Histoplasmosis is the most prevalent endemic mycosis on the American continent. It is caused by the dimorphic fungi Histoplasma spp. The infection is acquired by inhaling microconidia. It regularly starts in the lungs and then spreads to different organs. Skin involvement only occurs in 10% of cases. We present the case of a patient with a history of alcoholism. The disease initially manifested with non-specific respiratory symptoms such as cough with bloody sputum, dyspnoea, fever and multiple skin lesions. Using the PAS (periodic acid–Schiff) and Grocott stain histochemical techniques, the skin biopsy revealed intracellular microorganisms with peripheral nuclei and perinuclear ring, identified as Histoplasma capsulatum. The spread of primary pulmonary histoplasmosis led to the presentation of skin lesions. Correct diagnosis and treatment in this case helped to reduce the high mortality of the disease.
La histoplasmosis es la micosis endémica con mayor prevalencia en el continente americano. Es causada por un hongo dimórfico denominado Histoplasma spp. La infección se adquiere por inhalación de las microconidias. Se inicia regularmente a nivel pulmonar y posteriormente puede diseminarse a diferentes órganos. El compromiso cutáneo solo se da en el 10% de los casos. Se presenta el caso de un paciente con antecedente de alcoholismo que inició enfermedad con síntomas respiratorios no específicos como tos con expectoración hemoptoica, disnea, fiebre y con lesiones cutáneas múltiples. En biopsia cutánea y con las técnicas histoquímicas PAS y Groccott se demostraron microorganismos intracelulares, con núcleo periférico y halo perinuclear, identificados como Histoplasma capsulatum. La diseminación de la histoplasmosis primaria de pulmón conllevó a la presentación de lesiones cutáneas. El diagnóstico y tratamiento oportuno en este caso permitió disminuir la alta mortalidad de esta patología.
Histoplasmosis is the most prevalent endemic mycosis on the American continent. It is caused by the dimorphic fungi Histoplasma spp. Most infections are asymptomatic or self-limited; however, some individuals develop acute pulmonary infection or severe and progressive disseminated infection.1
The infection is acquired by inhaling microconidia, which, in the lungs, are converted into yeasts and attract phagocytic cells at the infection site. Because they are able to survive inside macrophages, they can reach numerous sites. In 10% of cases, the disease may present with skin involvement.
According to clinical presentation, histoplasmosis may be as primary cutaneous, acute pulmonary, chronic pulmonary, histoplasmoma, acute disseminated, subacute or chronic.2,3
Of all these, disseminated pulmonary histoplasmosis is the most common in immunocompromised patients and has the greatest mortality if timely treatment is not received.
Alcoholism is one of the main causes of immunosuppression as it suppresses innate and acquired immunity in the lungs of alcoholics and predisposes them to infections such as pneumonia, tuberculosis (TB) and opportunistic infections.4
We present the clinical case of a patient with a history of alcoholism whose definitive diagnosis was disseminated pulmonary histoplasmosis with multiple skin lesions.
Case reportA 58-year-old male with a history of alcoholism and a prisoner at the National Penitentiary Institute of Peru presented with clinical manifestations evolving over 4 months, characterised by weight loss of 23kg and respiratory symptoms, such as cough, haemoptysis, dyspnoea and fever.
A diagnosis of pulmonary tuberculosis was established based on clinical history and the high incidence of TB at the institute. He received treatment with isoniazid, rifampicin, ethambutol and pyrazinamide, which was suspended after 30 days due to liver toxicity data.
One week later, painful and pruriginous subcutaneous nodules appeared and steadily grew on the right hand, left forearm, face and left thigh. Three days later, he began to experience watery diarrhoea with mucous but no blood, approximately six times a day at a volume of 120ml per day.
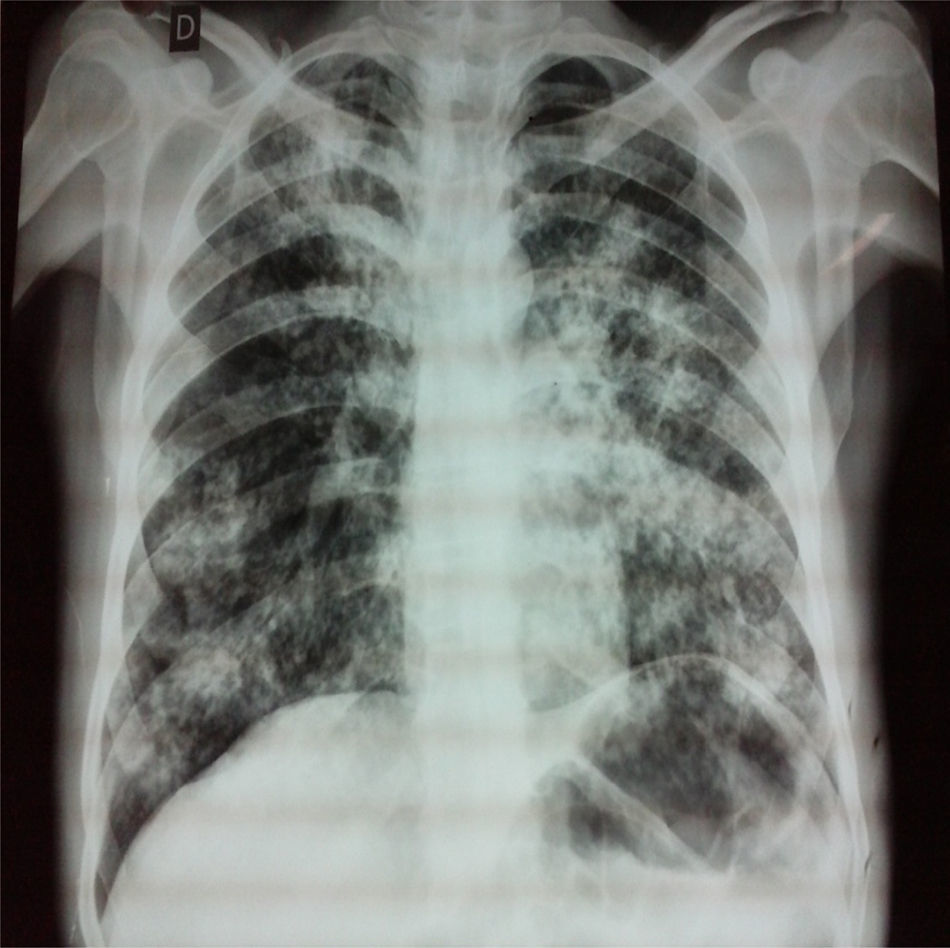
The physical examination revealed the above-described skin lesions (Fig. 1), in addition to an erythematous, maculopapular, flaking lesion on the outer edge of the left eyebrow.
Skin lesions due to histoplasmosis. (A) Back side of the right hand. Lesion measuring 1.5×2cm in diameter. It is a crateriform lesion with raised edges and no secretions. (B) Left forearm. Two ulcerated lesions with well-defined edges and yellowish secretion, the first measuring 1.5×1cm and the second, 4×3cm. (C) Posterior side of the left thigh. Two scabby lesions with yellowish secretion and a purplish, subcutaneous nodule with a semi-hard consistency, mobile and painful to the touch, the first measuring 5.5×3.5cm and the second, 3×3cm.
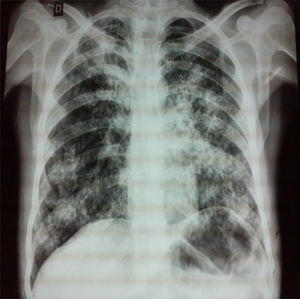
The chest examination revealed decreased respiratory movements of the left hemithorax, decreased lung sounds in both lung bases, bibasal crackles and diffuse rhonchi. The chest X-ray showed bilateral reticulonodular infiltrates and hilar involvement (Fig. 2).
The CBC revealed haemoglobin 10.1g/dl, haematocrit 29.6%, lymphocytes 11.9%, leukocytes 11,500/mm3, neutrophils 78.9% and platelets 665,000/mm3. Tests for RPR (rapid plasma reagin), HIV (human immunodeficiency virus), HTLV 1–2 (human T-cell lymphotropic virus types 1 and 2) hepatitis C virus and HBAg were negative; however, the anti-hepatitis B core test was positive.
The abdominal ultrasound showed the liver measuring 16cm with moderate steatosis, and normal spleen.
Mycobacterial cultures in solid Löwenstein–Jensen medium, taken from the samples extracted from bronchoscopy, sputum, gastric aspirate and stool, as well as the potassium hydroxide preparation, were negative.
Detection of antigen in serum and urine was not performed because the reagents were not available. In the biopsy of one of the skin lesions, using the PAS (periodic acid–Schiff) and Grocott stain histochemical techniques, we observed intracellular microorganisms with peripheral nuclei and perinuclear ring, diagnosed as cutaneous histoplasmosis.
Treatment was started with itraconazole at a dose of 400mg/day, and then at a maintenance dose of 200mg/day for 6 months. The pulmonary lesions resolved radiographically and the skin lesions shrunk.
DiscussionHistoplasmosis is an endemic and epidemic zoonotic disease in Equatorial Africa, North America, Central America and South America. Most cases in Europe are in immigrants from tropical areas.5
Sometimes, it is not possible to determine the event that precipitated contact with the fungus in patients with histoplasmosis. In our patient, we could not determine the epidemiological history.
This fungus is found in bird and bat guano.
In immunocompromised patients conditioned by HIV, HTLV 1–2, alcoholism, diabetes mellitus, corticosteroids or anti-TNF therapy, histoplasmosis may spread to other organs, affecting the lungs, tissues of the mononuclear phagocyte system, pancreas, intestines and meninges.
Immunocompromised patients develop very polymorphic and non-specific skin lesions on the face, arms and trunk. Diffuse reticulonodular infiltrate is observed mainly on the chest X-rays of patients with disseminated histoplasmosis, although it may be normal in up to 50% of cases.
Histoplasmosis requires deficient immune response in order to spread. For this reason, a history of alcoholism was considered to be an immunocompromising factor in this case, as alcoholism alters innate immunity in the lungs, thus inhibiting the recruitment of polymorphonuclear cells, altering bacterial removal, interfering with the differentiation and deterioration of the phagocytic function of alveolar macrophages and the expression of proinflammatory mediators. In acquired immunity, alcoholism interferes with antigen presentation, significantly reducing the absolute CD4+ T-lymphocyte count, decreasing interferon gamma production and suppressing the recruitment of CD8+ and CD4+ T-lymphocytes; this predisposes patients to acquiring different types of infection or contributes to more severe cases of infection.6,7
High clinical suspicion is required for the diagnosis of histoplasmosis. The main diagnostic method is skin biopsy, where Histoplasma spp. spores are observed.
Differential diagnosis of the histoplasmosis skin lesions should include infection by Cryptococcus neoformans, Herpes simplex, Molluscum contagiosum and Mycobacterium tuberculosis.
Disseminated histoplasmosis is treated in two phases. In the induction phase, itraconazole 200mg/8h is used for three days and then 200mg/12h for 12 weeks. In the maintenance phase, itraconazole 200mg/12h is used to prevent relapses.8
For reflection, we must still examine at what point the patient contracted histoplasmosis, given that he was not in an endemic area and no other cases of histoplasmosis were reported by the INPE [National Penitentiary Institute] in the same period.
In conclusion, we reported a case of histoplasmosis that spread cutaneously in a patient who was predisposed due to a history of alcoholism, which, as discussed, may have depressed his innate and acquired immunity, leading him to present one of the most uncommon and serious forms of histoplasmosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that they have no conflict of interests.