The American Nurses Credentialing Center (ANCC) established the Magnet Recognition Program® (MRP) with the goal of identifying excellence in the delivery of nursing services. Magnet Recognition® is an organizational credential earned by achieving performance-driven standards. The standards, called “sources of evidence,” are organized in a framework that can be used to assess or improve an organization's culture and the impact of its nursing services.
This article describes the Magnet® framework and reviews the research evidence linking organizational culture, nursing practice, and patient outcomes. While experience with the MRP outside of the United States is limited, early reports suggest that it is positive. The authors conclude that over 30 years of incremental research findings support the benefits of the Magnet® framework, and that the journey to fulling the Magnet® requirements can have rewards both internal and external to healthcare organizations.
El Centro de Credencialización de Enfermeras Estadounidenses (ANCC, por su nombre en inglés: American Nurses Credentialing Center) estableció el Programa de Reconocimiento Magnet® (MRP, por su nombre en inglés: Magnet Recognition Program) con la meta de identificar la excelencia en la entrega de servicios de enfermería. Reconocimiento Magnet ® es una credencial para una organización entera, otorgada por el cumplimiento de estándares basados en el desempeño. Los estándares, llamados “fuentes de evidencia” (o “sources of evidence” en inglés), están organizados dentro de un marco conceptual que puede ser utilizado para evaluar o mejorar la cultura de una organización y el impacto de sus servicios de enfermería.
El artículo describe el marco conceptual de Magnet® y revisa la evidencia de investigaciones que conectan la cultura organizacional, la práctica de enfermería y los resultados clínicos de pacientes. Aunque la experiencia con el MRP fuera de los Estados Unidos es muy limitada, los informes preliminares sugieren que su impacto es positivo. Los autores concluyen que los hallazgos incrementales de investigaciones después de más de 30 años dan respaldo a los beneficios del marco conceptual de Magnet® y que el camino para cumplir los requerimientos de Magnet® puede tener recompensas tanto internas como externas para las organizaciones que brindan servicios de salud.
Magnet Recognition® from the American Nurses Credentialing Center (ANCC) is the highest distinction that a healthcare organization can receive for nursing excellence. The ANCC has been clear that Magnet® status is not a prize or an award, but rather it is a performance-driven credential (1). The goals of the program have been to:
- (a)
promote quality in a milieu that supports professional clinical practice.
- (b)
identify excellence in the delivery of nursing services to patients.
- (c)
provide a mechanism for disseminating best practices in nursing services.
The Magnet® framework can be used to assess organizational culture, and where needed, improve the culture. Evidence shows that Magnet® hospitals have higher staff retention rates; improved satisfaction scores, both for nurses and patients; and demonstrate more collaborative teamwork among caregivers (2-5). Thus Magnet® hospitals promote a favorable work environment that facilitates better patient outcomes. The rationale is that there is a relationship between organizational culture, its effects on nursing practice, and patient outcomes.
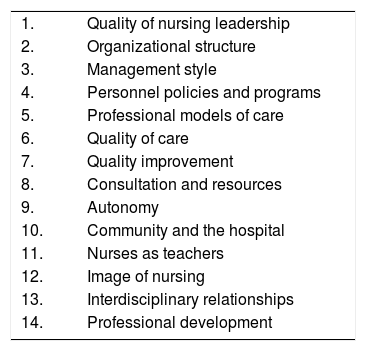
HISTORY OF THE MAGNET® FRAMEWORKThe Magnet® hospital concept originated with a study in the early 1980s that sought to explain why some U.S. hospitals were able to recruit and retain nurses during a severe national nursing shortage (6). There were 41 hospitals in the original study that were able to attract and retain professional nurses, which the researchers called the “magnet effect.” The study found these successful institutions had specific characteristics, listed in Table 1, which were subsequently labeled “the forces of magnetism.” (6,7) These characteristics reflect the organizational structure and culture, the work environment, nurse autonomy, and professional practice.
Forces of Magnetism.
| 1. | Quality of nursing leadership |
| 2. | Organizational structure |
| 3. | Management style |
| 4. | Personnel policies and programs |
| 5. | Professional models of care |
| 6. | Quality of care |
| 7. | Quality improvement |
| 8. | Consultation and resources |
| 9. | Autonomy |
| 10. | Community and the hospital |
| 11. | Nurses as teachers |
| 12. | Image of nursing |
| 13. | Interdisciplinary relationships |
| 14. | Professional development |
Ref. (7,8).
In the early 1990s, the American Nurses Association (ANA) developed a framework for evaluating hospitals that was based on the findings of the 1983 Magnet® research (7). They incorporated this framework into a program, set up the American Nursing Credentialing Center (ANCC) as a subsidiary of the American Nurses Association (ANA), and launched The Magnet Recognition Program® (MRP) the first organization to be Magnet® designated was the University of Washington Medical Center in Seattle in 1994. The first international hospital was recognized in 2002. Since then the growth of the program has been exponential. Currently 460 U.S. hospitals have Magnet® certification, or about 8.4% of the total. There are also 7 international hospitals currently holding the Magnet® certification, across Australia, Canada, Lebanon, and Saudi Arabia. Their international certification suggests that the Magnet Recognition Program® is applicable outside the U.S.A.
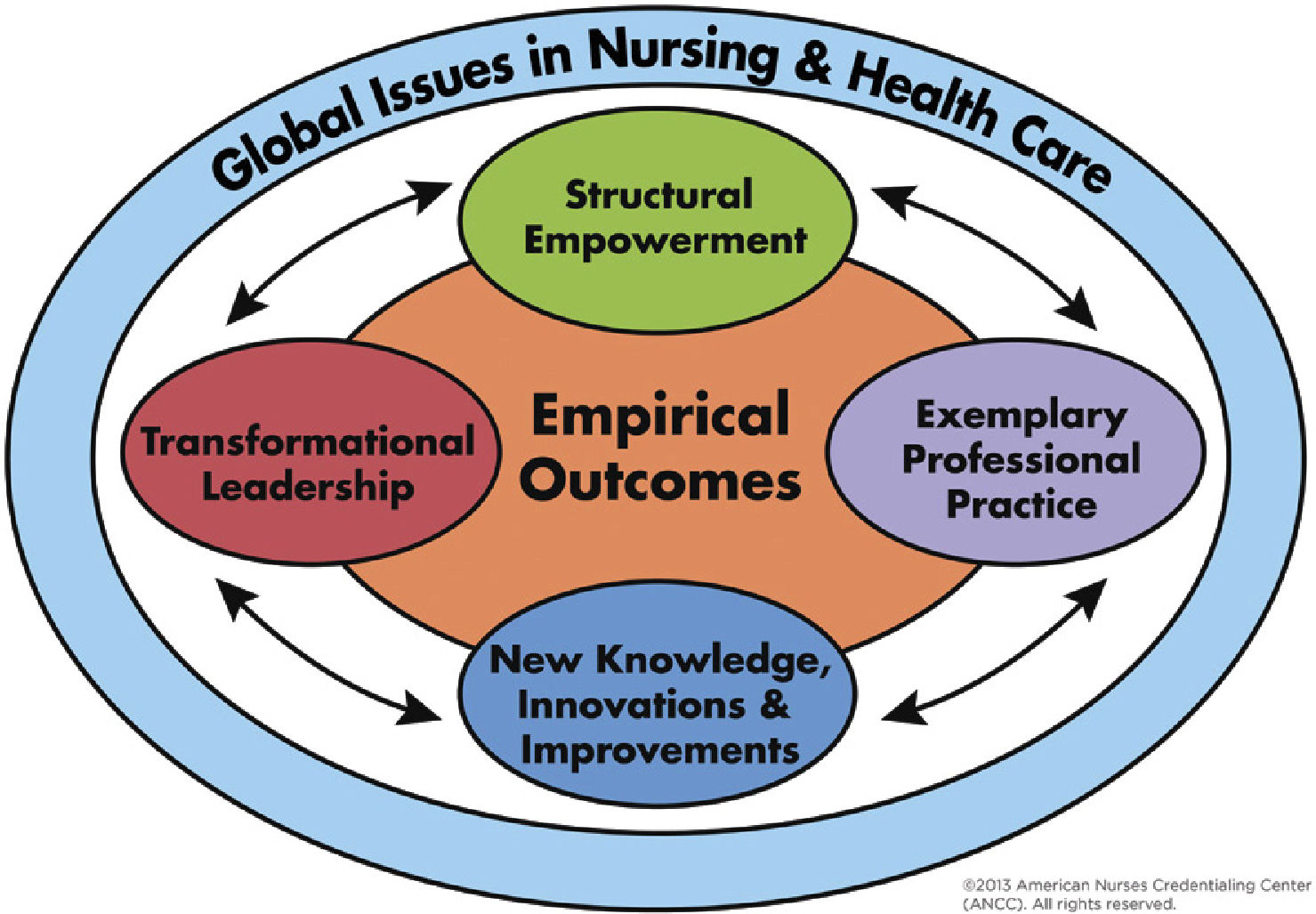
In 2008, the ANCC consolidated the 14 “forces of magnetism” into a parsimonious model, with the five components shown in Figure 1(8). These components include transformational leadership; structural empowerment; exemplary professional practice; new knowledge, innovations, and improvements; and empirical outcomes. Donabedian's classic model (9), which maintains that structure drives processes which produce outcomes, underlies the current Magnet® model. The focus on outcomes in the new Magnet® model represented a significant shift from structure and process evaluation, to greater evaluation of empirical evidence documenting improvement in outcomes for both patients and nurses.
According to Bass and Riggio (10), a transformational leadership style is characterized by motivating followers and helping them develop in a positive way. This style is the successor to the transactional leadership in which leaders have a vision and goals for the organization; and they meet those goals by directing the performance of their followers. Followers of a transactional leader will be rewarded or penalized depending on their performance. In contrast, the followers of a transformational leader not only look for an inspiration to guide them through uncertain times, but also seek autonomously to be performing at a high level. In this model, followers expect to be challenged and have the power to be involved in decision-making processes. Transformational leaders stimulate and inspire their followers to achieve remarkable results, and at the same time, develop their own leadership abilities.
The transformational nursing leader guides people to change and adapt to meet the demands of the future. This requires vision, influence, clinical knowledge, and strong expertise in professional nursing practice.
Structural EmpowermentStructural empowerment is reflected in organizational structure, personnel policies and programs, professional development, community outreach, and a positive nursing image.
Solid structures and processes developed by influential leaders provide an innovative environment where strong professional practice is discernable; and the mission, vision, and values come to life to achieve the best outcomes for the organization (11).
Leaders are responsible for cultivating a work environment that is extraordinary, where clinicians have the resources they need to deliver excellent patient care and where they feel their work is valued.
Exemplary Professional PracticeThe American Nurses Credentialing Center (12) bases exemplary professional practice on a professional practice model, which is “a schematic description of a system, theory, or phenomenon that depicts how nurses practice, collaborate, communicate, and develop professionally to provide the highest quality care for those served by the organization.” Exemplary practice is about how nurses interact with each other, patients, families, and interprofessional teams to promote and have influence over patient outcomes.
New Knowledge, Innovations and ImprovementsThis component works hand in hand with exemplary professional practice. It is the responsibility of nursing professionals to grow professionally and to help the profession grow. To ensure exemplary professional practice, the organization must support evidence-based practice. Nursing contributes to the organization and to the profession by generating new knowledge. It is an ethical and professional responsibility to provide evidence-based care and to generate new knowledge by conducting research. This research can then be used to improve the quality of care through innovative means (12).
Empirical OutcomesThe fifth component of the Magnet® model addresses the outcomes that are generated from the structures and processes that are in place in the organization. The outcomes are clinical outcomes related to nursing; workforce outcomes; patient satisfaction results; and organizational outcomes. Organizations can use data they are already collecting, however these need to be benchmarked against organizations that are similar (12) The results will show nursing excellence.
Applicants for Magnet® certification undergo a comprehensive process, which begins with an application to the ANCC. The next step is submission of written documentation demonstrating adherence to the Magnet® characteristics and providing “sources of evidence” on over 80 requirements (12). The documents are peer-reviewed and scored. Organizations that receive high scores on the written submission advance to a site visit where the content submitted is verified, clarified, and amplified. In a final step, on-site appraisers submit a report to the ANCC for review by a board of commissioners.
EARLY EVIDENCERemarkably little literature on the relationship between the organization and delivery of nursing services with patient outcomes appeared before 2000. Lundmark conducted an early systematic review of the research linking Magnet® environments to patient outcomes in 2008 (13). Lundmark noted that a limiting factor in this area of health sciences research has been the “inherent challenge of measuring organizational practice environments and the complexity of nursing's effects on patients.”
Lundmark (13) found that the majority of the Magnet® research “was dominated by cross-sectional survey studies with convenience samples.” In addition, the extant literature had two major limitations: (a) Biased sampling and (b) lack of valid and reliable measures for determining the presence of Magnet® characteristics. Organizations which have been Magnet® certified are self-selected, and comparison organizations may or may not have many of the Magnet® characteristics.
Lundmark (13) reviewed the early literature, from 1987-2005, in three areas. First, the studies conducted with the 41 reputational Magnet® hospitals from the original 1983 study. Second, studies that compared healthcare organizations with and without ANCC-recognition as Magnets®. Third, studies that investigated certain Magnet® characteristics to outcomes. This last group included one study of the degree to which Magnet® characteristics could be found outside the United States; and this was in Canada. Smith, Tallman, and Kelly (14) conducted a cross-sectional survey of 123 nurses from 13 rural Canadian hospitals. The survey had measures of Magnet® characteristics, including supportive management; professional autonomy and responsibility; nurse-physician relationships; and nurse-manager relationships. All categories were significantly, if modestly, correlated with job satisfaction except for nurse-physician relationships.
In general, Lundmark (13) concluded that the “magnet concept defines a framework for facilitating the professional practice of nursing” and that it has “demonstrated effectiveness in attracting nurses and shows promise for contributing to patient outcomes.”
LITERATURE REVIEWFor this article, a search for recent reviews of the literature on Magnet® characteristics was conducted using PubMed and Medline. Literature was appraised for its relevance to organizational culture and work environment, publication date (most recent 10 years), and the reliability of study findings. In addition, studies on Magnet® characteristics outside of the United States were examined.
Two reviews of the literature were found: Salmond, Begley, Breenan, et al. (2) and Lundmark, Hickey, Haller, et al. (15). The first review (2) considered 17 descriptive studies comparing Magnet®-designated hospitals to non-designated hospitals. They found evidence to support the positive effect of Magnet® designation on the professional practice environment. Magnet® status was associated with higher levels of nurse satisfaction, higher perceptions of the quality of care, and decreased intent to leave. But limited studies were found related to patient outcomes, and no studies considered economic impact. The second review (15)itemized positive outcomes found in Magnet® hospitals compared with non-Magnet® hospitals, with some sample findings given here with the most recent citation provided by the authors for each:
- •
Higher nurse job satisfaction in Magnet® organizations (3)
- •
Higher likelihood among nurses in Magnet® organizations to communicate about errors and participate in error-related problem solving (16), thereby contributing to improved patient safety.
- •
Higher adoption of National Quality Forum safe practices in Magnet® organizations (17).
- •
Lower patient fall rates in Magnet® organizations (18).
- •
Lower risk-adjusted rates of seven-day mortality, nosocomial infections, and severe intraventricular hemorrhage of very low-birth-weight infants (19).
Lundmark et al. (15) also documented the link between nurse practice environment and patient outcomes. They reviewed research that used the Nursing Work Index (NWI)—a set of survey items designed to measure characteristics of Magnet® environments—or its associated measure, the Practice Environment Scale of the Nursing Work Index (PES-NWI). (20, 21) Lundmark and colleagues (15)concluded that “superior nursing practice environments” were associated with better patient outcomes, citing studies that have supported this conclusion, as follows along with more recent studies:
- •
Lower nurse-reported adverse events (22)
- •
Lower rate of nurse occupational injuries (23)
- •
Higher patient-satisfaction (24)
- •
Lower rate of catheter-associated urinary tract infections (25)
- •
Lower patient mortality (26)
- •
Lower failure to rescue (27,28)
- •
Lower odds of having a hospital-acquired pressure ulcer (29)
International literature on the Magnet® program or Magnet® characteristics is scant, and largely anecdotal. In a seminal work, Aiken, Sloane, Clarke, et al. (30). studied the effect of hospital work environments on hospital outcomes across multiple countries. They analyzed primary survey data on work environments collected using the 28-item PES-NWI from separate cross-sections of 98116 nurses practicing in 1406 hospitals in 9 countries between 1999 and 2009. These countries included Canada, China, Germany, New Zealand, South Korea, Thailand, the UK (England and Scotland), and the USA. No Latin American countries were represented.
Aiken and colleagues (30)found considerable variability in the quality of the work environment across countries and within countries. Fully 26-44% of hospitals within each country were judged to have poor work environments. Hospitals with better work environments had higher likelihoods of reporting that the quality of care was “good” or “excellent,” and that their patients were ready for discharge. These findings were consistent across countries despite overtly different health-care systems.
One study of professional nursing practice in critical care units was conducted in Brazil (31). The aim was to assess characteristics of the work environment using a Brazilian modification of the Nursing Work Index (NWI). The method was a cross-sectional survey of 162 nurses working in intensive care units and the emergency department of a university hospital. The researchers found that autonomy, as well as relationships between nurses and physicians, were characteristics of the work environment that favored professional practice. Counterintuitively, however, control over the environment did not favor professional practice.
Two international sites have reported using the journey to Magnet® Recognition as a means to change organizational culture and improve patient outcomes. Walker and Aguilera (32) began their quest for Magnet® certification at St. Vincent's Private Hospital in New South Wales, Australia, by assessing the cultural climate using the NWI (modified for Australia). Subsequently, they embarked on a formal plan to engage staff, address gaps, and meet the standards. Working over some years, they achieved Magnet® Recognition in 2011. The authors note that healthcare facilities across the globe share similar challenges, including increasing patient acuity and greater prevalence of comorbidities; while at the same time, there is a more diverse nursing skill mix. They conclude, “Magnet is a robust, evidence-based framework for ensuring high levels of quality governance in nursing,” but the “Magnet advantage is yet to be fully appreciated internationally.”
Another Australian healthcare facility implemented the Magnet Recognition Program® as a means to change nursing workplace culture. Moss, Mitchell, and Casey (33)reported on the experience at The Princess Alexandra Hospital in Brisbane, Australia. They started with an employee engagement survey conducted in 2000, whose results reflected a workplace culture of “distrust, fear of reprisal, reluctance to challenge the status quo, acceptance of poor practice, denial, and lack of accountability.” These results catalyzed an effort to transform the culture using strategies aligned with the Magnet Recognition Program® (MRP). The site earned Magnet® designation in 2004, becoming the first hospital recognized as such in the southern hemisphere. They conclude that the MRP provided a framework to guide a clear path forward for nurse leaders in a non-US health care facility, and is a tool leaders can use globally.
While the evidence required for Magnet® recognition in the global community is the same as in the United States, the ANCC is aware of the “cultural, regulatory, environmental, and social factors in other nations that affect the practice of nursing” (12). The ANCC office has stated that they advise and assist global applicants as needed.
THE MAGNET JOURNEY®: A TRIP WORTH TAKING IN LATIN AMERICA?Latin America, like most areas of the world, is challenged to have sufficient health professionals to meet all of its population health needs and improve its population health outcomes. Responding to this challenge will require multiple approaches, including new technologies, new practices, new regulations, and transformative education. There is no single answer, however, one key effort by the Pan American Health Organization has been to promote interprofessional education (IPE) in health care to improve countries’ capacity to achieve universal health (34,35).
“Interprofessional” has a distinct meaning, and is not interchangeable with “multidisciplinary” or “interdisciplinary.” Interprofessional refers to all people who work to deliver care to a specific patient or population. On a hospital unit, this could include the nurses, the physicians, the pharmacist, and the people cleaning the rooms. By contrast, “interdisciplinary” or “multidisciplinary” refers to practitioners of a single profession who work across subspecialties; for example, the surgeon, radiologist, and anesthesiologist working on a case.
The Magnet Recognition Program® shares many of the same requirements as do interprofessional education and collaborate practice. These include promotion of a collaborative culture, a leadership model centered on professional development and outcomes, an organizational culture aimed at improving patient quality and safety, and practices rooted in sound evidence. These concepts were evident in the original “forces of magnetism” (Table 1), and are built into the new Magnet® model (Figure 1) respectively as transformational leadership, structural empowerment, exemplary professional practice, and innovations and improvements.
Over 30 years of incremental research have supported the benefits of implementing the Magnet® model and fulfilling its requirements, which in turn, suggests that the journey has benefits along the way toward the certification. Those benefits have been shown to reach well beyond the scope of nursing in a healthcare facility, with tangible results in patient satisfaction, staff satisfaction, improved financial outcomes, and improved quality and safety. This makes the journey a valuable exercise for all hospital executives and associates, not just for the nursing staff. The journey should be approached as an organization-wide and interprofessional effort if it is to be fully transformational.
THE BUSINESS CASEFor organizations that embark on the journey, the Chief Nursing Officer (CNO) will take the lead, but the Chief Executive Officer (CEO) and all other executive leaders must be in full support. The role of the CNO in health care organizations is to ensure that nursing services are well structured, processes and practices are evidence-based, and quality outcomes are achieved. The CNO, through his or her leadership, contributes directly to the organization's results including clinical, workforce, and financial outcomes; and ideally, there are metrics to measure and monitor each of these and thus demonstrate the tangible difference that can be made through the Magnet® journey. The institution needs to have a strategic plan for nursing, which drives toward achievement of outcomes and aligns fully with the organization's overall strategic goals, in order to meet the Magnet® requirements. Two recent case studies note the importance of linking the goal to achieve Magnet certification with the organization's strategic plan (36,37).
The support of the CEO and all executives is key because a financial investment is required. Case studies reported in the literature discuss the importance of the role of the CNO in leading and structuring the Magnet® journey, but it not a journey that the CNO alone can take. The CNO needs to make the business case for the return on the financial investment. This business case for Magnet® has been well-delineated by Drenkard (38), who calculated the range of cost savings that can possibly be achieved by a 500-bed hospital. There are both direct and indirect costs associated with the Magnet® journey. Direct cost include those associated with learning the requirements (books, conference attendance, consultants); followed by application fees, appraiser fees, site visit costs, and documentation preparation. For non-English-language applicants, the documents submitted must be translated and site-visitors may require translation services, which represent additional costs. Indirect costs include contracting with a vendor who can provide the surveys required to gather standard data, maintain a data warehouse, and benchmark the organization's data against a national sample. Organizations must collect and benchmark data on nurse- and patient-satisfaction, as well as on other nurse-sensitive clinical outcomes at the unit-level. In some nations, this is difficult to achieve because no comparative benchmarks exist (12).
Offsetting the investment, are cost savings, cost avoidance, and increased revenue. In Drenkard's analysis, financial benefits accrued from:
- •
Clinical quality, including fewer cases of pressure ulcers and a decreased fall rate.
- •
Nurse satisfaction, as higher engagement lowered turnover and vacancy rates.
- •
Cost, such as reduced cost of seroconversion in needle-stick injuries to staff.
- •
Efficiency and effectiveness gains from projects started to meet Magnet® requirements.
- •
Marketing, including publications and presentations in lieu of paid advertisements.
The total range of return on the investment was from $2308350 to $2323350 in U.S. dollars, on direct costs of $46000 to $251000. Drenkard (38) concludes that “securing only a modicum of this level of improvement will ensure a multifold return on the investment required.”
Three case studies emphasize that while the benefits of gaining the Magnet® certification are clear, measuring a hospital's need for Magnet® and readiness to apply are critical. Some CNOs start with an assessment (32,36), and these assessments may be conducted over time as the journey continues (37). At Emory Healthcare, Atlanta, each of its 5 hospitals gauged their readiness to apply by using a locally developed tool called the Magnet Readiness Index (MRI). Grant et al. (37). reports that there are 11 indicators on the MRI, which fall into 4 categories: Patient outcomes, nurse outcomes, organizational outcomes, and consumer outcomes. These are tracked on a monthly or quarterly basis at the unit-level within Emory, allowing nursing staff to use evidence to improve practice.
Moss, Mitchell and Casey (33) described how their nursing department undertook the journey to Magnet® recognition as a means to improve their nursing culture. They used their employment engagement survey to understand what was affecting the culture in their facility. In 2000, 54% of the survey responders reported they wanted to leave the organization. In that same year the turnover rate for nurses was 25%. By instituting Magnet principles they aimed to improve these numbers. In 2002 they applied for the Magnet recognition program and they succeeded in 2004. They reduced nursing turnover; since 2004 it averaged less than 8% and it was zero in 2015. The nursing engagement scores improved year over year with one exception in 2013. Engagement culture items improved from 23% to 42%. Nurses who were thinking of leaving the organization declined from 54% in 2002 to 28% in 2015. This underscores the importance of taking the journey.
CONCLUSIONMagnet Recognition® is an organizational credential that denotes quality and achievement. Over 30 years of incremental research have largely supported the link between the Magnet® framework and better patient outcomes. Internally, Magnet® certification assures the leadership and clinical staff at a healthcare institution that nursing services are well structured and have a performance-driven culture. Externally, Magnet® Recognition assures communities, consumers, and payors of the quality of care rendered. Any healthcare organization, globally, can embark on the journey to Magnet Recognition® and reap the benefits, both financial and in terms of the quality of care being delivered, regardless of reaching the final destination or not. Interestingly, it is not the destination that matters, but the transformational journey that accompanies the effort where the true gains lie for most healthcare organizations.
The authors are employed by Johns Hopkins Medicine International, which had a corporate affiliation with Clínica Las Condes for name use; consulting services; and knowledge transfer programs from 2007-2017.