ED and PE are the most common male sexual dysfunctions, although they remain underdiagnosed and undertreated.
AimTo ascertain how a group of Spanish urologists currently address ED and PE.
MethodsDescriptive study based on a self-designed questionnaire about the clinical practice in ED and PE upon diagnosis, treatment and monitoring, patient–physician relationship and the role of the patient's partner.
ResultsThe survey was completed by 188 experienced urologists. Most patients went to the urologist's office without a previous diagnosis (92% of the urologists found <10 PE-diagnosed patients in public settings). The diagnosis of ED and/or PE was mainly carried out by the current urologist and not by another professional, particularly in private centres as opposed to public centres (78.8% vs 57.0% for ED; 82.0% vs 62.6% for PE). Most urologists believed that these disorders are underdiagnosed and deemed them as general health issues. 38% of urologists acknowledged using validated questionnaires to diagnose ED. PE was considered a subjective problem rather than a true disease and the use of PRO-based diagnosis of PE was not generally accepted (14%). Treatment options of both disorders were chosen as expected. Referral to the andrologist is usually scheduled in moderate-to-severe PE or severe ED. The cohort seemed to be mostly neutral (50%–75% for ED and 40%–55% for PE) regarding patient reluctancy to talk about their sexual problem. Patients’ partners play an important role in helping men seeking treatment.
ConclusionUrologists should show more proactivity during anamnesis and routine visits to improve management of ED and PD.
A pesar de que, la DE y la EP son las disfunciones sexuales masculinas más frecuentes, siguen estando infradiagnosticadas e infratratadas.
ObjetivoConocer cómo es el abordaje actual de la DE y la EP, a partir de un grupo de urólogos españoles.
MétodoEstudio descriptivo, mediante un cuestionario predefinido, con relación a la práctica clínica de la DE y la EP, incluyendo su diagnóstico, su tratamiento y su seguimiento, la relación médico-paciente y el papel de la pareja.
ResultadosCiento ochenta y ocho urólogos expertos dieron respuesta al cuestionario predefinido. La mayoría de los pacientes acudieron a la consulta del urólogo sin un diagnóstico previo (el 92% de los urólogos hallaron <10 pacientes diagnosticados de PE en el ámbito público). El diagnóstico de la DE y/o la EP fue realizado mayoritariamente por el urólogo, y no por otro profesional, especialmente en el ámbito privado frente al público (78,8 frente al 57,0% para la DE; 82,0 frente al 62,6% para la EP). La gran mayoría de los urólogos señalaron que ambas disfunciones estaban siendo infradiagnosticadas y, por tanto, las consideraron como un problema de salud general. El 38% de los urólogos indicó utilizar cuestionarios validados para el diagnóstico de la DE. La EP se percibió como un problema subjetivo más que como una verdadera enfermedad, y el uso de PRO en el diagnóstico de la EP no fue generalmente aceptado (14%). La elección de las opciones de tratamiento de ambas disfunciones aconteció según lo esperado. Se consideró la derivación a andrología en los casos de la EP moderada-grave o en los casos de la DE grave. En cuanto a la reticencia de los pacientes a hablar de su problema sexual, la respuesta fue mayoritariamente neutra (50-75% para la DE y 40-55% para la EP). Las parejas de los pacientes desempeñan un papel importante en el momento que estos buscan opciones de tratamiento.
ConclusiónLos urólogos deben mostrar mayor proactividad, durante la anamnesis y las visitas de rutina, para mejorar el manejo de la DE y la EP.
Erectile dysfunction (ED) and premature ejaculation (PE) are reportedly the most common sexual problems in men and have a serious impact on global health and quality of life.1,2 ED is the inability to achieve and sustain an erection sufficient to permit satisfactory sexual performance.3 PE is defined as a male sexual dysfunction characterized by the inability to delay ejaculation on all or nearly all vaginal penetrations, with an intra-ejaculatory latency time (IELT) ≤1min of vaginal penetration (lifelong type) or ≤3min (acquired type).4
ED was reported to be the single greatest risk factor for acquired PE but not for lifelong PE.5,6 However, it was found that about one third of ED patients complained of PE on careful investigation.7 It is therefore important to acknowledge that there is a bidirectional relationship between both disorders, so that PE could be secondary to ED.8 It has been suggested that the lack of sexual satisfaction due to PE, could be a psychological reflection of ED, either because of the need for a more intense stimulation capable of sustaining and maintaining erection or the anxiety showed during the sexual intercourse.9 Accordingly, the Global Study of Sexual Attitudes and Behaviours (GSSAB), an international survey of different aspects of sex and relationships among adults aged 40–80 years from 29 countries all over the world, showed a significant correlation between ED and PE in any region studied.10 More recently, the results of a cross-sectional on-line survey confirmed a high prevalence of coexistence of PE and ED, indicating a complicated relationship between both conditions and the importance of their screening in practice.11
Primary care physicians (PCP) are often reluctant to initiate discussions about sexual concerns with their patients.12 This may explain why ED and PE are underdiagnosed and consequently undertreated in the primary health care setting before referral, and the scarcity of epidemiological data. The EDEM Study (Epidemiology of Masculine Erectile Dysfunction, 1998–1999) outlined the importance of this problem, so that the prevalence of ED is 12.1% (1.5–2.0 million Spanish men suffer from ED), although only 16.5% had visited a doctor.13 In this sense, the ATLAS Project on ED, conducted among 544 PCP demonstrated that only 5% of Spanish males reporting erection problems are diagnosed with ED, from those only half receive a treatment.14 The Spanish Association of Andrology, Sexual and Reproductive Medicine (ASESA) conducted the first Demographic Study on Premature Ejaculation (DEEP, unpublished). DEEP showed that 43% of Spaniards (n=1000; aged 18–59 years) suffer from PE at some point in their life, although only 38% of PE men considered that they should visit a doctor.
High prevalence data of ED and PE in Spain, together with the need to lower the rate of underdiagnosis and undertreatment due to the inaccurate clinical management of these patients, encouraged ASESA to start the PANDORA Project (Overview of Erectile Dysfunction and Premature Ejaculation) Approach Recommendations [Panorama de la Disfunción Eréctil y la Eyaculación Precoz. Recomendaciones para su Abordaje]). PANDORA was intended as a wide-ranging research project to enclose the opinions, attitudes and perceptions about ED and PE from 3 different groups: urologists, patients and the general healthy male population. The first data coming from PANDORA showed that while the level of knowledge of ED and PE is more than acceptable among the general male population, almost 70% of the sample have never or hardly ever worried about these sexual issues and 60% have never seen a urologist.15 This publication also highlighted a considerable percentage of ED and PE patients who had been underdiagnosed, firstly because not many individuals raise such problems with their doctors, and more importantly because physicians do not make the right questions to assess sexual dysfunctions.
Our group hypothesized that this problem still exists in Spain. Therefore, we aimed to investigate the knowledge, clinical practice patterns and attitudes of urologists when dealing with ED and PE.
Material and methodsStudy setting and designIn 2018, and on strength of the PANDORA project, ASESA launched a survey study that was mailed to a representative and statistically powered sample of randomly selected Spanish urologists (n=188). From the whole sample, 134 participants work in public health care centres, compared to 13 who were employed only in private hospitals, and 41 who worked in public and private settings, and all of them were included in the present study. A self-administered and quantitative online questionnaire was pointedly created and validated by the National and Regional Committee of the PANDORA Project, formed a group (n=17) of renowned and highly-experienced Spanish andrologists.
Data collectionThe questionnaire was developed to ascertain how urologists currently address ED and PE. It was also intended to describe the profile of the participating specialists who see patients with ED and/or PE, as well as possible differences in the management of both disorders due to the type of hospital centre – public or private – and the Autonomous Community of residence. The questionnaire also included questions about the general profile of the participating urologists: age, professional position, workplace (Autonomous Community, rural or urban and private or academic/public settings), years practicing sexual medicine and percentage of time spent dealing with sexual medicine in academic or private settings; their professional practice in male sexual health (the number of patients with or without a diagnosis of ED and/or PE); their opinion about the importance of ED and/or PE in male health (the extent of agreement on the underdiagnosis and undertreatment of both conditions); how they manage ED and/or PE in actual clinical practice (clinical history, diagnosis and treatment); ED- and PE-patient flow and monitoring of comorbidities; their perception of the communication between patient and physician (degree of difficulty in talking to patients about a sexual problem); and the role of partners in the course of ED and PE.
Statistical analysisQuantitative variables are presented as mean, average and standard deviation. Qualitative variables are expressed through absolute frequencies and percentages (n, %). The chi-square (χ2) statistical test was used to check independence between two qualitative variables. The significance level (p-value) was 0.05 bilateral. Some questions were quantitively answered with percentages (continuous variables), whereas some other statements required either a dichotomous answer (yes or no/private or public) or multiple-choice options. For the evaluation of some of the responses (definition, diagnosis and treatment of ED and PE; the patient–physician relationship and the role of partners as seen by the participants), a 7-point ordinal Likert-type scoring scale was used to assess the level of (dis)agreement (1=totally disagree/would never recommend it; 7=totally agree/always recommend it).
ResultsThe respondents consisted of 73.4% men with a mean age of 43 years (range 25–65 years), 35.1% have accounted on >10 year-experience in male sexual medicine (mean experience of 10.2 years); mostly working as assistant urologists (78.7%) and 50% worked in larger hospitals (>500 beds), in an urban setting (98.9%).
Half of patients seen by urologists in public centres were >65 years, while younger patients (<40 years) preferred private institutions (14.6% in public vs 21.6%, respectively; p=0.000) (data not shown). The number of patients already diagnosed with ED or PE before their first visit to the specialist was also investigated. Around 60% of physicians had seen an average of 10–20 patients who had been diagnosed with ED in the previous month in their public practice. In contrast, less than 5 PE patients who asked for medical help to the urologists working at public institutions (92%) were to the office with a previous diagnosis. Actually, nearly 80% of urologists recognized to diagnose these disorders in private office.
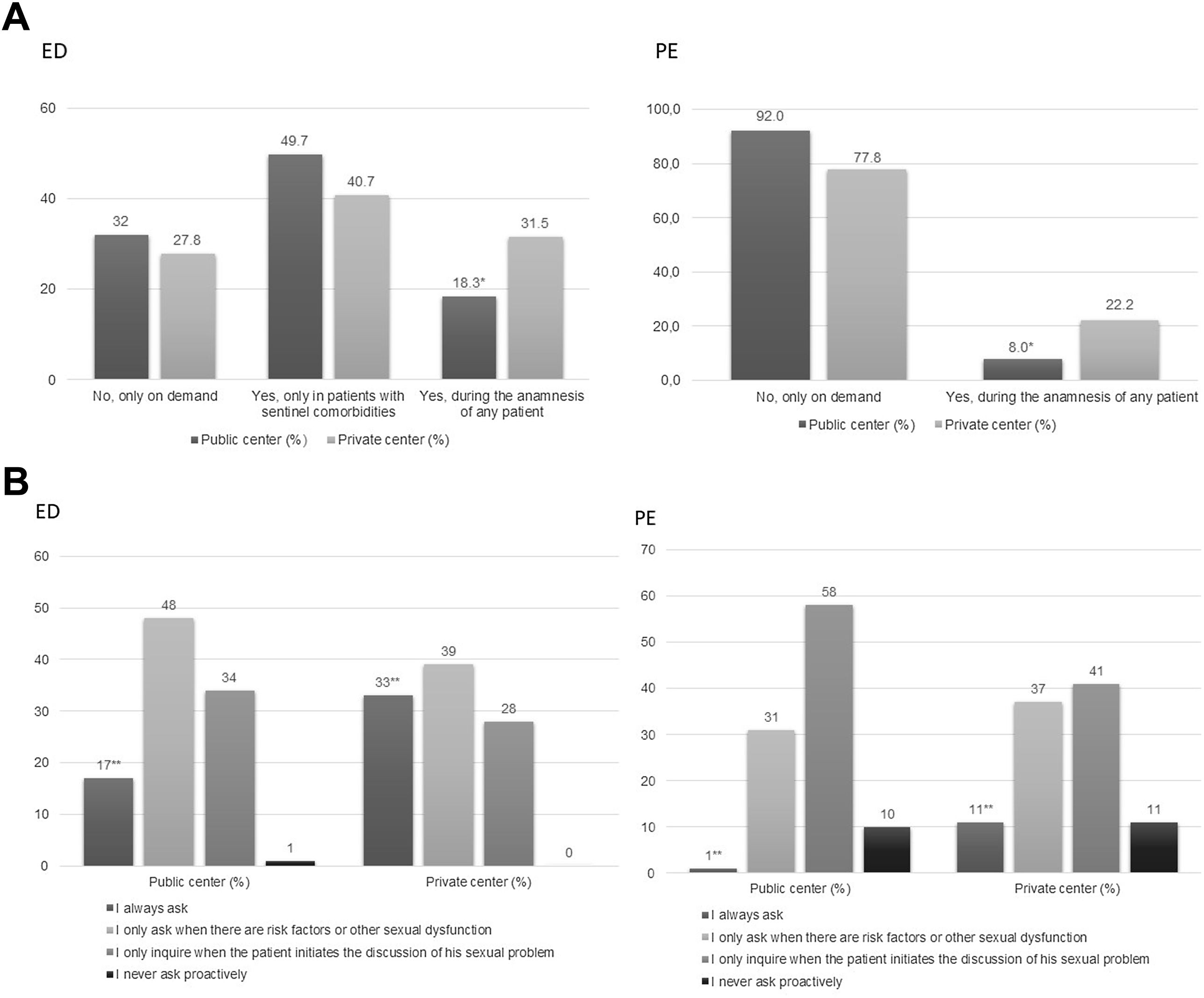
The procedure followed by urologists to do the anamnesis of ED and PE in clinical practice was also investigated (Fig. 1). The medical community showed a very little proactivity to question patients about ED or PE during the anamnesis regardless the hospital setting (Fig. 1a). Over 30% of participants admitted that they did not ask about ED unless that was the reason for the visit or was brought up by the patient (32%, public vs 27.8%, private) or unless ED could be a sentinel marker of other major comorbidities (such as diabetes, benign prostatic hyperplasia or cardiovascular disease). In the case of PE, the scenario was even worse; in public settings, up to 92% of respondents only reacted to cases in which the patient had asked for their sexual problem. In contrast, the number of clinicians who usually included questions about PE problems in the anamnesis was significantly higher in private medicine compared to the public setting (22.2% vs 8%, respectively; p=0.000). Common clinical practice patterns and the attitudes of the participants to approaching ED and/or PE were also investigated (Fig. 1b), with significant differences observed in the private setting. Of the entire cohort of participants employed in private hospitals, 33% and 11% stated that they always probe for ED symptoms (17% in public settings; p=0.003) and PE (1% in public settings; p=0.000), respectively. Moreover, similarly to the anamnesis, most participants confirmed that the symptoms of these male sexual disorders are assessed whenever they occur simultaneously with other health risk factors in their daily clinical practice (Fig. 1b).
Participant urologists (n=188) responded about how often they ask to the patient during the anamnesis (a) and in current clinical practice (b) of ED and PE. When indicated, data are shown as a percentage (%). *Statistical differences among the surveyed population were observed when answers related to anamnesis (a) were grouped (% urologists in public was less than % urologists in private healthcare centres; p=0.001 for ED; p=0.000 for PE). **Statistical differences among the surveyed population were observed when answers related to common clinical practice (b) were grouped by workplace (% urologists in public was less than % urologists in private healthcare centres; p=0.003 for ED; p=0.000 for PE). ED, erectile dysfunction; PE, premature ejaculation.
The lack of time available during patient appointments would be regarded as the main reason for failing to address the detection of ED or PE for >80% of the sample. In addition, one third of the urologists acknowledged not to use health electronic records (HER) in their patients (data not shown).
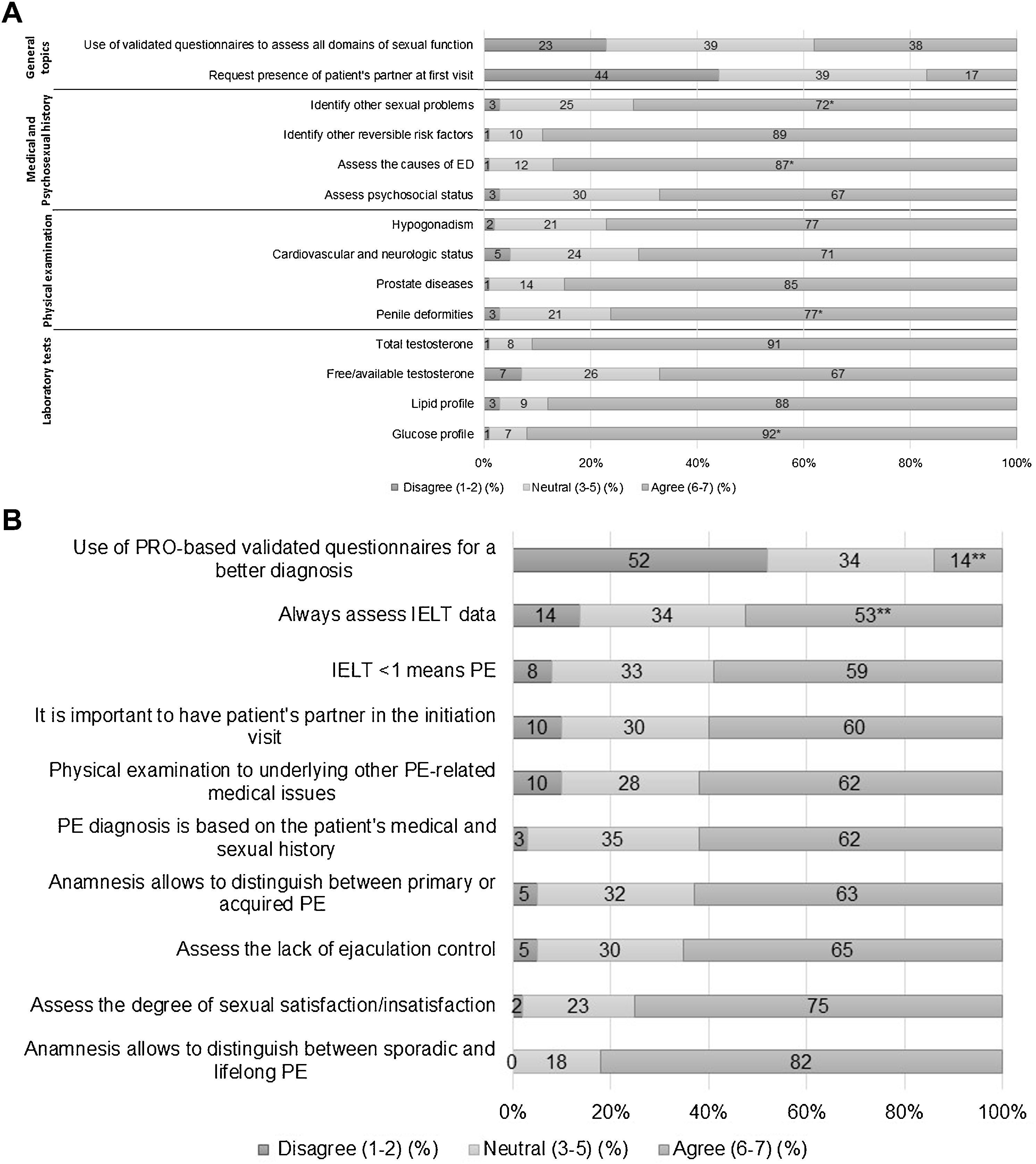
The urologists’ practice in the diagnosis of ED and PE was also investigated (Fig. 2). In the case of ED, the participants completed a structured questionnaire divided into four screening domains: general information related to ED, the use of each patient's medical and psychosexual history for diagnostic purposes, physical examination and laboratory tests (Fig. 2a). According to the general information requested, only 38% of the urologists use validated questionnaires to assess all domains of sexual function (e.g. IIEF, International Index of Erectile Function). 44% of the sample never asked for the partner to be present in the office during the visit for the initial patient evaluation.
Participants (n=188) respond to the questions about a set of statements related to the diagnosis of ED (a) and PE (b). When indicated, data are shown as a percentage (%) of agreement. Agreement score ranged from 1 (strongly disagree) to 7 (strongly agree). *Statistical differences among the surveyed population were observed when answers were grouped by workplace (the percentage of urologists in the public setting was lower than in the private setting). **Statistical differences among the surveyed population were observed when answers were grouped by workplace (higher level of agreement among urologists working in private healthcare centres; p=0.009 for the item ‘Always assess IELT data’; p=0.021 for the item ‘Assess the lack of ejaculation control’). PE, premature ejaculation; IELT, intravaginal ejaculation latency time; PRO, patient reported outcome.
Regarding the evaluation of the medical and psychosexual history that is reviewed in a visit with a patient with suspected ED, psychosocial status was the lowest-rated item by the study population (67%), compared to others such as identifying reversible risk factors for ED (89%), common causes of ED (87%) or other non-ED related sexual problems (72%). The attitude of the specialists to both specific physical and laboratory ED diagnostic tests was also outlined (Fig. 2a). Most physicians (range, 71%–85%) recommended the examination of penile deformities, prostatic disease, signs of hypogonadism and cardiovascular and neurological status for a minimal physical evaluation of ED. Among laboratory tests, glucose-lipid profile and total testosterone, were selected by over 90% participants in patient self-reported ED, and 67% of the sample used bioavailable or free testosterone levels (Fig. 2a).
Participants completed a structured list of 10 closed-questions about their preferences and attitudes experienced upon diagnosis of PE patients (Fig. 2b). Overall, 112–132 urologists (60%–70%) considered that patient history probing should involve a physical examination of the patient for underlying medical problems associated with PE, medical and psychosexual history and issues related to ejaculation control (mostly requested in private settings: 78% vs 64% in academic centres; p=0.021). More than 70% of the experts stated that they mainly took a simplified diagnostic approach to ascertaining satisfaction with sexual intercourse in making a distinction between constant and situational PE (which occurs with a specific partner in certain circumstances). Less than 60% of the consultants always asked the patient for data about the IELT and considered that when the value is <1 it is because they have PE. Only 14% of panellists trusted the use of patient-reported outcome (PRO) questionnaires to evaluate subjective symptoms and for a comprehensive collection of data. Unlike ED, our population mostly agreed to the partner being present in the office during the visit (Fig. 2b). Paradoxically, the panel revealed that about 44% of patients with ED (24% for PE; p=0.000) are always accompanied by their partners (data not shown).
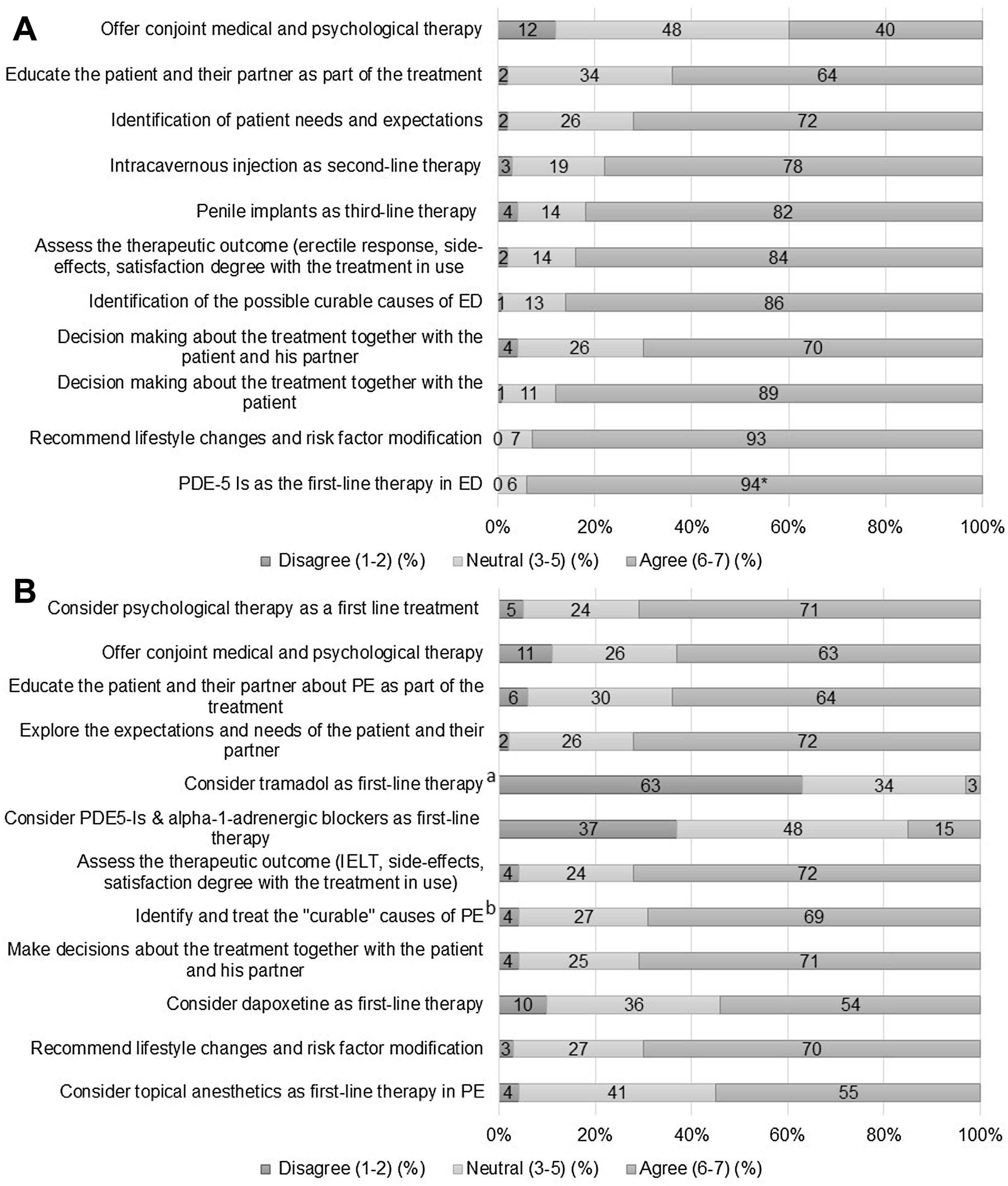
The recommendations for the treatment of ED and PE were rated by our study urologists (Fig. 3). Our questionnaire for ED indicated that over 90% of specialists agreed on the use of selective phosphodiesterase-5 inhibitors (PDE5-I), lifestyle changes and risk factor modification and shared decision-making with the patient (Fig. 3a). Other items were also chosen by an important part of the sample (80%–90%), such as the fact of treating first a curable cause of ED, assess the therapeutic outcome (erectile response, side effects, degree of satisfaction with treatment) or consider penile implants as a third-line therapy (Fig. 3a). Providing education and counselling to patients and partners was interesting (64%), although offering conjoint psychological and medical treatment was the lowest-rated option by the panel (40%). On the contrary, psychosocial therapy was among the three most supported recommendations for the treatment of PE, together with the identification of patient needs and expectations and the assessment of IELT, side effects and degree of satisfaction with the selected therapy (Fig. 3b). The use of topical anaesthetics or other drugs (dapoxetine) was considered by 55% and 54% of the sample, respectively. The use of tramadol as first-line PE treatment did not seem to be a good option (63%, disagreed; 34%, neutral).
Participants (n=188) respond to the questions about a set of statements related to the treatment of ED (a) and PE (b). When indicated, data are shown as a percentage (%) of agreement. Agreement score ranged from 1 (strongly disagree) to 7 (strongly agree). *Statistical differences among the surveyed population were observed when answers to the treatment of ED (a) were grouped by workplace (higher level of agreement among urologists working in public healthcare centres; p=0.036 for the item ‘PDE5-Is as the first-line therapy in ED’). ED, erectile dysfunction; PE, premature ejaculation; PDE5-Is, phosphodiesterase-5 inhibitors; IELT, intravaginal ejaculation latency time.
Table 1 illustrates the opinion of the panel about the role of these sexual conditions in male health, the level of communication of patients with their physicians and their partners, and the level of partners’ support and involvement. Our participants mostly agreed that “ED (or PE) affects a much larger population than is detected in clinical practice: underdiagnosis” (85% for ED; 75% for PE). Around 80% of the panel highlighted the problem of undertreatment for both disorders. ED was mainly understood as a possible sign of CVD. The need for more training courses or awareness-raising campaigns addressing the health hazard posed by ED and PE was also claimed. A significant percentage of the cohort (50%–75% for ED; 40%–55% for PE) remained neutral regarding the patients’ attitudes to talking about these disorders. Of the entire cohort of participants, 32% did not agree that a patient with an erection problem denied the existence of their disorder, although these patients generally prefer that the doctor initiate the discussion about ED, mainly in academic hospitals (30% public vs 17% private; p=0.005). This preference was also reported for patients with PE, who were hesitant to start a conversation about their sexual condition (Table 1). Interestingly, after a further evaluation of PE patients, urologists who worked in an academic hospital were significantly more likely to state that PE is still “taboo” (p=0.009). The concurrence of other pathologies is not a sufficient reason for a patient with an ejaculatory disorder to downplay the latter and this was acknowledged by 41% of the urologists. About 50% of the participants did not regard the partners as responsible for these sexual diseases or consider that the patients who came alone to the visit blamed them for it. Patients with ED seek professional advice at the request of their partner more frequently in the private than the public settings, although this difference was not statistically relevant (22% vs 14%, respectively; p=0.052). In fact, clinicians who work in private centres observed that women felt guilty and responsible for their partner's erection problem. Compared to ED, fewer partners would come with the patients to the PE visit, and they did not seem to participate very actively either (Table 1).
Participants (n=188) respond to the questions about a set of statements related to the perception of ED and PE in male health, the communication axis between doctors and patients, and between patients and their partners.
| Investigated item | ED | PE | ||||
|---|---|---|---|---|---|---|
| Disagree (%) | Neutral (%) | Agree (%) | Disagree (%) | Neutral (%) | Agree (%) | |
| Role of sexual dysfunction in health | ||||||
| •Common risk factors with a CVD | 2 | 4 | 94 | N.A. | N.A. | N.A. |
| •Training and/or awareness-raising actions are currently being carried out in ED/PE | 27 | 56 | 17 | 57 | 36 | 7 |
| •Not considered as an important health issue | 28 | 50 | 22 | 14 | 34 | 52 |
| •Considered as underdiagnosed | 2 | 19 | 79 | 2 | 18 | 80 |
| •Considered as undertreated | 1 | 14 | 85 | 2 | 23 | 75 |
| Communication line between physicians and their patients | ||||||
| •Patients deny the existence of ED/PE until it is evinced by the doctor | 32 | 55 | 13 | 29* | 54 | 17 |
| •Patients show a resigned attitude towards ED/PE | 11 | 72 | 17 | 27 | 50 | 23 |
| •Patients feel violent when talking about ED/PE | 22 | 53 | 25 | 14 | 47 | 39 |
| •Patients downplay the importance of ED/PE due to other problems/pathologies | 17 | 58 | 25 | 41 | 43 | 16 |
| •Patients talk openly about their sexual problem | 10 | 63 | 27 | 33 | 45 | 22 |
| •Patients prefer the doctor to initiate the conversation of their sexual disorder | 12 | 60 | 28* | 21 | 53 | 27* |
| •ED/PE is kind of a ‘taboo’ topic | 22 | 48 | 30 | 25 | 40 | 45* |
| Partners’ role in ED and PE | ||||||
| •Partner actively participates during the consultation, explaining their experience with the problem | 16 | 64 | 20 | 44 | 49 | 7 |
| •Partner is involved from diagnosis to treatment | 16 | 65 | 19 | 42 | 49 | 9 |
| •Patient attends the visit at the request of their partner | 15 | 70 | 15 | 27 | 59 | 14 |
| •Partner accompanies the patient | 20 | 65 | 15 | 54 | 38 | 8 |
| •Partner is the one who detects the problem | 14 | 76 | 10 | 31 | 55 | 14 |
| •Partner feels responsible for the problem** | 45 | 48 | 7 | 52 | 44 | 4 |
| •Men who come alone blame their partners about the sexual disorder | 54 | 42 | 4 | 64 | 31 | 4 |
| •Problem is even more important for the partners than for the patients | 51 | 46 | 3 | 37 | 50 | 13 |
When indicated, data are shown as a percentage (%) of agreement. Agreement score ranged from 1 (strongly disagree) to 7 (strongly agree).
ED, erectile dysfunction; PE, premature ejaculation.
Statistical differences among the surveyed population were observed when answers were grouped by workplace: the percentage of urologists in the public setting was lower than in private setting (p=0.005, for the item ‘Patients prefer the doctor to initiate the conversation about ED’; p=0.033, for the item ‘Patients deny the existence of PE until it is evinced by the doctor’; p=0.009 for the item ‘PE is kind of a Taboo topic’).
Finally, the study cohort was questioned about their clinical practice in the treatment or referral of these patients to other specialists for follow-up. Patients with ED and PE are usually diagnosed and treated by the actual urologist, and only referred to the andrologist in cases of severe ED or moderate-to-severe PE (data not shown).
DiscussionED and PE have a very strong impact on the emotional welfare and global quality of life of those who suffer them and their partners.16,17 However, despite having such a widespread and significant influence, they are still among the most underdiagnosed and undertreated disorders. This evidence supported the initiative led by ASESA to design the PANDORA study in order to depict a more realistic map of ED and PE in Spain from the perspective of urologists, patients and a representative sample of undiagnosed healthy male population. This survey presents the opinions, attitudes and perceptions of a representative and highly experienced population of Spanish urologists (n=188) in the management of these sexual disorders. Our panel work mostly in academic/public hospitals (134/188), although a significant number of them (41/188) also practice private medicine.
Sexual disorders, while related to aging,18 are not only present in the elderly. Indeed, patients >65 years are usually seen in public offices, whereas a significant percentage of patients <40 years were seen in private settings. It would seem to be logical for younger patients to prefer private practice. We hypothesize that the difficulty in getting time off work (public working hours are normally in the morning in Spain), as well as the younger population's greater purchasing power, might explain these results.
The reasons why patients who see the urologist for the first time with a diagnosis of ED are numerically higher in private centres cannot be determined on the basis of the available data, although it might be related to a common attitude among males of not to admit the occurrence of a sexual disorder, downplay its importance or find it as too uncomfortable to be discussed in front of any doctor. This means that few men seek for medical advice before being referred to a urologist in both public and private health. This was already demonstrated in our first publication, in which only 25% and 9.5% of 2515 healthy males had seen a doctor for a possible problem of ED or PE, respectively.15 Another study conducted in Spain with 512 men who had presented erection disorders reported that only 20% had sought medical advice.19 This picture is even worse with the diagnosis of PE, likely because men do not know how to self-diagnose PE and the need to see a doctor is then rarely emerged. Other studies reveal that the prevalence of self-reported PE may be lower than clinically-diagnosed PE because it is confounded with other sexual dysfunctions, particularly ED.20,21
Although ED and PE are the most prevalent sexual disorders, many clinicians are reluctant to discuss sexual concerns with their patients.22 Consistently with this, our first study from the PANDORA Project outlined that only 4.7% and 1.9% of surveyed men had been asked for ED and PE symptoms, respectively.15 In 2011, another Spanish study showed that up to 78% of 1531 males stated never been asked about sexual health by their doctor.23 These results are even more significant in the light of our current findings regarding the participants’ attitude during the anamnesis and in their current clinical practice in ED and/or PE. Therefore, most urologists only address sexual symptoms if the patient initiates a discussion about their sexual dysfunction or if these diseases could be considered as sentinel predictors for other comorbidities – diabetes, benign prostatic hyperplasia or heart disease. This observation was particularly notable during the evaluation of PE, which may be considered a subjective inconvenience, rather than an actual disease. This is in line with previous published surveys and is supported by current European Association of Urology Guidelines.24–26 The lack of proactivity among specialists proved to be particularly worrying in the public setting, mainly because of the limited time available to spend with the patient during the visit (80% of the sample). Barriers such us the awkwardness involved in discussing sexual issues, patient hesitation to discuss about sexual dysfunction and time constraints impede physicians to address these problems.27 In addition, the result of not having a HER or not including any questions about sexual health in patients’ electronic history do not help to account for these results. In this regard, the Atlas study14 underlined that ED data are highly not requested in the digitized medical history in Spain (73.5%), so it is a doctor's decision to probe the occurrence of ED or not.
There is no doubt that urologists are in the frontline for the diagnosis and treatment of male sexual dysfunction.28 Sexual dysfunction is in essence a self-reported condition, so the diagnosis is rather to discover the underlying aetiology than to demonstrate that the problem exists. Our panel were mostly more prone to assessing the common causes of ED (87%) and to identifying its reversible risk factors (89%) than to evaluating the psychosocial status of the patient (67%) or to using validated questionnaires to help assess all domains of the disease (38%). Our findings contrast with the recommendations of other authors to use an organized approach and/or validated questionnaires to sightsee all features of male sexual dysfunction and their burden on social life and wellbeing.29,30 However, despite the high number of questionnaires available to diagnose and assess ED severity, their clinical utility and validity are different, as one questionnaire may pick up on understated aspects that another may not.31 Although the physical examination of the patient will generally not help us to identify the aetiology of ED, most urologists agreed to carefully evaluate body habits, as well as the cardiovascular, neurologic and urogenital health.
The prevalent subjective connotation of PE has potential diagnostic consequences on physicians’ decisions. Therefore, our experts would take a simplified diagnostic approach that favours the use of a clinical and psychosexual history, physical examination, sexual satisfaction and self-control of ejaculation over PRO-based questionnaires and stopwatch-measured IELT. In line with the scepticism evinced by the panel in using these questionnaires to diagnose PE, Fusco et al.25 reported that diagnostic results can be very different whether they come from a questionnaire or are self-reported, and their role is discretionary in daily clinical practice.
A wide range of treatment options for ED may be tailored accordingly to a patient's specific goals. The majority of the participating urologists do a fairly good job of choosing the most relevant items for an appropriate therapeutic strategy: PDE-5 inhibitors, lifestyle changes and modification of risk factors, shared decision-making together with the patient, treating the cause of ED, penile implants and education and counselling for patients and their partners. More contemporary approaches of combining pharmacological and psychological therapy are not generally supported by the study participants, maybe because the successful outcome of such interventions is variable.17 PE has an important psychological burden and is closely related to depression, low self-esteem, anxiety, low sexual gratification, personal distress and relational difficulty.32 Indeed, psychosocial therapy is well received by most of the surveyed urologists.
Participant urologists assessed the role played by ED and PE in male health. Firstly, the vast majority of specialists agreed that both ED and PE affect many more individuals than are actually detected. In other words, Spanish urologists believe that both disorders are underdiagnosed and therefore go untreated. Our preliminary results showed that ED and PE are likely underdiagnosed in 3.5% of Spanish men with ED and in 11.7% of those with high to moderate risk of PE.15 It is difficult to explain the reason why urologists are more likely to take a neutral attitude towards considering ED as a real health problem, despite it may preclude the onset of CVD, even in men without any known cardiac disease at baseline.33 However, the reluctance to regard ED as a general health problem shown by our urologists is not entirely surprising, since the overwhelming majority sustained that very few training programmes and/or awareness campaigns on male sexual health are organized for them.
Sexuality continues to be a taboo, which is consistent with our observations in this study. Only half of the participating urologists have taken a firm stance on the quality of communication established between doctor and patient, and pinpointed the existence of a kind of “taboo” surrounding the question of talking about sexual problems in the office. The other half continued to evince a neutral attitude to approaching this. We understand that this finding is surprising and gives cause for concern.
It must be emphasized that there might be a need to regard ED and PE as shared sexual disorders that produce symptoms that are distressing for the man diagnosed with the dysfunction, but also for his partner. Furthermore, this survey revealed that partners somehow feel responsible for their partner's sexual problem and encourage them to seek professional advice. It is important for urologists to provide comprehensive information to patients and their partners when it is available. Indeed, most of the experts would include patients’ partners in the assessment in view of the role of the partner's input in the choice of therapy. In this context, scientific evidence shows that the partner plays a crucial supportive function in men seeking treatment for ED and in a successful long-term ED therapy.34
The limitations to our study include the heterogeneity of respondents, who represented many different regions in Spain with different programmes for urology patients, the small sample size of the group of urologists with private assistance compared to those with public assistance, and the participants may have been highly self-selected because completing the questionnaire was time-consuming. Therefore, whether or not our results can be mainstreamed to Spanish urologists overall is unclear, hence caution should be exercised in extrapolating these results. However, attending to the demographic characteristics of the panel, the categorization of workplace settings (private or public), and years of clinical experience are fairly representative of the Spanish urologist population. Another point to be challenged would be the way the questions for this survey were selected. Our questionnaire was designed to assess concisely only relevant practice information, as well as those determinant factor for the management of ED and PE. Despite these limitations, and up to our knowledge, there are no published surveys describing the current clinical patterns used among urologists for sexual dysfunctions. This study provides an overview of management strategies for ED and PE. In addition, it would be worth it to develop another survey among ED and PE patients. It might happen that their perception and treatment preferences diverge from those collected by urologists. However, this will be the PANDORA Project's next area of study.
ConclusionThe present report is the first-of-its-kind study has been developed in Spain, collecting the opinions, attitudes and perceptions of a representative population of highly-experienced Spanish urologists in the management of ED and PE. However, not all urologists are familiar with the diagnosis and management of the entire spectrum of these disorders. Increased efforts to enhance the education of urologists regarding the global management of these common sexual dysfunctions, including the use of validated questionnaires and considering the psychosocial approach for both diseases, should be a priority. Most urologists in Spain never use HER, or no questions about the sexual health are included in the patients’ electronic history, and neither do they proactively probe to assess possible sexual dysfunction. We hypothesize that gathering information about sexual behaviour in digitized clinical histories would reduce the number of underdiagnosed and undertreated cases of ED or PE.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FundingPANDORA is an initiative of the Spanish Association of Andrology, Sexual and Reproductive Medicine, which has been funded with an unconditional grant from Grupo Menarini España.
Conflicts of interestPuigvert-Martínez AM and Prieto-Castro R have received personal fees from Menarini. Artigas-Feliu R, Cruz-Culebra N and Illán-Mateo P work in the medical department of Menarini.
The authors would like to thank all the members of the PANDORA Project Regional Committee for their contribution to the development of the research and drafting of the manuscript: Alcaraz Reverte, José Pascual (Policlínico Hospital Perpetuo Socorro, Murcia); Arrondo Arrondo, José Luis (Hospital de Navarra, Navarra); Campos Juanatey, Félix (Hospital U. Marqués de Valdecilla, Cantabria); Corral Molina, Juan Manuel (Hospital Clínic i Provincial de Barcelona, Barcelona); Cortiñas González, José Ramón (Hospital U. del Río Hortega, Valladolid); Fernández Rosaenz, Jesús (Hospital Viamed Los Manzanos, La Rioja); Jorge Manuel González Suárez (Hospital Universitario Central de Asturias); Gutiérrez Hernández, Pedro Ramón (Hospital U. de Canarias, Santa Cruz de Tenerife); Jara Rascón, José (Hospital General U. Gregorio Marañón, Madrid); Leibar Tamayo, Asier (Hospital U. Infanta Sofía, Madrid); Martínez Jabaloyas, José María (Hospital Clínico U. de Valencia, Valencia); Mateos Blanco, Jesús (Hospital U. de Badajoz, Badajoz); Meijide Rico, Fernando (Hospital Povisa de Vigo, Pontevedra); Rodríguez Vela, Luís (Hospital U. Miguel Servet, Zaragoza); Rosselló Gayá, Mariano (Instituto Médico Rosselló, Balearic Islands); Valero Rosa, José (Hospital U. Reina Sofía, Córdoba); Vela Jiménez, Francisco José (Hospital General U. de Ciudad Real, Ciudad Real).