To determine the factors affecting the success of distal hypospadias repair in adults.
Material and methodsMedical records of adult patients who underwent distal hypospadias repair in our clinic were reviewed. Patient's age, external urethral meatus location, hypospadias status, anesthesia type, diversion type, nelaton diameter and surgeons were recorded as factors affecting surgery success. Only patients, operated with tubularisation incised plate urethroplasty (TIPU) technique, were included. Results were classified as successful, stricture, fistula and slough. We compared the factors affecting the success.
SPSS 16.0 were used for statistical assessment and logistic regression analysis was used to determine success. p<0.05 was considered to show statistical significance.
ResultsOne hundred and eight patients underwent distal hypospadias repair in our clinic. Mean age was 21.44±2.0. 38 patients had distal penile, 67 patients had subcoronal, 2 patients had coronal and 1 patient had glandular hypospadias. Eighty eight patients had primary, 12 secondary, 5 tertiary and 3 cripple hypospadias. Seventy eight patients underwent TIPU under local anesthesia, and 30 patients underwent under spinal anesthesia. Suprapubic catheter was used in 92 patients and transurethral catheter was used in 16 patients. Sixteen different surgeons performed the operations. Seventy operations were successful. Three stricture, 24 fistula, and 11 slough were determined. Overall success rate was 64.81%. Patient's age, external urethral meatus location, anesthesia type, diversion type, nelaton diameter and the surgeon difference did not affected surgical outcomes. Only hypospadias status (primary/redo) affected the success (p=0.037).
ConclusionThe only factor affecting surgical outcomes of distal hypospadias repair in adults seems to be hypospadias status. It might be due to the lack of second layer in the redo operations.
Determinar los factores que influyen en el éxito de la reparación de hipospadias distal en adultos.
Materiales y métodosSe revisaron las historias clínicas de los pacientes adultos que se sometieron a reparación de hipospadias distal en nuestra clínica. Los siguientes factores se consideraron factores que afectan al éxito de la operación:la edad del paciente, la localización del meato uretral externo, el estado de hipospadias, el tipo de anestesia, el tipo de desvío, el diámetro nelaton y los cirujanos. Solo se tuvieron en cuenta los pacientes operados con la técnica de plato incidido tubularizaciónuretroplastia (TIPU). Los resultados fueron clasificados como: exitoso, estenosis, fístulas y Slough. Se compararon los factores que influyeron en el éxito de la operación.
Se utilizóSPSS 16.0 para la evaluación estadística, mientras que el análisis de regresión logística se utilizó para determinar el éxito. Para mostrar significación estadística, se usóla cifra p <0,05.
ResultadosCiento ocho pacientes fueron sometidos a reparación de hipospadias distal en nuestra clínica. La media de edad fue de 21.44 ± 2.0. 38 pacientes tenían pene distal, 67 pacientes, tenían hipospadiassubcoronal, 2 pacientes,coronal y 1 paciente,glanular. Ochenta y ocho pacientes lo tenían primario, 5 secundario y 3,terciario. Setenta y ocho pacientes fueron sometidos a TIPU bajo anestesia local y a 30 pacientes se les realizó bajo anestesia epidural. Se utilizóun catéter suprapúbico en 92 pacientes y una sonda transuretral, en 16 pacientes. Dieciséis cirujanos diferentes se encargaron de llevar a cabo las operaciones; setenta de las cuales tuvieron éxito y hubo, además,tres casos de estenosis, 24 fístulas y 11 Slough. En general la tasa de éxito fue del 64.81%. La edad del paciente, la localización del meato uretral externo, el tipo de anestesia, el tipo de desvío, el diámetro del Nelatony el hecho de haber sido realizados por diferentes cirujanos no afectaron a los resultados quirúrgicos. Solo el estado de hipospadias (primari/reconstrucción) afectó al éxito (p=0.037).
ConclusiónEl único factor que influye en los resultados quirúrgicos de reparación de hipospadias distal en adultos parece ser el estado de los propios hipospadias. Podría ser debido a la falta de aplicación de la segunda capa en las operaciones reconstructoras.
Hypospadias is a frequent malformation affecting 18.61 per 10,000 live births in Europe.1 Hypospadias surgery is recommended between 6 and 12 months by The American Academy of Pediatrics. Although a large number of surgical techniques are described, the most popular one is TIP urethroplasty described in 1994 by Snodgrass.2 In developed countries, early diagnosis can be made due to the birth in hospitals, and surgery can be performed in pediatric ages. However, in developing countries, patient's has to reach the doctors and thus the diagnosis can be late. Accordingly, hypospadias surgery is carried out in adulthood. Success rates have been found to be lower in adulthood.3–5 Nocturnal erections and infections are often its causes.
Second layer is important to prevent fistulas.6 Also double-layer flaps are more successful than one-layer or flapless procedures.7–9 More complications may be seen in re-operative cases due to the difficulty of harvesting dartos flap. Poor ventral skin and insufficient flaps may cause fistulas.
In the present study, we aimed to evaluate the results of our patients with distal hypospadias repair surgery in adults and the factors affecting these results.
Material and methodsMedical records of adult patients who underwent distal hypospadias repair in our clinic between December 2001 and January 2016 were reviewed. Study population includes 15- to 30-year adult patients who underwent distal hypospadias repair. Patient's age, external urethral meatus location, hypospadias status (primary/redo), anesthesia type (local/spinal), diversion type (suprapubic/transurethral catheter), catheter diameter and the surgeons performed the operation were recorded as factors affecting the operation success. Patients with chordee and who underwent urethroplasty surgery are excluded from the study. Only patients, operated with tubularisation incised plate uretroplasty (TIPU) technique, were included. Results were classified as successful, stricture, fistula and slough. We compared the factors affecting the success.
Statistical analyses were performed using the SPSS software version 16.0. The univariate analyses to identify variables associated with patient outcome were investigated using Chi-square test. For the multivariate analyses, the possible factors identified with univariate analyses were further entered into the logistic regression analysis to determine independent predictors of patient outcome. A 5% type-I error level was used to infer statistical significance.
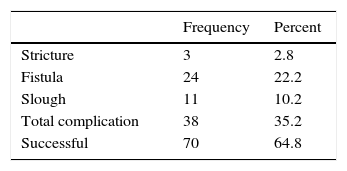
ResultsOne hundred and eight patients underwent distal hypospadias repair in our clinic between December 2001 and January 2016. Mean age was 21.44±2.0 (ranged from 15 to 30 year). Thirty eight patients had distal penile, 67 patients had subcoronal, 2 patients had coronal and 1 patient had glanuler hypospadias. Eighty eight patients had primary, 12 secondary, 5 tertiary and 3 cripple hypospadias. Seventy eight patients underwent TIPU under local anesthesia, 30 patients underwent under spinal anesthesia. Suprapubic catheter used in 92 patients and transurethral catheter used in 16 patients. Sixteen different surgeons performed the operations. Mean follow up time was three months. Seventy operations were successful. Three stricture (2.8%), 24 fistula (22.2%) and 11 slough (10.2%) were determined. Overall success rate was 64.81%.
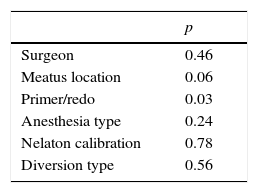
When we compared the factors affecting by Chi-square test meatus location, anesthesia type, diversion type, catheter diameter, surgeon did not affected the success rates, respectively (p=0.34, 0.11, 0.83, 0.71, 0.39). Only affecting factor was hypospadias status (primary/redo) (p=0.05).
When we compared the factors by logistic regression analysis, hypospadias status was the only factor affecting the surgery outcomes (p=0.03).
DiscussionDistal hypospadias surgery is one of the most challenging topics in urology practice. It is also more challenging in adults because of the nocturnal erections and infections.3–5 Fistula is the commonest complication, of which incidence varies from 0% to 27.8%.10 Neo-urethra is covered with flaps to avoid fistula.11 This coverage may be one or double layer. Double layer technique is more successful than single layer or flapless ones.7–9 Redo operations also causes more complications, especially fistula.11 Surgical experience is also important for surgical success.
In our study, overall success rate was 64.81%. Fistula was the most commonly seen complication (22.2%). It was coherent with literature.10 Overall complication rate was 35.19%. This was lower than most of the studies.3,12,13 Generally distal hypospadias surgery was more successful than proximal ones.14 However, hypospadias type did not affected our results. We only assessed our distal hypospadias results. It might be due to this. Anesthesia type did not differ our results. It showed that this surgery can be done under local anesthesia if needed. Soydan et al. also declared that statement before.15 Mostly suprapubic catheter was used for diversion. Diversion type did not significantly differ from each other. However suprapubic catheter is a good way of keeping the wound dry.
Surgical experience was thought to be important for surgical outcomes. It was also shown before.14 Sixteen different surgeons performed our operations. All the surgeons learned the same technique in the same clinic. Surgical outcomes of the surgeons were similar in our study.
The only affecting factor was hypospadias status (primary/redo) (p=0.03). It is hard to find second layer to cover the neo-urethra in redo operations. Penile skin quality is also low. Fahmy et al. reported that fistula rates higher in reoperations.11 Increasing the success of the surgery external spermatic fascia flaps, tunica vaginalis flaps and buccal mucosal grafts can be used for the second layer.16,17
The main limitation is the retrospective manner of the study. Large number of surgeons might affect our results for assessing surgeon experience. Also other limitation is our follow-up time. We might have missed some strictures. However, number of patients increases the power of study (Tables 1 and 2).
The only affecting factor to the surgery outcomes was the hypospadias status (primary/redo). It is due to difficulty of harvesting second layer for covering neo-urethra. In redo surgeries other flap or grafts can be used.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestAuthors declare no conflict of interest.