Sir John Charnley ushered in the era of total hip replacement over 50 years ago. His innovations of polymethylmethacrylate fixation of implants, polyethylene/metal bearing surfaces, standardized instrumentation, and clean air operating rooms revolutionized previous attempts to replace arthritic hips. In the United States, Charnley's principles and implants were adopted, investigated, and modified as they have been in most countries. His basic concepts and techniques remain valid, however, and total hip replacement is widely regarded as one of the most successful procedures in orthopaedic surgery. Over 400,000 hip replacements are now performed annually in the United States.
The accepted indications for total hip replacement changed and expanded over the years. An operation intended as a salvage procedure in elderly, low demand patients has evolved to being the preferred surgery for a wide variety of pathological conditions of the hip. The primary indication for THR remains endstage osteoarthritis. With our aging population in the United States suffering from an epidemic of obesity (recent estimates that one third of the American population is obese with a body mass index of greater than 30), the prevalence of primary osteoarthritis has markedly increased. When nonoperative care, including weight reduction, activity modification, ambulatory aides, and nonsteroidal antiinflammatory medications, fail to relieve the pain and disability of endstage osteoarthritis, total hip replacement offers a highly predictable treatment.
Inflammatory arthritis, principally from rheumatoid disease, historically has been another common indication of THR. Since the introduction of disease modifying anti-rheumatic medications several decades ago, however, the prevalence of advanced rheumatic destruction of the hip joint has decreased. Post-traumatic arthritis following fractures and/or dislocations of the acetabulum and proximal femur remain a frequent indication for THR.
Osteonecrosis with segmental collapse of the femoral head is an all too common indication for total hip replacement. With the widespread use of corticosteroids for numerous medical conditions, the high rate of alcoholism in the general population, and the increasing number of HIV patients on highly active antiretroviral medications, the incidence of osteonecrosis has increased in the United States as well as in many other industrialized countries.
Displaced fractures of the femoral neck in patients older than 60 years have become another common indication for THR. Several large retrospective studies as well as randomized clinical trials demonstrate that THR provides better functional outcomes and fewer complications compared to traditional techniques of internal fixation or hemiarthroplasty for displaced femoral neck fractures.
Less frequent indica tions for THR include primary or metastatic tumors of the hip joint and the residua of post-infectious arthritis.
Techniques in total hip replacementThe surgical technique in total hip replacement evolved over the last 50 years. While traditional Charnley cemented components remain popular in the United Kingdom and much of Europe, most surgeons in the United States currently use noncemented implants only. More importantly, the types of bearing surfaces changed dramatically, especially in the last 10–20 years.
Acetabular componentsAll orthopaedic centers now utilize strictly non-cemented acetabular cups (1). Indeed, most young orthopaedic surgeons do not know how to implant cemented acetabular cups in index arthroplasties. Noncemented hemispherical cups differ in design with variable microporous or plasma spray surfaces for osteointegration of new bone. Immediate fixation can be provided by spikes, fins, or screws on the cup. Whenever technically feasible, solid cups without screw holes are preferred so as to lessen the liner wear and diminish the effective joint space for spread of osteolysis.
Cup positioning is critical for a stable prosthesis. Ideally, cup anteversion should be from 10 to 30 degrees, and cup inclination from 40 to 50 degrees off the horizontal. Outliers from these preferred positions may predispose to dislocation and/or increased polyethylene wear. Accurate cup positioning may be achieved using body surface landmarks, intraoperative landmarks (e.g., the transverse acetabular ligament) or computer navigation.
In the last five years, trabecular metal coated cups have gained popularity in both primary and revision arthroplasties. The tantalum microporous dimensions of trabecular metal provide both an ideal roughened surface for immediate stability with trabecular bone as well as pore dimensions for rapid osteointegration of the implant.
Femoral componentsFemoral implants have undergone a similar evolution in design over the last 20 years. While cemented femoral stems are occasionally used (hybrid arthroplasty), noncemented stems now constitute around 80–90% of the market (2). Most modern noncemented femoral stems share a common generic design including
- 1)
Titanium metal composition with its favorable elastic modulus,
- 2)
A double or triple wedge configuration allowing for both immediate fit and fill of the medullary canal and minimal early subsidence for stability,
- 3)
A straight, collarless design,
- 4)
Multiple available sizes,
- 5)
Modularity for use in patients with significant proximal femoral deformity,
- 6)
Proximally, circumferentially coated surfaces with micropores between 100 and 600 microns,
- 7)
Precise instrumentation for insertion through small incisions,
- 8)
Variable offset necks for precise restoration of the abductor moment arm, and
- 9)
Optional hydroxyapatite coating of the porous surface for enhanced osteointegration. Despite these widely-used, common design features, numerous other stem designs are marketed in the United States.
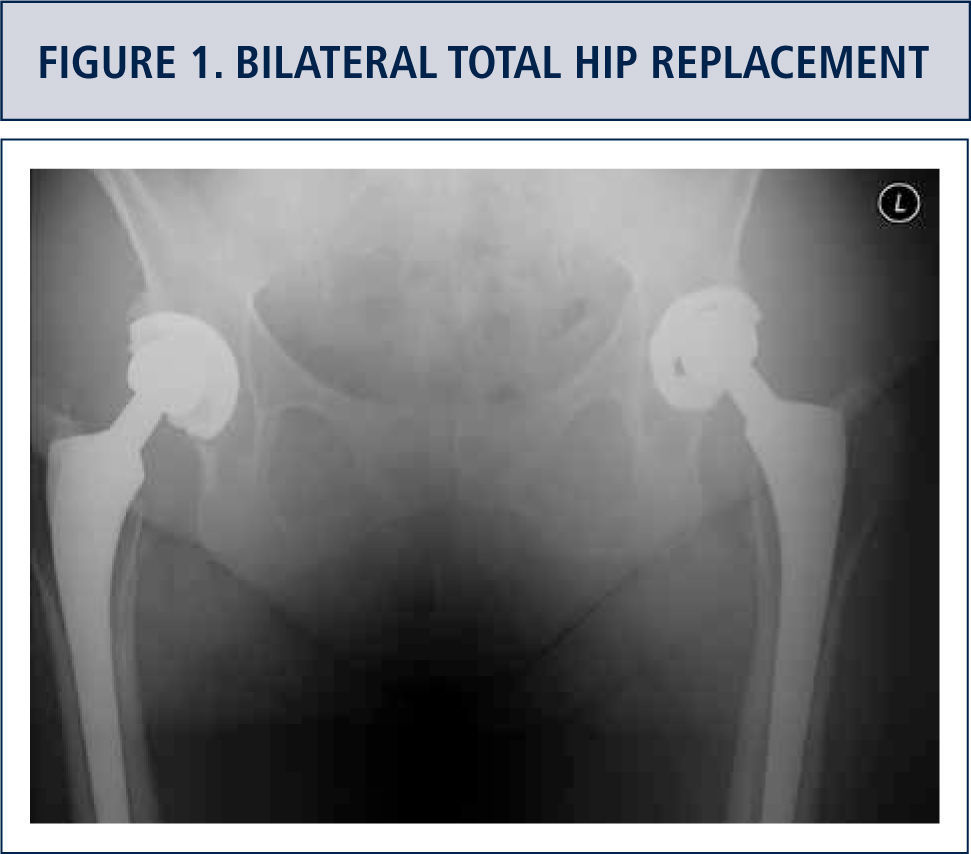
The primary long-term mode of failure ofTHR historically has been abrasive polyethylene wear resulting in osteolysis and subsequent component loosening (figure 1). Technological advances have led to the introduction of three potential solutions to this clinical problem.
Twenty year followup pelvis radiograph in a 65 year old female with bilateral total hip replacements for moderate acetabular dysplasia and osteoarthritis. Her functional status bilaterally is excellent though the radiographs demonstrate moderate linear wear of her conventional polyethylene liners.
First, highly cross linked polyethylene was first clinically used approximately 10–15 years ago (3). Both in laboratory testing and early clinical experience, its abrasive wear properties are 5–10 times better than conventional polyethylene. This biomechanical improvement along with changes in the sterilization, packaging, and storage of the polyethylene markedly enhances its longevity. Multiple recent, well documented studies of metal or ceramic on highly cross linked polyethylene demonstrate at an average of 10 years negligible wear and no osteolysis, even in highly active younger patients (3).
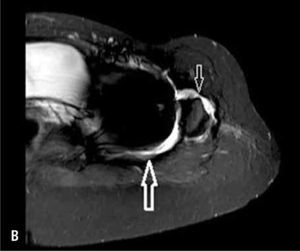
Second, metal on metal (MOM) bearing surfaces were reintroduced in Europe and then the United States for both resurfacing arthroplasty and conventional THR. In theory, the MOM surface creates less volumetric wear and thus, less osteolysis compared to metal on polyethylene. After initial favorable results in the United States, it use explanded to the point where 5 years ago, 35% of all bearing surfaces used were MOM. At that point, however, multiple arthroplasty registries and individual clinical trials reported higher failure rates with MOM surfaces both in resurfacings and primary THR using large diameter heads (4,5). A new complication of metallosis with adverse local tissue reactions (ALTR) and high metal ion levels in the blood was identified (figures 2a, 2b) (6). Early catastrophic failure with ALTR more recently has been attributed to corrosion of the head-neck taper, especially with the use of modular femoral heads of diameter of 36 mm or greater (7). Regardless of the etiology, source, and pathogenesis of this metallosis, governmental agencies in the United Kingdom and the United States have issued warnings on the use of MOM bearing surfaces. Their use has precipitously dropped to less than 5% of the American market for bearing surfaces.
Anteroposterior radiograph of a 35 year old female five years status post MOM total hip replacement for acetabular dysplasia and severe secondary osteoarthritis. She was initially pain free but now has diffuse left hip pain.
MARS MRI image of her left hip demonstrates fluid collections posterior (large arrow) and anterior (small arrow) to left hip suggesting either infection or metal-on-metal local soft tissue reaction.
A third and final solution to long-term wear is ceramic on ceramic implants. The combination of a ceramic liner in a metallic cup articulating with a ceramic head creates the lowest friction surface currently available for THR. Wear debris and osteolysis are negligible. Early problems with ceramic breakage and a poorly understood complication of audible squeaking of the ceramic on ceramic surface have been addressed and nearly eliminated with improved manufacturing and technical changes. Ceramic bearing surfaces are gaining wider usage in the United States.
Surgical approachesMany different surgical approaches for hip arthroplasty have been utilized. Currently, most surgeons use either a posterior (southern, Kocher), an anterolateral (Hardinge), an anterior, or a two incision approach. The proponents of each of these approaches claim specific advantages to their preferred dissection and approach. These theoretical and practical differences in approaches include the extent of exposure, the ease of insertion of acetabular and/or femoral implants, the accuracy of component positioning, the degree of abductor muscle trauma, and the rapidity of rehabilitation. All evidence-based medicine to date identifies no clinically important or significant differences between approaches. Similarly, computer navigated surgery for hip arthroplasty has not proven to improve radiographic or clinical results and now it is not widely used.
Unfortunately, “minimally invasive” surgery of the hip has been widely marketed in the United States. The theoretical advantages of such approaches to hip arthroplasty failed to be proven in clinical trials. Due to patient misconceptions, however, the concept remains extremely popular.
Results of total hip arthroplastyTotal hip arthroplasty tops the list of the most successful reconstructive surgical procedures. Both in terms of implant survivorship and patient perceived outcomes, hip arthroplasty consistently ranks as an excellent, cost-effective surgery.
Using Kaplan-Meier analysis, survivorship of conventional THR at 20 years stands at 85 to 90%. Revision surgery is necessary mainly during the first 1–2 years (for infection, dislocation, or periprosthetic fracture) but then plateaus after the first few years to a low rate of less than 1% annually. After 20 years, revision rates increase due to osteolysis and aseptic loosening. It is expected that with the use of the newer, more durable bearing surfaces, the high survivorship rates will be extended to 25–30 years. However, this enhanced survivorship may not be realized due to the fact that THR is now being performed on younger, more active and often more obese patients.
Patient perceived outcomes as assessed by quality of life measures also are outstanding following THR. Whether measured by SF-36 (general functional outcome), WOMAC (limb/disease specific measure) or a general clinical measure suchas the Harris Hip Score, total hip arthroplasty offers predictable improvements in patients’ pain and functional status. The improvements reported in these outcome measures exceed those of nearly any other orthopaedic or general surgical procedure.
The results after THR vary with socioeconomic status, gender, ethnicity, and psychological profile of the patients. Interestingly, recent data from our institution demonstrate that the improvement scores in SF-36 and WOMAC for Hispanic patients are higher than those in other ethnic groups. Nearly all patients however show statistically significant improvement in their postoperative scores. Pain and function improve up to one year after surgery and then plateau. Only a minor deterioration in scores occurs over time due to aging of the patient.
ComplicationsEarly postoperative complications include wound infection, deep venous thrombosis and/or pulmonary embolus, and dislocation. Late complications primarily involve osteolysis and aseptic loosening. Recent Medicare data reflect a changing pattern of complications with the near universal use of noncemented components and newer bearing surfaces. Early complications of periprosthetic fractures, dislocations and ALTR have increased while late complications of osteolysis/loosening are decreasing in prevalence. Regardless, the rate of complications is low. The Centers for Medicare and Medicaid Services (CMS) of the United States federal government has identified specific hospital-based quality standards for total hip arthroplasty. They include 30-day any-cause hospital readmission and various 90-day medical and surgical complications identified through a claims database. These hospital quality measures will be used to adjust hospital payments for this widely performed elective surgical procedure. Additionally, these data will be made public to assist patients in comparing outcomes between different hospitals (8,9).
ConclusionsTotal hip arthroplasty is a dynamic, ever-changing surgical procedure. Modern technology and instrumentation along with standardized surgical methods combine to make it a highly predictable, cost-effective reconstructive procedure for severely disabled patients. Until the advent of a reproducible biologic solution to osteoarthritis of the hip, total hip arthroplasty promises to remain an excellent treatment for patients suffering from endstage arthritis of the hip.
The author declares no conflict of interests with this article.