Pathogens such as Haemophilus spp. have been associated with non-gonococcal urethritis, but their role is unproven. To describe the clinical characteristics and therapeutic outcomes in male patients diagnosed with Haemophilus spp. urethritis.
MethodsWe carried out a retrospective study of all patients who presented to our hospital (in either the emergency department or the outpatient clinic) between July 2016 and April 2018 in whom Haemophilus spp. was isolated in the urethral samples. We enrolled 30 men with Haemophilus spp.-positive urethritis, including coinfections with Neisseria gonorrhoeae and Chlamydia trachomatis. Clinical, laboratory, demographic, and behavioral data were obtained by reviewing medical histories.
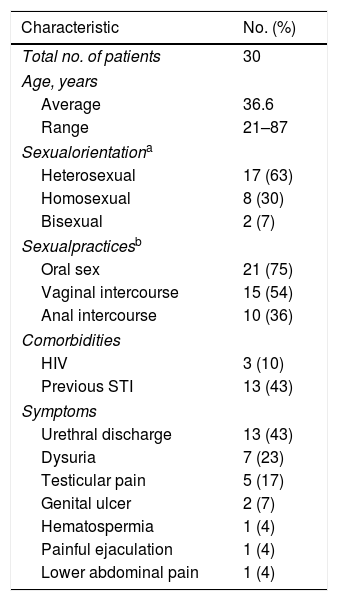
ResultsThe mean age of the patients was 36.6 years (range 21–87). Seventeen patients (63%) reported being exclusively heterosexual. Three patients (10%) were HIV infected, all of them with an undetectable viral load. The most common clinical presentation was mucopurulent urethral discharge, in 13 patients (43%). The antibiotic treatment achieved a complete clinical resolution in 73%.
ConclusionsHaemophilus urethritis affected men regardless of their sexual orientation or HIV status. Unprotected oral sex may play a role in its transmission. The limitations of the study preclude verification of the pathogenic role of Haemophilus spp. in acute urethritis, but clinical response after antibiotic treatment suggests that Haemophilus spp. can play such a role.
Patógenos como Haemophilus spp. se han asociado con uretritis no gonocócica, pero su papel no está probado. El objetivo de nuestro trabajo ha sido describir las características clínicas y los resultados terapéuticos en varones diagnosticados de uretritis de Haemophilus spp.
MétodosRealizamos un estudio retrospectivo de todos los pacientes que se presentaron en nuestro hospital (ya sea en el departamento de emergencias o en la clínica ambulatoria) entre julio del 2016 y abril del 2018 en quienes Haemophilus spp. se aisló en las muestras uretrales. Se incluyó a30 hombres con uretritis positiva para Haemophilus spp., incluidas las coinfecciones con Neisseria gonorrhoeae y Chlamydia trachomatis. Los datos clínicos, de laboratorio, demográficos y de comportamiento se obtuvieron al revisar las historias clínicas.
ResultadosLa edad media de los pacientes fue de 36,6 años (rango 21-87). Diecisiete pacientes (63%) informaron ser exclusivamente heterosexuales. Tres pacientes (10%) estaban infectados por el VIH, todos ellos con una carga viral indetectable. La presentación clínica más común fue secreción uretral mucopurulenta, en 13 pacientes (43%). El tratamiento antibiótico logró una resolución clínica completa en el 73%.
ConclusionesLa uretritis por Haemophilus afectó a los hombres independientemente de su orientación sexual o estado de VIH. El sexo oral sin protección puede desempeñar un papel en su transmisión. Las limitaciones del estudio impiden la verificación del papel patogénico de Haemophilus spp. en uretritis aguda, pero la respuesta clínica después del tratamiento con antibióticos sugiere que Haemophilus spp. puede desempeñar ese papel.
Urethritis, one of the most common sexually transmitted infections (STI) among men, is classified as gonococcal (GU) or non-gonococcal (NGU) depending on the presence or absence of Neisseria gonorrhoeae.1 In 20–50% of cases of NGU the cause is not identified. Chlamydia trachomatis accounts for 30–40% of cases and Mycoplasma genitalium for around 10–30%.2 Other pathogens, such as Haemophilus spp., have been associated with NGU, but their role is unproven.2,3 Both Haemophilus influenzae and Haemophilus parainfluenzae are colonizers of the upper respiratory tract and are part of the normal oral microflora.4,5 They are not only commensal within the pharynx but also pathogens causing various infections, mainly in relation to the respiratory tract.6 Sexual transmission of both has been described. Transmission of oropharyngeal commensal flora to the urethra via insertive oral sex is recognized as a mode of transmission of several pathogens, including Haemophilus spp.5
Materials and methodsStudy populationThis is a retrospective study of all patients who presented to our hospital (in either the emergency department or the outpatient clinic) between July 2016 and April 2018, reporting symptoms of urethritis in whom a Haemophilus sp. was isolated from urethral samples. Symptoms suggestive of urethritis included urethral discomfort, dysuria, and/or mucopurulent or clear discharge. The study was approved by our institutional medical and research ethics committee. Clinical, laboratory, demographic, and behavioral data were obtained by reviewing medical charts.
Laboratory studiesUrethral samples were obtained by convenient swabs for conventional bacteriological and Multiplex PCR studies. Conventional bacteriological study included microscopic examination by Gram stain of the sample and culture. Petri dishes of chocolate agar (BD), Martin-Lewis agar (BD), Gardnerella agar (BD), and Sabouraud agar with gentamicin and chloramphenicol (BC) were used. Chocolate agar, Martin-Lewis agar, and Gardnerella agar were incubated at 35–37°C with enriched 7% CO2 atmosphere for 3 days (chocolate and Martin-Lewis agar) or 2 days (Gardnerella agar). Sabouraud agar was incubated at 35–37°C for 2 days in room air. Neisseria and Haemophilus strains were identified by API NH test (bioMérieux). Multiplex PCR was performed by AnyplexTM II STI-7 assay (Seegene), which detects five major pathogens in a single reaction: Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Mycoplasma genitalium, and Ureaplasma urealyticum.
Statistical analysisStatistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented for continuous measurements. Frequencies and percentages are reported for dichotomous and ordinal variables.
ResultsOver the study period a total of 204 patients were diagnosed with acute urethritis, and Haemophilus spp. were isolated in 30 urethral samples received in our laboratory (Table 1). The mean age of the patients was 36.6 years (range 21–87). Seventeen patients (63%) reported being exclusively heterosexual, eight (30%) were men who have sex with men (MSM), and two (7%) reported having sexual intercourse with both men and woman; data on sexual activity were not available for three patients. The mean number of sexual partners in the last 60 days before the hospital visit was 3.5 (range 1–20). Patients were asked about their sexual exposures during the 2 months before consultation. With the exception of three patients, all reported having practiced unprotected insertive sex, most commonly oral sex. Three patients (10%) were HIV infected, all of them with undetectable viral load. Thirteen patients (43%) reported a previous STI.
Causes of urethritis diagnosed between July 2016 and April 2018.
| Neisseria gonorrhoeae | 73 |
| Chlamydia trachomatis | 69 |
| Haemophilus parainfluenzae | 19 |
| Haemophilus influenzae | 10 |
| Haemophilus sp. | 1 |
| Ureaplasma urealyticum | 17 |
| Mycoplasma genitalium | 13 |
| Trichomonas vaginalis | 1 |
| Neisseria meningitidis | 1 |
| Total | 204 |
The most common clinical presentations were mucopurulent urethral discharge (13patients, 43%), dysuria (seven patients, 23%), and testicular pain (five patients, 17%). Complete demographic data are listed in Table 2. Ten cases (33%) corresponded to Haemophilus influenzae, 19 (63%) to Haemophilus parainfluenzae, and one (3.3%) could not be identified at the species level. In five of the 30 cases (17%), Haemophilus was isolated with another pathogen: in four cases with C. trachomatis (80%) and in one with N. gonorrhoeae.
Patient demographics.
| Characteristic | No. (%) |
|---|---|
| Total no. of patients | 30 |
| Age, years | |
| Average | 36.6 |
| Range | 21–87 |
| Sexualorientationa | |
| Heterosexual | 17 (63) |
| Homosexual | 8 (30) |
| Bisexual | 2 (7) |
| Sexualpracticesb | |
| Oral sex | 21 (75) |
| Vaginal intercourse | 15 (54) |
| Anal intercourse | 10 (36) |
| Comorbidities | |
| HIV | 3 (10) |
| Previous STI | 13 (43) |
| Symptoms | |
| Urethral discharge | 13 (43) |
| Dysuria | 7 (23) |
| Testicular pain | 5 (17) |
| Genital ulcer | 2 (7) |
| Hematospermia | 1 (4) |
| Painful ejaculation | 1 (4) |
| Lower abdominal pain | 1 (4) |
HIV, human immunodeficiency virus.
STI, sexual transmitted infection.
In the present study, we retrieved clinical data from the medical records of men with Haemophilus spp. Culture-positive urethritis who were treated in our institution. In our series, H. parainfluenzae was more frequent than H. influenzae (63% vs 33%), which is in concordance with the literature.5,7,8 Interestingly, Haemophilus parainfluenzae was the third most common pathogen in urethral samples in the overall total of 204 patients with symptoms of acute urethritis, being isolated in 19 patients (9.3%) as compared with Neisseria gonorrhoeae in 73 cases (35.7%) and Chlamydia trachomatis in 69 (33.8%). In other studies, the third most frequent cause of urethritis has been Mycoplasma genitalium (Ito 2016, Rane 2014). The most common clinical symptoms were urethral discharge, which was present in 13 patients (43%), followed by dysuria in 7 (23%) and testicular pain in 5 (17%). Urethritis caused by Haemophilus spp. has indistinctive clinical symptoms compared with other causes of urethritis, which can cause difficulties in differentiating them.5 Patients were asked about their sexual behavior (orientation and practice) during the 2 months before consultation. The mean number of sexual partners was 3.5 (range 1–20). To our knowledge, this is the only study to report these data. The majority were heterosexual (17, 63%) and practiced unprotected oral sex. This finding is discrepant in comparison with previously published studies, which show a higher prevalence of Haemophilus urethritis in MSM. Rane et al.9 suggested that MSM may be acquiring established and unidentified urethral pathogens more commonly than would be anticipated via low-risk sexual practices, perhaps reflecting the widespread practice of unprotected orogenital sex in MSM9. Ito et al.10 reported that all men with Haemophilus influenzae-NGU in their series practiced unprotected oral sex.10 Another study5 reported that all men in their series had practiced unprotected insertive oral sex, and five of them denied having had another sexual contact apart from this exposure.5 Other studies have also reported that urethritis caused by Haemophilus spp. is characterized by transmission of the pathogens through oral sex.5,10 Those data support the contribution of oropharyngeal exposure to this syndrome and require examination in case-control studies using molecular methods. Diagnostic and management approaches to acute NGU do not differentiate between men who have sex with men (MSM) and men who have sex with women (MSW).9 Because the patients were treated at different institutional levels, the following treatments were proposed: azithromycin, azithromycin plus ceftriaxone, azithromycin plus ciprofloxacin, ciprofloxacin, doxycycline, or doxycycline plus ceftriaxone. In 22 patients (73%) the empirical treatment achieved a complete clinical resolution. In the eight patients in whom symptoms persisted, the main complaint was urethral discharge. All of them had positive results for culture of a second urethral exudate after the first treatment, in seven (88%) for H. parainfluenzae and in one (13%) for H. paraphrophilus. The treatment was then guided by the antibiogram. Two patients, both HIV positive, remained symptomatic, presenting persistence of urethral exudate and positive cultures for H. parainfluenzae. Oral Haemophilus colonization in different amounts is very frequent.11 Patients with treatment failure may benefit from a search strategy for Haemophilus colonization in their sexual partner(s) and possible prophylactic measures, such as antimicrobial single dose use after oral insertive sexual practices.
Several limitations of this study have to be pointed out. The lack of a representative control group precludes proof of the pathogenic role of Haemophilus spp. in urethritis. As this is a retrospective study involving retrieval of clinical information from clinical records, some items of information were lacking in some patients. Finally, the small sample size does not allow accurate conclusions to be drawn regarding therapeutic outcomes.
The predominance of heterosexual men in our series may be related to the frequency of oral sexual practice in our own population and could also be due to MSM having access to regular screening and treatment in specific community settings. The data presented in our study, as well as in the specific literature, support the contribution of oropharyngeal exposure to this syndrome and warrant further investigations in case–control studies using molecular methods. In men with treatment failure it may be useful to study the partner's oral flora and, hence, to establish a direct relation with oral sex and identify possible antimicrobial prophylaxis measures.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestNo funding or conflict of interest for this paper; no need of informed consent.