mobile messaging software. There were 12 questions about participants’ demographic characteristics and SB-specific care topics. Data was collected from January 2019 to January 2020. Checklist for reporting results of internet e-survey (CHERRIES) guidelines were followed to ensure the quality of this study.
ResultsWe received 101 valid answers from participants practicing in seven different countries. Among these, 98.4% confirmed that sexuality in the SB population is considered relevant, nevertheless it is only evaluated by 62.5%. Transitional urologists discuss sexuality more often than those whose practice consists solely of pediatric patients (70% vs. 50%). Basic surgeon training (urologist vs. pediatric surgeon), age, part or full-time pediatric urology practice and country of participants were of no statistically different influence inrates of approach to sexuality.
ConclusionOur study demonstrates that pediatric urologists are insufficiently addressing sexuality in SB patients. Those who practise transitional urology show higher rates of approach to sexuality with SB patients, which suggests this is an important model of care.
Evaluar el estatus del abordaje de la salud sexual en pacientes con espina bífida (EB).
Materiales y métodosSe envió una encuesta online a 223 urólogos pediátricos de países latinos, contactados mediante correo electrónico o software de mensajería móvil, en la que se incluían 12 preguntas sobre las características demográficas de los pacientes y cuestiones sobre cuidados específicos de la EB. Los datos fueron recabados entre enero de 2019 y enero de 2020, y se siguieron las directrices sobre listas de comprobación para el reporte de resultados de encuestas por internet (CHERRIES) para garantizar la calidad de este estudio.
ResultadosRecibimos 101 respuestas válidas de los participantes que ejercían en 7 países diferentes. De entre ellos, el 98,4% confirmó que la sexualidad en la población con EB se considera relevante, aunque sin embargo se evalúa únicamente en el 62,5% de los casos. Los urólogos transicionales debaten la sexualidad más a menudo que aquellos cuya práctica consiste únicamente en pacientes pediátricos (70 vs. 50%). La formación en cirugía básica (urólogo vs. cirujano pediátrico), la edad, la práctica urológica a tiempo parcial o completo y el país de los participantes no tuvieron una influencia estadística diferente en las tasas de abordaje de la sexualidad.
ConclusiónNuestro estudio demuestra que los urólogos pediátricos no abordan suficientemente la sexualidad en los pacientes con EB, y que aquellos que practican la urología transicional reflejan unas mayores tasas de abordaje de esta cuestión con los pacientes con EB, lo cual sugiere que se trata de un modelo importante de cuidados.
The life expectancy of spina bifida patients (SB) has increased as a result of improved medical care. Therefore, adult life issues such as sexuality have become growing concerns among this population.1 There is consistent data associating urological complications of SB with negative effects on sexuality, specially urinary incontinence.1,2 Nevertheless, many patients are sexually active as some papers have reported that up to 40% of SB adults present regular sexual activity.1,3
Several studies reveal that most of these patients only receive sexual education from school or by parents, which seems not enough since SB is a complex condition that impacts their sexual and reproductive function.4,5 The need for more information given by the physician was expressed in different studies using heterogeneous SB population, indicating that this issue could be improperly approached during medical care.4–6
Therefore, we decided to undertake an online survey among pediatric urologists to assess if there is a disconnect between what patients say they experience and what providers think they are doing. We also analyzed if there is correlation between different medical practices and the rates of sexual approach.
Materials and methodsAn online invitation to a survey was sent to 223 physicians from the Sociedad Iberoamericana de Urología Pediatrica (SIUP) and Brazilian School of Pediatric Urology (BSPU). After both institutional review board approval, invitations were made using these societies mailing lists providing a weblink to a free-basis query (Google Forms). The authors also announced the study using mobile messaging software with the same weblink in the oficial BSPU and SIUP Whatsapp groups. It consisted of a non-open voluntary survey that requested individual registration with one personal email, preventing duplicate responses. A informed consent was displayed in the invitation mail, with a full description of the study purpose, authors identification, the approximate length of 5min to fulfill the survey and that data would be stored privately with authors. Data was collected from January 2019 to January 2020 with three invitation attempts during this period. Checklist for reporting results of internet e-surveys (CHERRIES) guidelines were followed to ensure que quality of this study.7
Within this survey there was a total of 12 questions, which included participants demographics (i.e. country, age, years of practice), medical formation (i.e. basic formation in pediatric surgery that performs urology vs. urologist that performs pediatric urology), medical practice (i.e. private or academic hospital; transitional urologist or strictly pediatric urologist) and SB-specific care topics (Appendix). Survey was available in three different languages: Spanish, Portuguese and English. Participants who did not work with SB patients were excluded from analysis.
The following statistical tests utilized in the study were Chi-square, Fischer‘s exact test and ANOVA, being analyzed with SPSS (SPSS Statistics for Windows, Version 21.0).
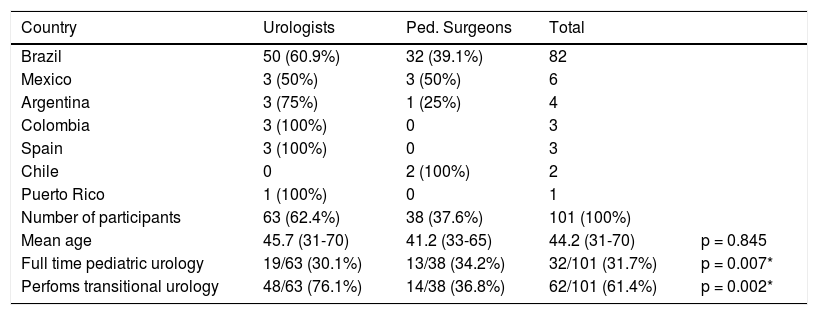
ResultsA total of 105 individuals completed the survey which represented a 47.1% response rate. Four participants informed that do not have SB patients and were excluded from the analysis. Pediatric urologists practicing in seven different countries have fulfilled the survey (in order of prevalence: Brazil, Mexico, Argentina, Colombia, Spain, Chile and Puerto Rico). The median age of responders was 44.2 years (range 31–70), being 63 (62.4%) urologists and 38 (37.6%) pediatric surgeons dedicated to pediatric urology. Participants work with pediatric urology in more than 50% of their clinical office in 75.2% (76/101), being fully dedicated to this specialty in 31.7% (32/101). A total of 62 (61.4%) participants considered that they do practice transitional urology, being this more frequent among urologists than pediatric surgeons (76.1% vs. 36.8% p=0.002) (Table 1). Although 98% (99/101) of participants who work with SB agreed that sexuality was a relevant topic of discussion, only 62.4% (63/101) actually talk about it with the SB-patients. Quality of life (QOL), however, was discussed by 85.1% (86/101) of physicians, being significantly more explored than sexuality (85.1% vs.62.4% p=0.001). The basic surgeon formation (urologist vs. pediatric surgeon) did not influence statistically with differences in the sexuality or QOL approach rates. Transitional urologists debate sexuality more frequently than those who do not follow up patients into adulthood (69.3% vs. 48.7% p=0.043). There are only 11 (10.9%) doctors that work exclusively in a private manner compared to 90 (89.5%) in academic institutions. Participants who work in academic hospitals approached sexuality and quality of life statistically more than those who work exclusively in private hospitals (sexuality: academic 67.8% vs. private 27.3% p=0.018; quality of life: academic 91.1% vs. private 54.5% p=0.001) (Table 2). One should keep in mind that there are important group size differences in this last analysis. There were no differences in sexuality approach rates comparing age, partial or full-time dedication in pediatric urology and country of participants.
Characteristics of pediatric urologists who follow SB-patients in the study.
| Country | Urologists | Ped. Surgeons | Total | |
|---|---|---|---|---|
| Brazil | 50 (60.9%) | 32 (39.1%) | 82 | |
| Mexico | 3 (50%) | 3 (50%) | 6 | |
| Argentina | 3 (75%) | 1 (25%) | 4 | |
| Colombia | 3 (100%) | 0 | 3 | |
| Spain | 3 (100%) | 0 | 3 | |
| Chile | 0 | 2 (100%) | 2 | |
| Puerto Rico | 1 (100%) | 0 | 1 | |
| Number of participants | 63 (62.4%) | 38 (37.6%) | 101 (100%) | |
| Mean age | 45.7 (31-70) | 41.2 (33-65) | 44.2 (31-70) | p = 0.845 |
| Full time pediatric urology | 19/63 (30.1%) | 13/38 (34.2%) | 32/101 (31.7%) | p = 0.007* |
| Perfoms transitional urology | 48/63 (76.1%) | 14/38 (36.8%) | 62/101 (61.4%) | p = 0.002* |
* statistically significant value
Sexuality and quality of life approach on the SB patient.
| Discuss QOL | Discuss Sexuality | Considers sexuality relevant in SB | |
|---|---|---|---|
| All participants(101) | 86/101 (85.1%) | 63/101 (62.4%) | 99/101 (98%) |
| Surgical formation | |||
| Urologist(63) | 52/63 (82.5%) | 38/63 (60.3%) | 96.8% (61/63) |
| Ped. Surg.(38) | 34/38 (89.5%) | 25/38 (65.8%) | 100% (38/38) |
| p-value | p = 0.472 | p = 0.453 | p = 0.612 |
| Transitioning | |||
| Trans. Urol.(62) | 56/62 (90.3%) | 43/62 (69.3%) | 62/62 (100%) |
| Only Ped. Urol.(39) | 31/39 (79.5%) | 19/39 (48.7%) | 37/39 (94.8%) |
| p-value | p = 0.238 | p = 0.043* | p = 0.373 |
| Type of Hospital | |||
| Academic(90) | 82/90 (91.1%) | 61/90 (67.8%) | 64/90 (71.1%) |
| Private only(11) | 6/11 (54.5%) | 3/11 (27.3%) | 7/11 (63.7%) |
| p-value | p = 0.001** | p = 0.018** | p = 0.540 |
* Statistically significant value
** Although p < 0.05 the low number of participants in the “private hospital only” must be considered
A greater survival of SB patients occurs due to medical and multidisciplinary care advances, allowing that 70–80% of these patients reach adulthood nowadays.1,8 However, the SB population suffers multiple adversities during transition from childhood to adult such as urinary incontinence, depression and sexual dysfunction.9 Pediatric urologists tend to focus in the bladder management and renal function preservation, being sexuality and infertility overlooked.10 Furthermore, since SB was traditionally treated as a pediatric condition, individuals have been infantilized by caregivers making it difficult to offer a proper sexual care.11 Adult SB males present higher rates of erectile dysfunction, retrograde ejaculation and diminished perineal sensation leading to worst orgasmic satisfaction.11,5 Female SB patients also present impaired sexual function in the orgasmic/pleasure, arousal, desire, satisfaction, receptivity and frequency domains.12 Different SB-population studies from diverse regions demonstrated a common complaint from patients: lack of sexual information and approach from caregivers. These studies revealed that only 0% to 39% of the SB adult patients have received any sort of sexual counseling from their physicians.10,13,14 This frequent claim has motivated this study, when we decided to evaluate how does the pediatric urologist approaches sexuality with SB patients and if there are factors influencing that.
Most of pediatric urologists have considered sexuality a important topic to discuss, however just over half of them admitted to talk about this with patients. Regardless the basic specialty (urologist or pediatric surgeon), clearly there is a need to improve the rates of sexual approach during medical appointments, especially because these are the most prepared physicians to council and treat sex issues. Even thought urologists seem to have a more frequent contact with sexual dysfunction due to their initial formation with the general adult population, in our study the pediatric surgeons asked the patients more frequently about sex and quality of life despite this difference was not statistically significant. Streur et al. performed a provider-perspective study that analyzed how pediatric urologists deal with this. Participants claimed that they had no training and did not feel prepared to provide sexual and reproductive health education for SB patients. They stated important barriers such as lack of knowledge on SB specific modifications of sexual physiology and the presence of the parents in the office making uncomfortable to start such a delicate topic. In the meantime the pediatric urologists revealed that long-term relationship with the patient and family facilitates discussing sex and fertility issues.15
The continued need for care in the SB patients and many other chronic urological conditions have lead to the development of transition clinics. Transitioning from adolescence to adulthood is a challenging period for SB patients and their family, which is best managed by a multidisciplinary team that treats patients in an integrative way and, despite different models of transition clinics, often is the pediatric urologist who has the major role as coordinator.16,17 Although just a few centers have described data on the benefits of transitioning, there are reports of important changes in the bladder management as much as in 70% of patients when referred to transitional urology centers.18 Data from patient-based surveys have demonstrated overall satisfaction with transitional programs, being a key factor giving patients more time and written information during a medical appointment.19,20 In our study, transitional urologists more commonly approached sexuality and quality of life with their patients, which is consistent with this proposal and emphasizes the importance of this model of care. Also academic providers showed better rates in our research which could reflect the fact that transition clinics are located mainly in multidisciplinary educational centers.
There are some potential limitations in this study. As a survey we depend in how the participants interpret our questions, therefore some definitions such as transitional urology, sexual discussion and QOL could find different meanings. The low number of participants in the “private hospital only” group compromises this information and should also be considered a limiting factor.
ConclusionAlthough 98% of participants agreed that sexuality was a relevant topic of discussion, only 62.4% actually talk about it with patients of caregivers. Our results show that there is a need to improve communication between the pediatric urologist and SB patients about sex and fertility. Those who perform transitional urology show higher rates of approach of sexuality with SB patients, which suggests this is a important model of care.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestNone declared.