Different aspects of semen study improved the knowledge of male reproductive system. Aim of the present study is to find out the effect of daily ejaculation for 10 days on semen quality and the level of calcium and magnesium in semen.
Materials and methodsTwenty-one young healthy sexually active men participated in this study. Their consent was collected prior to it. Effect of daily ejaculation for 10 days on semen parameters and calcium and magnesium it were studied. After an abstinence of 3–5 days 11th sample was collected. On a daily basis samples were evaluated and calcium and magnesium were estimated in spermatozoa as well as seminal plasma.
ResultsThe study showed quality of semen improved by daily ejaculation. Statistically no differences in the level of calcium and magnesium in seminal plasma and spermatozoa were observed.
ConclusionThe study proved daily ejaculation was useful in improving its quality.
Los diferentes aspectos del estudio del semen han mejorado el conocimiento del aparato reproductor masculino. El objetivo del presente estudio es descubrir el efecto de la eyaculación diaria durante 10 días sobre la calidad seminal y el nivel de calcio y magnesio en semen.
Materiales y métodosEn el estudio participaron 21 varones sanos y sexualmente activos. Se obtuvo su consentimiento previo al estudio. Se analizó el efecto de la eyaculación diaria durante 10 días sobre los parámetros seminales y el nivel de calcio y magnesio. Tras una abstinencia de 3–5 días, se recogieron 11 muestras. Se evaluaron las muestras sobre una base diaria, calculándose el nivel de calcio y magnesio en los espermatozoides, así como en el plasma seminal.
ResultadosEl estudio mostró que la calidad del semen mejoró con la eyaculación diaria. No se observaron diferencias estadísticas en cuanto al nivel de calcio y magnesio en el plasma seminal y en los espermatozoides.
ConclusiónEl estudio demostró que la eyaculación diaria es útil para mejorar la calidad seminal.
Childlessness is a serious medical and social problem. The cause of male infertility was considered as less knowledge on male reproduction and lack of proper treatment to patient.1 Weyer2 supported this fact, by stating knowledge on male system was thirty years behind that of female. Today male infertility is alarmingly increasing due to different factors such as environmental,3–5 cigarette smoking,6,7 alcoholism6 and others leading to low quality of semen. A major concern of clinicians treating male infertile patient was for improving semen quality. Daily ejaculation was proposed as a measure for this.8,9 Oligozoospermic and oligoasthenozoospermic patients with regular sexual contact achieved fatherhood.8 Similarly daily sexual activities reduced sperm DNA damage and improved semen quality.10 Different elements were shown to play their role in functioning of spermatozoa.11–16 Calcium and magnesium were placed in this list.17–20 Current study is aimed to find out the effect of daily ejaculation for 10 days on semen quality and the level of calcium and magnesium in semen.
Materials and methodsAll glasswares and plasticwares used in this study were kept overnight in 6N nitric acid and washed with tap water, glass distilled, double distilled and triple distilled water. Glasswares except volumetric, were dried in hot air oven above 200°C. Volumetric glasswares and plasticwares were dried by placing them on clean blotting paper. All were stored at dust free area.
Semen samples were collected from 21 healthy and sexually normal subjects belonging to the age group of 20–35 years. All of them gave their consent for the study. They submitted semen samples daily at 8am (±0.5h) for 10 days. They were instructed to maintain an abstinence of 3–5 days21 prior to 1st and 11th sample collection. Mode of collection was masturbation and sample was collected to clean wide mouthed sterile bottles supplied from laboratory.
After collection each semen sample was evaluated for liquefaction time, total volume, pH, viscosity, total spermatozoa count, percentage as well as different grades of sperm motility and morphology of spermatozoa.22 The seminal plasma was separated from spermatozoa by centrifugation (2000×g×10min) and were kept under −20°C till the estimation of calcium and magnesium was carried out. Calcium and magnesium were estimated by Clark and Collip23 and Titan yellow24 method respectively. The principle of the biochemical reaction in Clark and Collip method is, calcium from the sample is precipitated as oxalate by using ammonium oxalate and after washing with ammonia solution, the precipitate is dissolved in acid and titrated with permanganate solution. The principle of method for magnesium estimation is, titan yellow gives red colour with magnesium by using gum ghatti as the colour stabilizer. Magnesium level is measured colorimetrically.
Student's t test was done in semen parameters among first to last day. Correlation coefficient (r value) was performed between two parameters of each day.
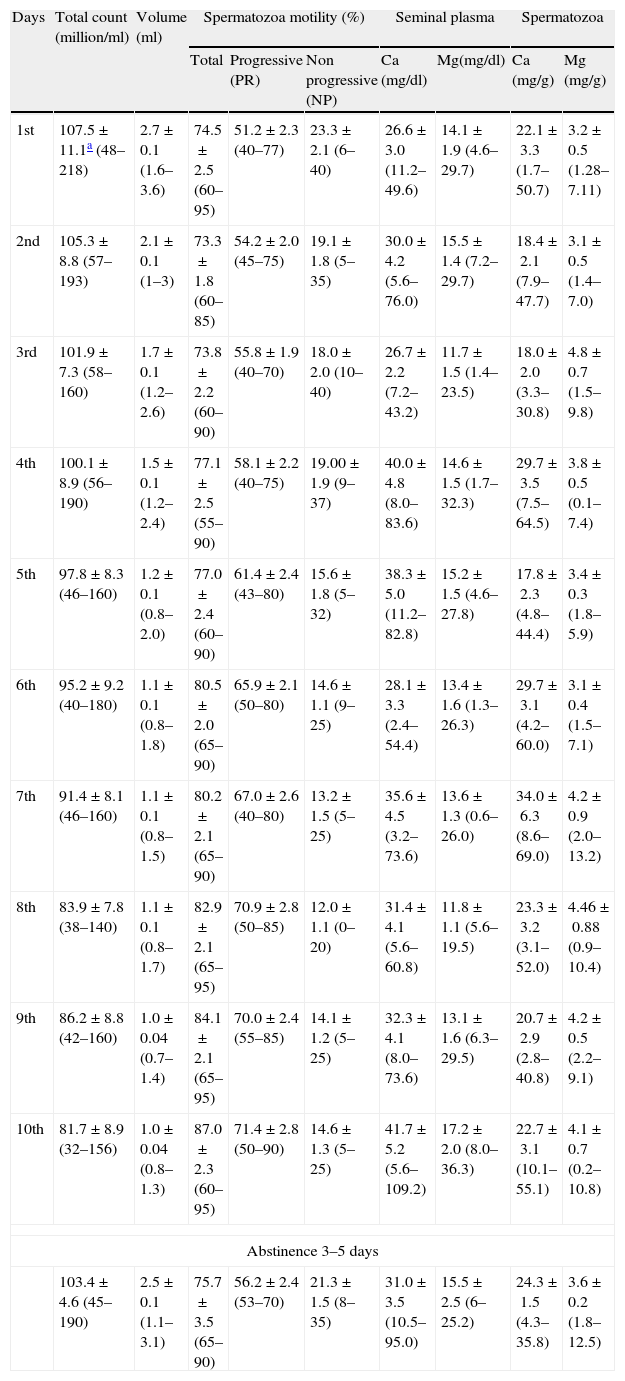
ResultsThe results of this study are shown in Table 1. Semen volume decreased significantly from 1st to 10th day. Liquefaction time and viscosity were within normal range. pH varied but not significantly. Morphology of spermatozoa did not show any change. There was a decrease in total spermatozoa count and an increase in the total percentage of motility. Semen parameters of first day were compared to those of 10th day. All parameters showed highly significant (p<0.001) difference except in case of NP motility (p<0.01). Though calcium showed significant change the level of magnesium remained at same level.
Results of the daily ejaculation study.
| Days | Total count (million/ml) | Volume (ml) | Spermatozoa motility (%) | Seminal plasma | Spermatozoa | ||||
| Total | Progressive (PR) | Non progressive (NP) | Ca (mg/dl) | Mg(mg/dl) | Ca (mg/g) | Mg (mg/g) | |||
| 1st | 107.5±11.1a (48–218) | 2.7±0.1 (1.6–3.6) | 74.5±2.5 (60–95) | 51.2±2.3 (40–77) | 23.3±2.1 (6–40) | 26.6±3.0 (11.2–49.6) | 14.1±1.9 (4.6–29.7) | 22.1±3.3 (1.7–50.7) | 3.2±0.5 (1.28–7.11) |
| 2nd | 105.3±8.8 (57–193) | 2.1±0.1 (1–3) | 73.3±1.8 (60–85) | 54.2±2.0 (45–75) | 19.1±1.8 (5–35) | 30.0±4.2 (5.6–76.0) | 15.5±1.4 (7.2–29.7) | 18.4±2.1 (7.9–47.7) | 3.1±0.5 (1.4–7.0) |
| 3rd | 101.9±7.3 (58–160) | 1.7±0.1 (1.2–2.6) | 73.8±2.2 (60–90) | 55.8±1.9 (40–70) | 18.0±2.0 (10–40) | 26.7±2.2 (7.2–43.2) | 11.7±1.5 (1.4–23.5) | 18.0±2.0 (3.3–30.8) | 4.8±0.7 (1.5–9.8) |
| 4th | 100.1±8.9 (56–190) | 1.5±0.1 (1.2–2.4) | 77.1±2.5 (55–90) | 58.1±2.2 (40–75) | 19.00±1.9 (9–37) | 40.0±4.8 (8.0–83.6) | 14.6±1.5 (1.7–32.3) | 29.7±3.5 (7.5–64.5) | 3.8±0.5 (0.1–7.4) |
| 5th | 97.8±8.3 (46–160) | 1.2±0.1 (0.8–2.0) | 77.0±2.4 (60–90) | 61.4±2.4 (43–80) | 15.6±1.8 (5–32) | 38.3±5.0 (11.2–82.8) | 15.2±1.5 (4.6–27.8) | 17.8±2.3 (4.8–44.4) | 3.4±0.3 (1.8–5.9) |
| 6th | 95.2±9.2 (40–180) | 1.1±0.1 (0.8–1.8) | 80.5±2.0 (65–90) | 65.9±2.1 (50–80) | 14.6±1.1 (9–25) | 28.1±3.3 (2.4–54.4) | 13.4±1.6 (1.3–26.3) | 29.7±3.1 (4.2–60.0) | 3.1±0.4 (1.5–7.1) |
| 7th | 91.4±8.1 (46–160) | 1.1±0.1 (0.8–1.5) | 80.2±2.1 (65–90) | 67.0±2.6 (40–80) | 13.2±1.5 (5–25) | 35.6±4.5 (3.2–73.6) | 13.6±1.3 (0.6–26.0) | 34.0±6.3 (8.6–69.0) | 4.2±0.9 (2.0–13.2) |
| 8th | 83.9±7.8 (38–140) | 1.1±0.1 (0.8–1.7) | 82.9±2.1 (65–95) | 70.9±2.8 (50–85) | 12.0±1.1 (0–20) | 31.4±4.1 (5.6–60.8) | 11.8±1.1 (5.6–19.5) | 23.3±3.2 (3.1–52.0) | 4.46±0.88 (0.9–10.4) |
| 9th | 86.2±8.8 (42–160) | 1.0±0.04 (0.7–1.4) | 84.1±2.1 (65–95) | 70.0±2.4 (55–85) | 14.1±1.2 (5–25) | 32.3±4.1 (8.0–73.6) | 13.1±1.6 (6.3–29.5) | 20.7±2.9 (2.8–40.8) | 4.2±0.5 (2.2–9.1) |
| 10th | 81.7±8.9 (32–156) | 1.0±0.04 (0.8–1.3) | 87.0±2.3 (60–95) | 71.4±2.8 (50–90) | 14.6±1.3 (5–25) | 41.7±5.2 (5.6–109.2) | 17.2±2.0 (8.0–36.3) | 22.7±3.1 (10.1–55.1) | 4.1±0.7 (0.2–10.8) |
| Abstinence 3–5 days | |||||||||
| 103.4±4.6 (45–190) | 2.5±0.1 (1.1–3.1) | 75.7±3.5 (65–90) | 56.2±2.4 (53–70) | 21.3±1.5 (8–35) | 31.0±3.5 (10.5–95.0) | 15.5±2.5 (6–25.2) | 24.3±1.5 (4.3–35.8) | 3.6±0.2 (1.8–12.5) | |
All parameters of 11th semen sample returned back to similar to that of 1st day. This was reported earlier.21
DiscussionEjaculation performed once in every 24h is termed as daily ejaculation. Many believed repeat ejaculation deplete the gonadal as well as extra gonadal reserve and abstinence permit to accumulate spermatozoa and fluid volume. Considering this aspect some physicians suggested to their oligozoospermic patients to maintain sexual abstinence for several days and perform coitus on the day of ovulation. Similarly clinicians instructed patients to maintain an abstinence of minimum number of days before semen examination. Some clinicians reported daily ejaculates improved semen quality. Van Zyl et al.8 observed in their study 58% of patients with less than 10 million/ml total sperm count could achieve fatherhood after regular sexual contacts. Reasonably Gosalvez et al.25 reported decrease in sperm DNA fragmentation with shorter duration of abstinence. In a 7 day lasting daily ejaculate study improvement in semen quality by reducing sperm DNA damage was seen.10 This was due to shorter exposure of sperm to reactive oxygen in testicular ducts and epididymis. It was proposed frequent ejaculation might promote sperm production by reducing spermatogenesis regulator – inhibin in blood.9,26 Biochemical studies showed different inorganic elements were present in semen.11,14–16,27–29 Calcium and magnesium were considered as important elements in semen for metabolic function. Hong et al.30 and Sorensen et al.31 reported that calcium act as a key regulator of human sperm functions especially in motility and acrosome reaction. Magnesium was required for enzymes promoting ATP production essential for sperm motility. Nikoobakht et al.32 and Omu et al.33 found a decrease in seminal plasma magnesium led to premature ejaculation. Considering all above, the present daily ejaculation study was designed to understand changes in seminal parameters and two elements – calcium and magnesium – in it.
In the current study it was seen that semen volume decreased significantly (p<0.001) from 1st to 10th day as observed earlier.21,34–38 This was due to exhaustion of seminal vesicles which contributed 60% secretion of a normal ejaculate.11,27 In a single emission significant exhaustion of seminal vesicles was taking place and repeated ejaculation increased exhaustion rate faster.27 Heuchel et al.39 noted a statistical correlation between length of abstinence and semen volume. A reverse pattern might be expected to some level in absence of abstinence.
In this study, liquefaction time and viscosity did not show change from 1st to 10th day. pH of semen insignificantly changed. Possible reason was reduced secretion of seminal vesicles. In another study it was observed that pH changed in 3rd and 4th day of daily ejaculation.21 No correlation was found between pH and level of Ca and Mg in semen. No significant change in morphology of spermatozoa was seen in the current study. Tyler et al.37 had similar observation. Zaneveld and Polakoski40 had shown increase in the number of immature form of spermatozoa.40 Authors explained this as interruption in spermatogenesis. Valsa et al.20 similar observation on their four hourly ejaculation study.
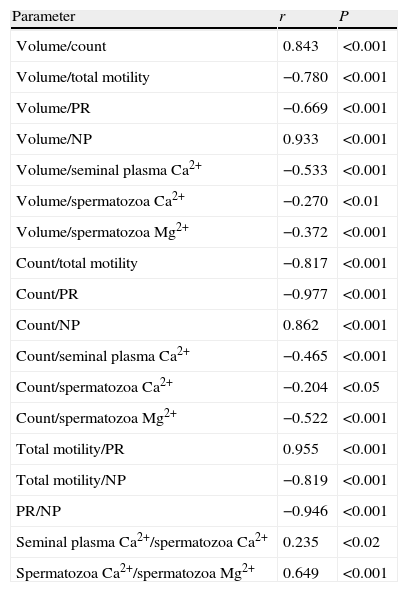
Generally total sperm count and motility pattern are considered as to important parameters in semen study.41 The study showed that a constant level of total spermatozoa count maintained a level up to 3rd day, which differed significantly from fourth day (<0.001). Earlier studies supported this.21,37,38 Though Amann42 noted daily production of semen was constant. Reduction in volume and spermatozoa count was positively correlated (Table 2) which indicated that both were regulated by one source. Opposing results were reported by Tyler et al.37 Though decrease in total sperm count was highly significant it was much above the minimum prescribed by WHO.22
The significant r values between different parameters of semen evaluation and Ca2+ and Mg2+ concentration in all days together (n=210) samples of daily ejaculate study.
| Parameter | r | P |
| Volume/count | 0.843 | <0.001 |
| Volume/total motility | −0.780 | <0.001 |
| Volume/PR | −0.669 | <0.001 |
| Volume/NP | 0.933 | <0.001 |
| Volume/seminal plasma Ca2+ | −0.533 | <0.001 |
| Volume/spermatozoa Ca2+ | −0.270 | <0.01 |
| Volume/spermatozoa Mg2+ | −0.372 | <0.001 |
| Count/total motility | −0.817 | <0.001 |
| Count/PR | −0.977 | <0.001 |
| Count/NP | 0.862 | <0.001 |
| Count/seminal plasma Ca2+ | −0.465 | <0.001 |
| Count/spermatozoa Ca2+ | −0.204 | <0.05 |
| Count/spermatozoa Mg2+ | −0.522 | <0.001 |
| Total motility/PR | 0.955 | <0.001 |
| Total motility/NP | −0.819 | <0.001 |
| PR/NP | −0.946 | <0.001 |
| Seminal plasma Ca2+/spermatozoa Ca2+ | 0.235 | <0.02 |
| Spermatozoa Ca2+/spermatozoa Mg2+ | 0.649 | <0.001 |
Increase in PR from 2nd day and total motility from 4th day was seen (Table 1). It was noted that NP decreased from 2nd day. The increase in motility was at the cost of NP ones. Amelar et al.43 reported same in their 5 day daily ejaculate study. However quality of semen was poor in ejaculates submitted by same patients after 10 days of abstinence. This showed storing male secretion in own system deteriorated semen quality and daily ejaculation improved it. Rui et al.44 and Shah et al.45 reported similar objection to this explanation was present.37,39,46,47 Spermine showed positive correlation with spermatozoa motility.48 Adenyl cyclase – primary regulator of spermatozoa motility was changed in frequent ejaculate.49 de Lamirande and Gangon50 found a depletion in spermatozoa motility inhibitory factor. Similar was also reported by Skandhan et al.21
Spermatozoa motility and total volume were negatively correlated (Table 2). Total percentage of motility and sperm count showed negative correlation from 2nd to 10th day. When values of all samples (n=210) were included negative correlation between total spermatozoa count and motility was seen (Table 2). Whereas in case of normal sample positive correlation was seen.41
Calcium and magnesium was estimated both in spermatozoa and seminal plasma by different group of workers. A total of 116 semen sample were studied by us for establishing normal values for calcium and magnesium. Total semen showed calcium as 38.9mg/dl and magnesium as 17.2mg/dl.51 In this study no significant changes in the level of calcium and magnesium was observed both in seminal plasma and spermatozoa (Table 1). This indicated that prostate gland, which is the source of calcium and magnesium was regularly functioning during daily ejaculation. The prostate product, spermine, was significantly high in repeat ejaculation.44,45 A four hourly ejaculate study showed that level of calcium and magnesium in seminal plasma and magnesium in spermatozoa increased significantly.20 Similarly level of zinc and copper increased significantly.21 Earlier studies were not conducted on the level of calcium and magnesium in daily ejaculate. In a similar study Valsa et al.38 did not any correlation between metal copper in semen and semen parameters.
A negative correlation of volume was seen in seminal plasma and spermatozoa calcium and magnesium (Table 2). This was due to less amount of seminal vesicular fluid and more amount of prostatic fluid with calcium and magnesium.52,53 Spermatozoa count was negatively correlated with seminal plasma and spermatozoa calcium and magnesium (Table 2). This was possibly due to lack of time for spermatogenesis or for storing and maturation of cells at different levels. Presence of immature spermatozoa was seen in sample.
After maintaining an abstinence of 3–5 days, 11th sample showed returning of semen parameters back to normal. Noticeable was spermatozoa motility. Percentage of NP increased at the cause of PR. This supported a hypothesis that motility of spermatozoa depended on its retention time in epididymis; the less the time stay in epididymis the better the motility. Sperm motility inhibitory factors at this level was proposed as the reason.54 The level of calcium and magnesium returned back to the level of 1st day of experiment (Table 1). Supporting reports were available.21 The results of the present study confirmed that an abstinence to 3–5 days each sufficient to bring back the element to the normal level. The abstinence days differed among different workers which was as follows, Eliasson34 3 days; Zaneveld, Polakoski40 4 days; Belsey et al.55 2–7 days; Tyler et al.37,56 3–7 days; Fredricsson57 3–5 days; Skandhan et al.21 3–5 days. Whereas some preferred for collecting semen samples while continuing regular sexual activity.58,59
In conclusion, 10 days daily ejaculate study showed that volume and total sperm count significantly decreased whereas PR and total spermatozoa motility increased. The level of calcium and magnesium in seminal plasma and spermatozoa remained same. After maintaining an abstinence of 3–5 days the seminal parameters returned back to the level of first day. Study proved daily ejaculation improved semen quality by means of maintaining total spermatozoa count in normal range and increasing spermatozoa motility.
Ethical disclosuresRight to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Protection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflict of interestThe authors have no conflict of interests to declare