Male health has emerged as a new field of medicine as a response to dramatic disparities in male mortality and morbidity worldwide. A gender-focused view of the unique health needs facing boys and men have driven physicians and policy makers to establish gender-specific strategies for care delivery advocacy education, and research. Urologists are often seen as the most suited to address the broader scope of male health and as a community, they have been instrumental in leading both the definition of male health and collaborative initiatives to address the health issues facing men in the 21st century.
When considering male health the focus has historically been on single-system diseases, generally part of the genito-urinary system. Infertility, prostatic enlargement, urinary symptoms, and cancer were seen as male diseases to be treated in isolation by a urologist. Little thought was given to the inter-connectedness between organ systems, nor how behaviour or environment may contribute significantly to these illnesses. Over the last two decades certain questions have arisen which have forced those who care for men to reexamine male health. Why do men die sooner and live with more years of poor health compared to women? While a century ago, men and women had equal mortality rates; today men live 6 years less women in the United States 1 and in no country in the world do men out-live women. Men also live more years in poor quality of life. Male health expectancy, which measures both the quantity and quality of a healthy life, is much lower compared to matched females (2). Early male morbidity and mortality has significant detrimental effects on families, communities and economies. Men are at increased risk of premature death related to higher rates of cardiovascular disease, workplace accidents, suicide, and risky behaviours such as drunk driving. By addressing preventable causes of death and disability, those working in the field of male health have the opportunity to impact our global population on a social, psychological, financial, and health level.
BackgroundThe early evolution of male health has taken place over the past 20 years. Early work in the 1980’s focused on cardiovascular disease and sexual health (3-5). In 1992, the Men’s Health Network was established in the United States as a non-profit organization dedication to education. President Bill Clinton and the U.S. Senate passed a joint resolution in 1994 declaring a National Men’s Health week. The international focus on male health continued to grow over the subsequent years in the form of conferences, surveys and initiatives in several countries including Australia (6), Ireland (7), and the U.K. Following the first World Congress on Men’s Health in 2001, whose focus was to increase awareness and facilitate networks to address male health issues, there was the formation of the International Society for Male Health (ISMH). The societies’ goal is to bring together multiple disciplines to improve the health of men. In the same year, Europe developed the European Men’s Health Initiative to create policy and practice across the continent. The World Health Organization released shortly after the Madrid Statement which aimed to develop strategies to achieve gender equity, taking into account biological and gender-role differences of men and women (8).
The State of Men’s Health in Western Europe reported on the health needs of 190,500,000 men in 17 western European countries. The study found differences between the health of men and women across all age groups, as well as country-to-country geographic variations in disease states among men. Men were found to have higher rates of death than women as a result of ischemic heart disease, colon cancer, and accidental death. The key findings of the study were marked inequalities between both countries and genders, with gender related differences in population health needs. Men were at greater risk of all major diseases, including cirrhosis and ischemic heart disease, had higher rates of lung, liver, and stomach cancer, and were at greater risk of overall mortality than women9. This study provided part of the framework for the Vienna Declaration on the Health of Men and Boys in Europe, which was signed in 2005. In this Declaration, the signatories expressed a desire to improve public health and prevent disease by specifically addressing men’s unique health-care needs (10).
The world’s first National Men’s Health Policy was established in Ireland in 2009. Around the same time, the national Office of Men’s Health was established in the United States. In Canada, the Men’s Health Initiative of British Columbia was created as a multidisciplinary program for health promotion, risk assessment and reduction, disease prevention, community education, and advocacy for male health policy (11). The Australian National Male Health Policy in 2010, outlined six key areas to prioritize, including optimizing health outcomes, promoting health equality between groups of men, creating strategies for improving the health of men at different stages of life, focusing on prevention, and building evidence-based outcomes to inform future policies, programs and initiatives (12).
Care deliveryGiven the dramatic difference in health outcomes between men and women, those caring for men now see male health through a new perspective. A combination of genetics and society both contribute importantly to men. While men are physically built differently than women, social class, education, and employment heavily influence male health outcomes. Any approach to male health must take into consideration the role of masculinity as it pertains to men’s lifestyles and behaviours. Up to 80% of men refuse to see a physician until their spouse or partner convinces them (13). Stereotypes of masculine personalities, such as heavy drinking, heavy smoking, poor diet and sedentary lifestyle reinforce a negative view of male health, however they also provide prime areas to focus education, prevention, and intervention strategies.
While men’s physical advantage of strength has allowed them to excel in dangerous professions such as manual labor or combat, the accompanying sense of immortality has led many to engage in higher risk activities such as drunk driving and unsafe sexual practices. Physicians delivering care to men must be aware of the risks facing men and know how to screen for these harmful behaviours. Masculine men more often believe they can handle problems without help from others. For example, men with depression and alcoholism are less likely to seek appropriate assistance (14). Similarly, men have lower rates of depression compared to women, but have a 3-10 fold higher rate of suicide (15, 16). Screening for mental health disorders should be a standard of care for any physician caring for men, followed by referral to the appropriate experts. Few men will look anything like the ideal image on the cover of a magazine nor will they be interested in preventative strategies for health. However, when men present with erectile dysfunction, low testosterone, or lower urinary tract symptoms the opportunity to screen for metabolic syndrome and cardiovascular disease should be seized, especially given the evidence of their association (17-19).
Strategies for care delivery should address male health from childhood and adolescence, through middle age and old age. A broader variety of health-related areas should be addressed, including nutrition, physical activity, cardiovascular health, substance abuse, mental health, workplace safety, and regular health maintenance.
To assist the general and specialty physician to improve the care they provide for male patients, the American Urological Association (AUA) has developed the Men’s Health Checklist. The checklist covers the adult male through four stages of life—from ages 18-39 years, 40-49 years, 50-69 years, and >70 years. The checklist is divided into two sections relating to ‘urology-specific’ checks and ‘related health’ checks. Urology-specific checks—including urine voiding health, sexual health, and focused genitourinary examination—are designed to detect disorders such as lower urinary tract symptoms (LUTS), erectile dysfunction, hematuria, and infertility. Related health checks investigate weight, physical activity, metabolic assessment, mental health, PSA screening, and screening for cancers (including testicular, colorectal, prostate, bladder, and skin cancers). The Men’s Health Checklist provides an evidence-based roadmap—based on best-practice guidelines and systematic reviews—for patients and physicians alike. The checklist introduces health topics that might, otherwise, have been overlooked. Its popularity is evidenced by the fact that it is now available as an App (application) for multiple Smartphone platforms.
AdvocacyMany physicians within the urologic community have taken national and nternational leadership roles in male health policy and initiatives. As the preeminent advocacy and educational organization in North American urology, the American Urological Association (AUA) created the Committee on Male Health (CMH) in 2009 to develop a “comprehensive approach to address the issues of men’s health including education, community outreach, research, integration with other specialties, and support of local and national men’s health initiatives”(20). The Washington State Urology Society, USA, developed a similar advocacy and health policy campaign for male health education. As a direct result of this advocacy, the development and passage of legislation to guarantee that PSA screening tests would be included in all insurance plans for men (21).
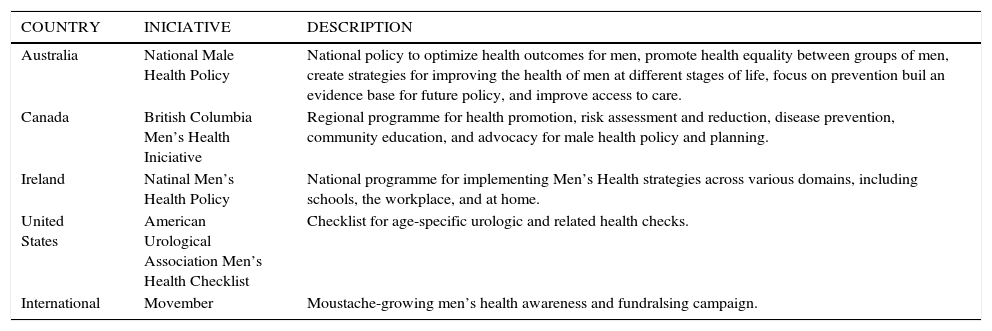
Advocacy and health policy have expanded into the national governments of Ireland and Australia, where federal male health policies have been enacted (7,11,12). Gender-specific approaches to health planning and policy are now implemented to address the specific discrepancies and needs of men. In Australia, the national Men’s Health Policy has committed to provide community-based health programs in the form of a Men’s Shed program. The program, established in 2006, organizes gatherings of men based on shared interests such as hobbies, activities, and crafts that can be performed in a backyard shed. The purpose of the “shed community” is to bring together men in a social setting and provide lay “shed leaders” the educational tools and materials to encourage conversations about health and wellbeing. The Men’s Health Initiative of British Columbia (MHIBC), an academic program set up by the Department of Urologic Sciences at the University of British Columbia, Canada, is a province-wide initiative “aimed at improving men’s health and quality of life through leadership, awareness and education campaigns, research, and dissemination of best practices in clinical care” (11). The goal of this program is to provide an umbrella organization for building partnerships in education, research, and advocacy for male health in the community and at all levels of governmental policy. See Table 1 for summary of current global male health initiatives.
Global male health initiatives
| COUNTRY | INICIATIVE | DESCRIPTION |
|---|---|---|
| Australia | National Male Health Policy | National policy to optimize health outcomes for men, promote health equality between groups of men, create strategies for improving the health of men at different stages of life, focus on prevention buil an evidence base for future policy, and improve access to care. |
| Canada | British Columbia Men’s Health Iniciative | Regional programme for health promotion, risk assessment and reduction, disease prevention, community education, and advocacy for male health policy and planning. |
| Ireland | Natinal Men’s Health Policy | National programme for implementing Men’s Health strategies across various domains, including schools, the workplace, and at home. |
| United States | American Urological Association Men’s Health Checklist | Checklist for age-specific urologic and related health checks. |
| International | Movember | Moustache-growing men’s health awareness and fundralsing campaign. |
Any successful male health advocacy initiative should use an evidence-based approach, which takes into consideration social, cultural, and economic factors. Gender-specific barriers to accessing health care and creating new ways of engaging men should be one of the first goals of any initiative. Redefining old stereotypes of masculinity into more modern concepts that embrace healthy living as a core male value are necessary. Being healthy and engaging the health care system as a principle of masculinity is a novel approach to make men take ownership of their own health. One successful advocacy campaign that has used this approach has been the Movember men’s health campaign. Established in Australia to raise awareness and funding for prostate cancer, it is now the world’s single largest sources of funding for prostate cancer research and education. Since 2004, Movember has acquired 1.9 million global registrants, raising a combined total of about $299 million USD. In 2012 alone, 1,127,152 participants from more than 20 countries raised over $141.5 million USD for men’s health initiatives, with a particular focus on education and research for prostate and testicular cancer (22). Participants grow a moustache during the month of November to raise both funds and awareness for male health. They have used a classically masculine feature, a moustache, to bring about discussion, awareness and advocacy for male health issues.
EducationThe AUA, through the mission of the Committee on Male Health has defined the issues surrounding male health and made recommendations on how these issues can be incorporated into the clinical, research, and educational realm of urology. By educating urologists to provide specialized care for a wider range of male health needs, the discipline strives to become the authority and coordinator of care for men in the health care system. Many lessons can be learned from Obstetricians-Gynecologists, who in many parts of the world have become the “woman’s health” physicians. Perhaps because they engage women early in their reproductive lives and establish long-term relationships as women move through the cycles of life, Obstetricians-Gynecologists have expanded their scope of education and subsequently practice to address broader areas of health including nutrition, weight reduction, smoking cessation, and cancer screening.
Similarly, through educating urologists on similar lifestyle interventions, they may be able to intervene earlier on modifiable risk factors, such as smoking and obesity, which are closely linked to the development of genito-urinary disorders later in life. An example of where education of urologists and other physicians could have a significant impact is in the area of prostate cancer, diet and lower urinary tract symptoms. The earliest cellular changes of prostate cancer occur in young men (aged 30-40 years) and diets that are high in fat and animal proteins promote the disease once it has begun to develop (23-25). Early interventions in the form of healthier diets and increased exercise could have a substantial effect on prostate cancer prevention for todays’ younger generation of men. Similarly, obesity and waist circumference have been associated with lower urinary tract symptoms (LUTS) (19,26,27).
In addition to the medical management of LUTS, the physician should become educated in ways to encourage healthier diets, improve physical fitness, and reduce alcohol and tobacco consumption. Smoking is a known risk factor for bladder cancer, with an odds ratio for males relative to females of 5.95 (95% CI 4.36-8.12), and diet has an established effect on the development of kidney stones and CAD (28,29). Men’s diets typically contain too few fruits and vegetables and too much salt and fat. 58 Educating men on adopting a healthier diet, such as the Dietary Approaches to Stop Hypertension (DASH) and Mediterranean diet, has been shown to result in significant reductions in the risk of hypertension and overall mortality (30). The DASH diet is enriched with vegetables, fruits, whole grains, and low-fat dairy foods, with minimal red meat and foods with added fat or sugar. The DASH diet has been shown to lower blood pressure (31,32) and even reduce the risk of developing kidney stones (29).
Physicians treating men should also understand that erectile dysfunction might be the first clinical sign of a hidden health condition and that cardiovascular and endocrine etiologies should be investigated. A recent meta-analysis examining the prediction of cardiovascular events and all-cause mortality in men with erectile dysfunction demonstrated greater pooled relative risk for these two conditions, especially in younger men and men with intermediate cardiovascular risk (33).To achieve a greater level of understanding of the urological and non-urological issues facing men, programs of education within residency training programs and continuing medical education (CME) curricula need to be instituted. The opportunity for physicians from diverse specialty backgrounds to cover male health exists and inter-disciplinary collaboration will be necessary for successful male health policy and programs.
ResearchEvidence-based research has emerged as a foundational pillar to male health policy.
The Australian National Male Health Policy has generated a complementary research program in the form of the Australian Longitudinal Study on Male Health, based out of the University of Melbourne. The objective of the study is to provide a national population-based account examining male health and its determinants including social, economic, environmental and behavioral factors that influence longevity and quality of life (34). The Australian Institute of Health and Welfare has started reporting on the health of Australian males with published health bulletins, the first of which was released in June 2011. Their research showed that two-thirds of adult males and one-quarter of boys are overweight or obese, and only two-thirds of males participate in sport or physical activity. Half of all men claimed to have been a victim of violence at least once in their lifetime and nearly half reported a history of mental health problems. In terms of health-care utilization, males’ account for a smaller proportion of primary care visits, hospitalizations, and mental health service appointments than women but are more likely to utilize the emergency services. The Movember men’s health campaign has organized an international research collaboration relating to prostate cancer biomarkers, entitled the Global Action Plan (GAP). The goal of this project is to connect prostate cancer researchers with practicing urologists, enabling them to link their biomarker research in ways that accelerate discovery in the fields of tumor biology, metastatic disease, and treatment resistance. As the discipline of Male Health continues to take shape and advance, more research in the field is being conducted. The International Society of Men’s Health now holds an annual Men’s World Health Congress to present the latest in clinical and research covering domains of urology, cardiology, endocrinology, psychiatry, oncology, family-health, public health, sociology and sexual medicine as they pertain to male health.
ConclusionAs a result of identifying men’s health disparities, the field of male health has evolved from single-system male genitourinary health to multidisciplinary models of care delivery. Local and national initiatives have developed models for gender-specific policies that address the unique health needs and barriers faced by men. Physicians will need to expand their expertise of current models of male health to include preventative health strategies, along with the impact of socioeconomic and behavioral influences. Education, research, and inter-disciplinary collaboration are all necessary to fully address the epidemics of obesity and cardiovascular disease, which are dramatically shortening the lives of men worldwide. Male health can be incorporated into existing models of clinical practice by acknowledging the disparities present and creating new models to deliver care to men. Male health is not an issue solely facing men; it is a global concern affecting spouses, children, communities, and countries.
Authors declare no conflict of interests.