Obesity may lead to a serious deterioration in general quality of daily life and sexual functionality. Bariatric surgery is the most effective treatment method for obesity and related morbidities so far and it is better than some medical treatment modalities. In this study, we aimed to investigate the effects of bariatric surgery and especially sleeve gastrectomy, which has been currently performed in increasing numbers on female sexual functions and quality of life.
Materials and methodsA total of 53 patients were included to the current study. The participants were selected from eligible individuals who have undergone laparoscopic sleeve gastrectomy operation in our center between April 2014 and March 2015 dates. Age, body weights and body mass indexes (BMIs) of the patients were pre-operatively recorded. The patients have completed the Female Sexual Function Index (FSFI), Beck Depression Scale and SF-36 (Short form-36) forms before and after the surgery. Additionally, post-operative decrease in body weights and mean BMI were recorded.
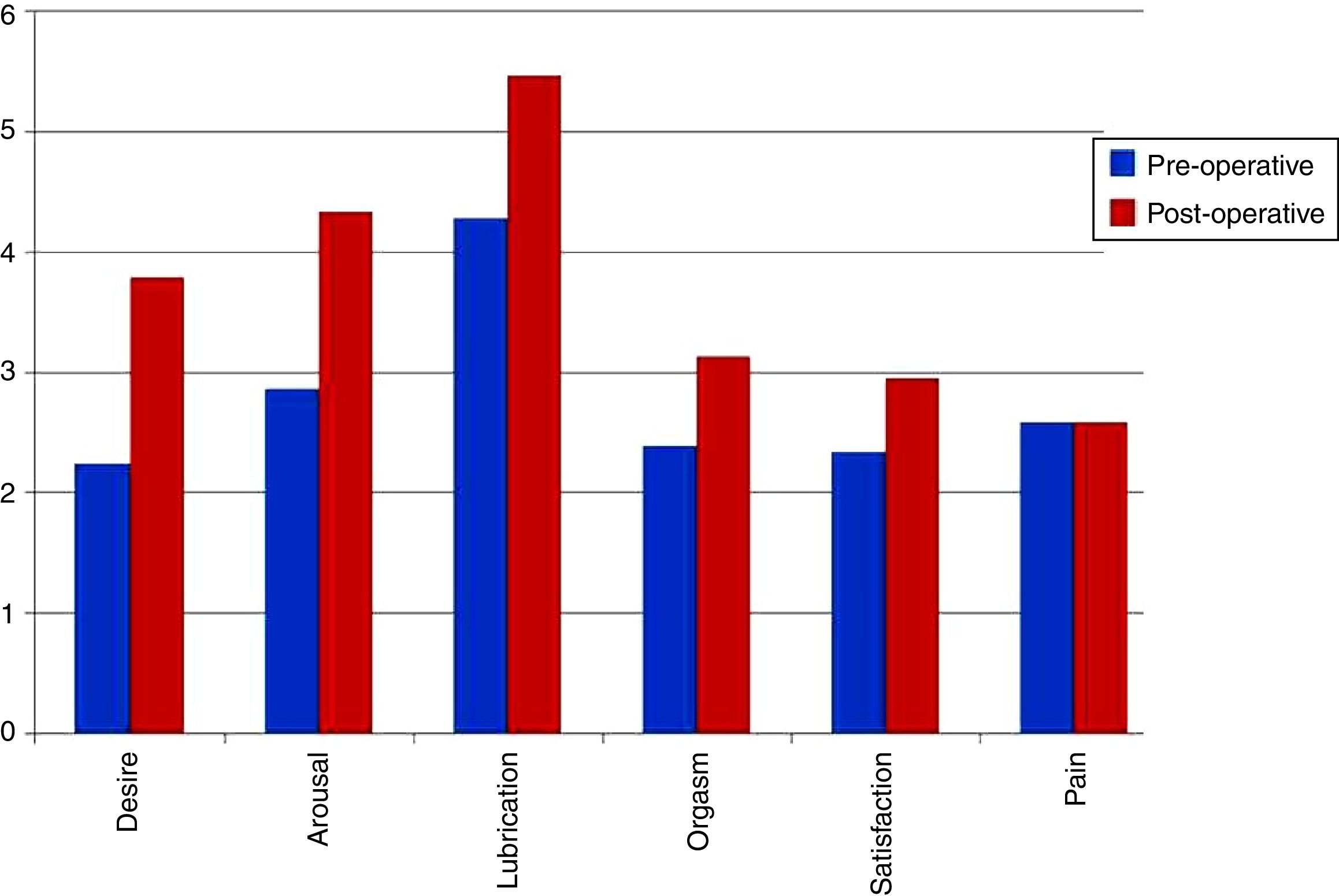
ResultsFollowing bariatric surgery, sexual functions of the female patients improved and total FSFI scores increased. When FSFI scores were analyzed, it was observed that sexual desire, sexual arousal, lubrication, orgasm and sexual satisfaction increased, while the pain parameter has not changed.
ConclusionRecent literature reveals that unfavorable effects of increasingly prevalent obesity on sexual functions cannot be denied. We think that sleeve gastrectomy can obtain considerable weight loss, improvement in self-esteem, decrease in anxiety, amelioration in sexual functions and general quality of life.
La obesidad reduce la calidad de vida en general y también la vida sexual. La cirugía bariátrica es uno de los métodos de tratamiento más efectivos contra la obesidad y sus comorbilidades. En este estudio nos propusimos analizar los efectos en funciones sexuales de mujeres y en su calidad de vida de la cirugía bariátrica, en concreto de la gastrectomía vertical, cuya implantación se está extendiendo en la actualidad, a través de las pruebas actuales comunes.
Materiales y métodosEn nuestro estudio se incluyó a un total de 53 pacientes seleccionadas entre las pacientes aptas a las cuales se les había implantado una manga gástrica por laparoscopia en nuestro centro entre abril de 2014 y marzo de 2015. Previamente se registró la información correspondiente a su edad, peso corporal e índice de masa corporal (IMC). Las pacientes completaron el Índice de la Función Sexual Femenina (FSFI), la Escala de Depresión de Beck y el Cuestionario de Salud SF-36 antes y después de la operación, y sus puntuaciones fueron registradas. Asimismo, se registraron las disminuciones de peso corporal postoperatorias y los IMC de las pacientes.
ResultadosTras la cirugía bariátrica, las funciones sexuales de las pacientes mejoraron y se registró un aumento de los valores del FSFI. Cuando se analizaron individualmente los parámetros incluidos en los valores del sistema del FSFI se observaron mejoras en el deseo sexual, en la excitación sexual, en la lubricación, en el orgasmo y en la satisfacción, mientras que el parámetro del dolor no sufrió ningún cambio.
ConclusiónLa bibliografía reciente revela que los efectos desfavorables de la cada vez más frecuente y extendida obesidad sobre las funciones sexuales no pueden negarse. Creemos que la cirugía bariátrica, como la colocación de mangas gástricas, genera una pérdida de peso considerable. Además, las mujeres se encuentran más atractivas a sí mismas, su autoestima crece y sus preocupaciones (ansiedad) mejoran con la consiguiente mejoría en sus funciones sexuales y en su calidad de vida.
Obesity is one of the most important health problems with respect to its related comorbidities. From the year 1980 up to now, the number of obese individuals has increased nearly two-fold. Based on 2008 annual data of The World Health Organization, there are approximately 1.6 million overweighted adults worldwide. This figure also includes 300 million obese female individuals.1,2 Sixty-seven percent of the total population of The United States of America (USA) are either overweighted or obese, while the incidence of obesity raises up to 40–50 percent in many European countries.3 According to the 2011 data, more than 40 million children smaller than 5 years of age are overweighted globally.1,2
Although it is possible to lose weight using non-surgical methods, 66% of the individuals regain their lost weights within a time period of 24 months. Since comorbidities associated with obesity mostly result in premature deaths and cause epidemics, surgery has become the first choice in the treatment of morbid obesity.4 Bariatric surgery is the only treatment modality which leads to nearly 15% weight loss in long term.5 Bariatric surgery is applied to more than 220,000 new cases in United States every year.6 When mortality, morbidity, cost-effectiveness, patient's satisfaction and weight loss rates are taken into consideration, laparoscopic sleeve gastrectomy (LSG) is one of the most frequently preferred surgical procedures.7 The other most preferred methods after LSG are as follows: Laparoscopic Roux-en-Y, Gastric Bypass (LRYGB), Laparoscopic Adjustable Gastric Band (LAGB) and Biliopancreatic Diversion with Duodenal Switch (BPDS).
Comorbidities as type 2 DM, hypertension (HT), heart diseases, hyperlipidemia and obstructive sleep apnea can accompany with obesity.8 Though sexual dysfunction (SD) has been initially defined as a psychological disorder, currently it is accepted that SD is a multifactorial disease with neurobiological, hormonal and psychosocial aspects.9 Obesity decreases general quality of life (QoL) and sexual functionality.10 Bariatric surgery is the most effective treatment modality for obesity and its related comorbidities and this method is superior to many other medical treatment alternatives.11 However, there is lack of information about the post-operative effects of bariatric surgery and especially LSG on general quality of sexual life. Although LSG has been firstly described to be performed as a restrictive component of duodenal switch operation, it was introduced into surgical practice as a risk-decreasing method in high-risk patients who cannot compensate prolonged procedures.12
Although female sexual dysfunction is one of the main subject of urology, it does not attract enough attention in urology practice. The role of sexual dysfunction in urology practice, which is associated with obesity frequency and obesity which are increasing rapidly nowadays, is gaining importance. We aimed to investigate the effect of LSG, one of the effective treatments of obesity in this study, on sexual functioning, depression and quality of life in women.
Materials and methodsThe current study was designed in a prospective manner. A total of 53 female patients who had undergone LSG for obesity between April 2014 and March 2015 dates were included to the current study. Participants who comply with the following criteria were excluded from the study: (I) patients who did not give their informed consent, (II) having previously treated for SD, (III) having a mental or psychiatric disease, (IV) having received a weight-loss therapy before, (V) being previously treated for incontinence or lower urinary tract symptoms, (VI) patients younger than 18 years of age and (VII) patients with respiratory tract diseases (i.e. chronic obstructive pulmonary disease) or a neurological disorder which might be associated with urinary symptoms.
Pre- and post-operative data of the participants including age, height, body weight and body mass index (BMI) were collected and evaluated. Patients have completed the Female Sexual Function Index (FSFI), Beck Depression Scale (BDS) and SF-36 (Short form-36) scales before and after the operation. FSFI is an inventory used to objectively measure the sexual functionality, which was firstly described by Rosen et al.13 Validity tests have been performed for this index in women with clinically established diagnosis of impaired sexual arousal. The FSFI scale consists of six subgroups, which evaluate six parameters including sexual desire, sexual arousal, lubrication, orgasm, sexual satisfaction and pain. Each item is scored between 0 and 5. After multiplication of the average score of a subgroup by factor loads, the minimum and maximum scores established from the scale were estimated as 36.0 and 2.0 points, respectively. BDS is a multiple-choice self-assessment scale consisting of 21 items used to measure the severity of depression in children and adults. In 1961, Beck et al. developed the BDS and then, revised in 1978 and then, translated into Turkish in the following years and tested for reliability and validity.14 Mean depressive levels were scored as follows: 0–21 pts (low depressive symptoms), 22–35 (moderate depressive symptoms) and 36–63 (severe depressive symptoms). Women with depressive disorders tend to score four points higher than men with depressive disorders.
SF-36 was translated into Turkish and tested for validity and very frequently used scale in evaluation of quality of life.15 This scale consists of 36 items and enables measurements of eight domains which include vitality, physical functionality, somatic pain, general health perceptions, physical role/emotional role/social role functioning and mental health. Scoring was summarized under two headings namely Physical Summary Scores (PCS) and Mental Summary Scores (MCS).
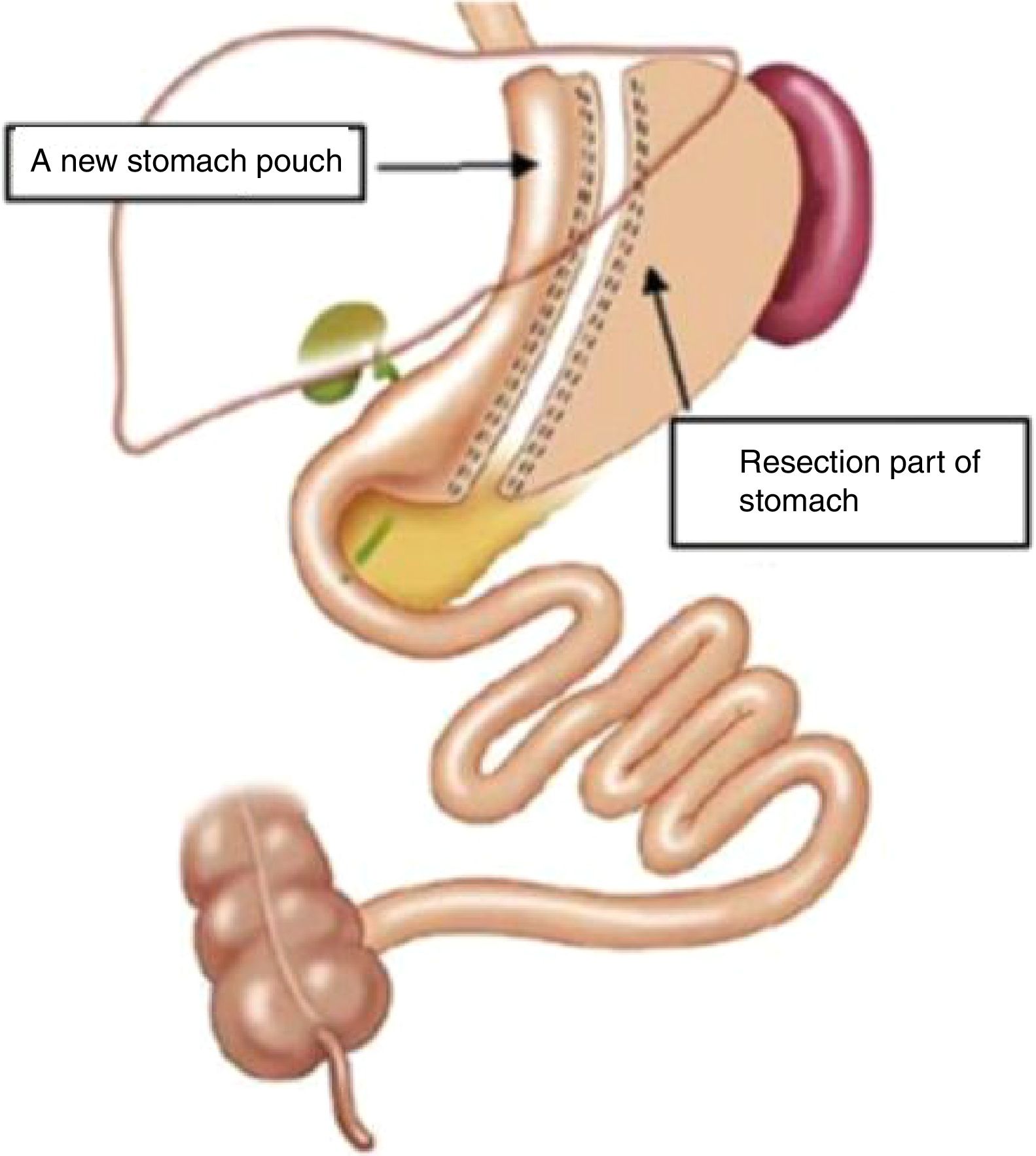
Surgical techniqueThe patients have undergone LSG operation and greater curvature was freed from 2 to 3cm proximal to the pylori up to His angle (ıncisura cardíaca). Gastric resection was subsequently performed (Fig. 1). In order not to leave a large fundus pouch behind, posterior dissection should be very well done so as to make His angle visible. Sleeve tube was fixated by suturing it to the omentum or gastrocolic adipose tissue. This procedure prevents kinking of the stomach from incisura angularis. LSG has become a very frequently preferred method alone or in combination with other methods in morbid obesity treatment.16
Statistical analysisIn statistical analysis of the established data, R For Windows x64 (v-3.2.4) statistical analysis software was used (R Foundation for Statistical Computing, Vienna/Austria, 2016, https://www.R-project.org). As we have only one study group consisting of 53 participants, paired samples t-test was used to compare the pre- and post-operative parameter variables. Pearson correlation analysis was used to investigate whether there is a relationship between the BMI and FSFI, BDS and SF-36 (PCS and MCS) parameters. P values less than 0.05 were considered as statistically significant.
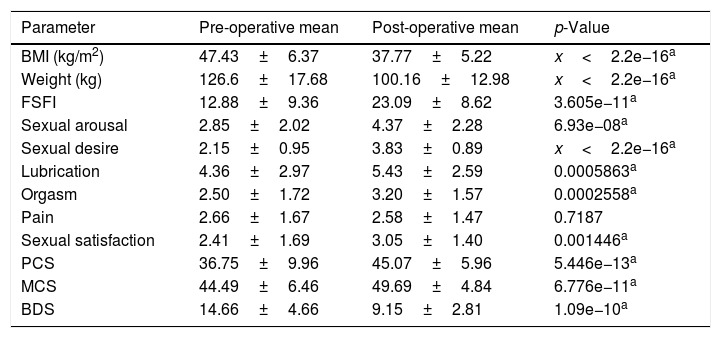
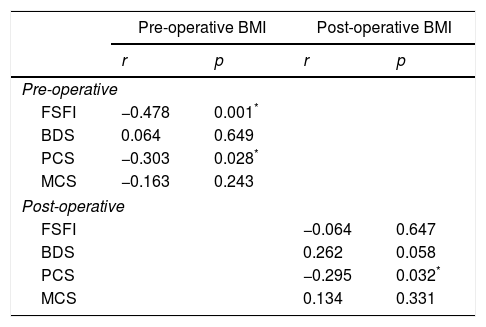
ResultsMean age of the patients was 34.85±9.38 years (range 18–54). There was a statistically significant decrease in average post-operative BMI value, body weight and BDS scores, when compared with the pre-operative estimates (p<0.001) (Table 1). There was a prominent increment in mean post-operative FSFI total score when compared with the pre-operative scores. There was a prominent increment in mean post-operative FSFI sub-groups severally sexual desire, sexual arousal, lubrication, orgasm, sexual satisfaction when compared with the pre-operative scores. Besides there was a prominent increment in mean post-operative PCS and MCS values when compared with the pre-operative scores (p<0.001) (Table 1) (Fig. 2). Pre-operative pain scores did not statistically differ from the post-operative values (p>0.05). Negative correlation ratio between the pre-operative BMI and pre-operative FSFI total score was 47.8% (p<0.05). And, negative correlation between the pre-operative BMI and pre-operative PCS total score was 30.3% (p<0.05). However, there was no relationship between pre-operative BMI and pre-operative BDS (p>0.05). Negative correlation ratio between the post-operative BMI and post-operative PCS was 29.5% (p<0.05). There was no statistically significant relationship with other post-operative correlations (Table 2).
Pre- and post-operative mean and standard deviation values of the measured parameters.
| Parameter | Pre-operative mean | Post-operative mean | p-Value |
|---|---|---|---|
| BMI (kg/m2) | 47.43±6.37 | 37.77±5.22 | x<2.2e−16a |
| Weight (kg) | 126.6±17.68 | 100.16±12.98 | x<2.2e−16a |
| FSFI | 12.88±9.36 | 23.09±8.62 | 3.605e−11a |
| Sexual arousal | 2.85±2.02 | 4.37±2.28 | 6.93e−08a |
| Sexual desire | 2.15±0.95 | 3.83±0.89 | x<2.2e−16a |
| Lubrication | 4.36±2.97 | 5.43±2.59 | 0.0005863a |
| Orgasm | 2.50±1.72 | 3.20±1.57 | 0.0002558a |
| Pain | 2.66±1.67 | 2.58±1.47 | 0.7187 |
| Sexual satisfaction | 2.41±1.69 | 3.05±1.40 | 0.001446a |
| PCS | 36.75±9.96 | 45.07±5.96 | 5.446e−13a |
| MCS | 44.49±6.46 | 49.69±4.84 | 6.776e−11a |
| BDS | 14.66±4.66 | 9.15±2.81 | 1.09e−10a |
Pre- and post-operative correlation analysis of the compared parameters.
| Pre-operative BMI | Post-operative BMI | |||
|---|---|---|---|---|
| r | p | r | p | |
| Pre-operative | ||||
| FSFI | −0.478 | 0.001* | ||
| BDS | 0.064 | 0.649 | ||
| PCS | −0.303 | 0.028* | ||
| MCS | −0.163 | 0.243 | ||
| Post-operative | ||||
| FSFI | −0.064 | 0.647 | ||
| BDS | 0.262 | 0.058 | ||
| PCS | −0.295 | 0.032* | ||
| MCS | 0.134 | 0.331 | ||
Pearson correlation analysis.
There is a gradually increasing information addressing the relationship between the obesity and the male SD. Central obesity and metabolic syndrome have some predictive outcomes for erectile dysfunction.17 Male obesity can lead or contribute to the following conditions: SD, endocrinopathy, aromatization activity, psychological and thermal effects, sleep apnea, accumulation of leptin and other minor toxins and possibly the inflammatory/obstructive compounds of the pathogenesis process of epididymitis.18 However, the relationship between the obesity and disturbances in female sexual functionality has not been well defined to date. Changes in sexual quality and the incidence of SD following bariatric surgery have only been assessed by a few authors with controversial results.19,20 Thus, there is an increasing demand to explore this neglected area of bariatric care, so that alterations in overall quality of life after surgical weight loss could be better understood. In this method, a narrow tubular stomach is constructed. Restrictive nature of LSG, decrease in ghrelin hormone production, rapid passage of food into distal segments and increase in peptide-YY (PYY) and glucagon-like peptide-1 (GLP-1) hormones are thought to induce weight loss.21 LSG is preferred in super obese patients and those with BMI<50kg/m2 who want to be treated with this method. In a systemic analysis of 2500 patients (median BMI 51.2kg/m2) who had been operated with LSG, average weight loss, complication and mortality rates were found as 55%, 8% and 0.19%, respectively.22 Remission rate of diabetes following LSG operation has been reported nearly 66.2% among the patients and it has also been mentioned that 15% of these patients might require a bariatric surgery intervention again.23
FSFI is a scale which evaluates the sexual functionality and dysfunction conditions and it includes six parameters including sexual desire, sexual arousal, lubrication, orgasm, sexual satisfaction and pain. When average subgroup scores were multiplied by factor loads, the highest score to be obtained from the scale was calculated as 36.0 and the lowest one as 2.0 points. Rosen et al. have multiplied the average FSFI scale subgroup scores with factor loads and calculated the average scores as 19.2 and 30.5 points in SD and the control groups, respectively.13 In another study in which The Turkish Adaptation of The Female Sexual Function Index was used for evaluation, an average score of 16.7 points was calculated for the control group.24 In our study, multiplication of FSFI scale subgroup means with their factor loads yielded an average pre-operative score of 12.93 points, which appears to be in consistent with SD. However, the corresponding post-operative scores increased up to 23 points. In the current study, sexual function improved in female patients who underwent bariatric surgery and their total FSFI scores increased and this finding was in accordance with the literature. When parameters included in the FSFI scoring system were separately evaluated, a significant improvement was observed in sexual desire, sexual arousal, lubrication, orgasm and sexual satisfaction domains, while any comparative difference was not detected in pain parameter. At this point, attention to ensure that the pain does not increase after surgery. We think that this pain palliation can be achieved by medical treatment in urology practice.
Bond et al.19 have conducted a study on 34 female patients with SD and emphasized that improvement in sexual function following bariatric surgery was not essentially related to weight loss. Thus, studies investigating the endocrineologic and metabolic parameters which would explain the etiopathogenesis of post-operative improvements in body appearance and quality of life induced by weight loss in patients undergone bariatric surgery and those exhibited minimum weight loss are required to accomplish these improvements.25–28 Depression condition and antidepressant agent use can affect the sexual functionality in women.29 Kadioglu et al. have reported that obesity had no significant relationship with FSD, but obese patients were in a more depressive mood than age-matched normal counterparts.30 In a study conducted by Bond et al.; it has been mentioned that bariatric surgery did not mainly affect the post-operative sexual function in women using antidepressants.19
In another study performed on 153 female patients, Janik et al. have reported that weight loss following bariatric surgery made the women feel themselves more attractive, increased their self-esteem and alleviated their concerns (anxiety) with resultant improvement in their sexual desire and increase in their responsiveness to sexual arousal.20 In our study, unfortunately, self-esteem and anxiety were not assessed. In our study, female patients were evaluated before and after the operation using the BDS and comparatively lower post-operative BDS scores were observed.
Synder et al. have analyzed the physical and mental quality of life of the women athletes and non-athletes in 2010 and found that the average PCS and MCS of the control group was 53.3 and 46.6 points, respectively.31 In a study performed in Turkey about the effect of rheumatoid arthritis on the overall quality of life, the mean PCS and MCS values established from the SF-36 scale applied on the control group were 51.28 and 41.43 points, respectively.32 In the present study, the mean pre-operative PCS and MCS values were 36.72 and 44.36 points in obese participants, which were apparently lower than the average scores detected in normal population. Whereas, the mean post-operative PCS and MCS values significantly improved and raised up to 45.01 and 49.7 points, respectively.
Janik et al. have reported that there was a negative correlation between BMI and post-operative sexual function and indicated that post-operative weight loss favorably affected sexual function in women and these improvements may be directly proportional to the percentage of weight loss.20 Also in our study, a meaningful correlation was found between the weight loss and improvement in sexual functionality, however change in BMI did not correlate with improved sexual function.
In numerous studies in the literature, it has been reported that post-operative weight loss improved the quality of life and sexual function in obese patients and this weight alteration was also independent from the performed surgical procedure.
In addition, when we consider the rapid increase in the rate of obesity in recently, we think that we can share our knowledge that sexual health can be treated by sleeve gastrectomy technique in obese female patients who suffer from sexual dysfunction or are understood to have sexual dysfunction when they are questioned in our daily urology practice.
More comprehensive and multidisciplinary studies which would analyze the relevant physiologic, medical and psychosocial factors are needed to be conducted in order to get more insight into this field of research in the future.
ConclusionRecent literature reveals that unfavorable effects of increasingly prevalent obesity on sexual function cannot be denied. We think that sleeve gastrectomy can obtain considerable weight loss, decrease in depressive disorders, amelioration in sexual function and general quality of life.
Disclosure statementAll of the authors who have taken part in this study hereby certify that the current paper has no conflict of interest and/or funding support from third party institutions or corporations in any means.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflicts of interest.