Necrotising enterocolitis (NEC) is an acute inflammatory condition of the colon involving a wide range of diseases with one end result: necrosis. This disease entity is very common in preterm infants, since 5–10% of premature babies weighing less than 1.5kg are believed to suffer from it, and it has a mortality rate of around 50% of cases.
ObjectiveTo describe the clinical and pathological characteristics of 24 patients with an established diagnosis of NEC and to identify their characteristics in terms of demographics, concomitant diagnoses and treatment response in order to provide preliminary data for designing prospective studies and future medical interventions.
Materials and methodsInformation for 24 autopsied neonates who died of complications of NEC between 1993 and 2013 was compiled and analysed retrospectively.
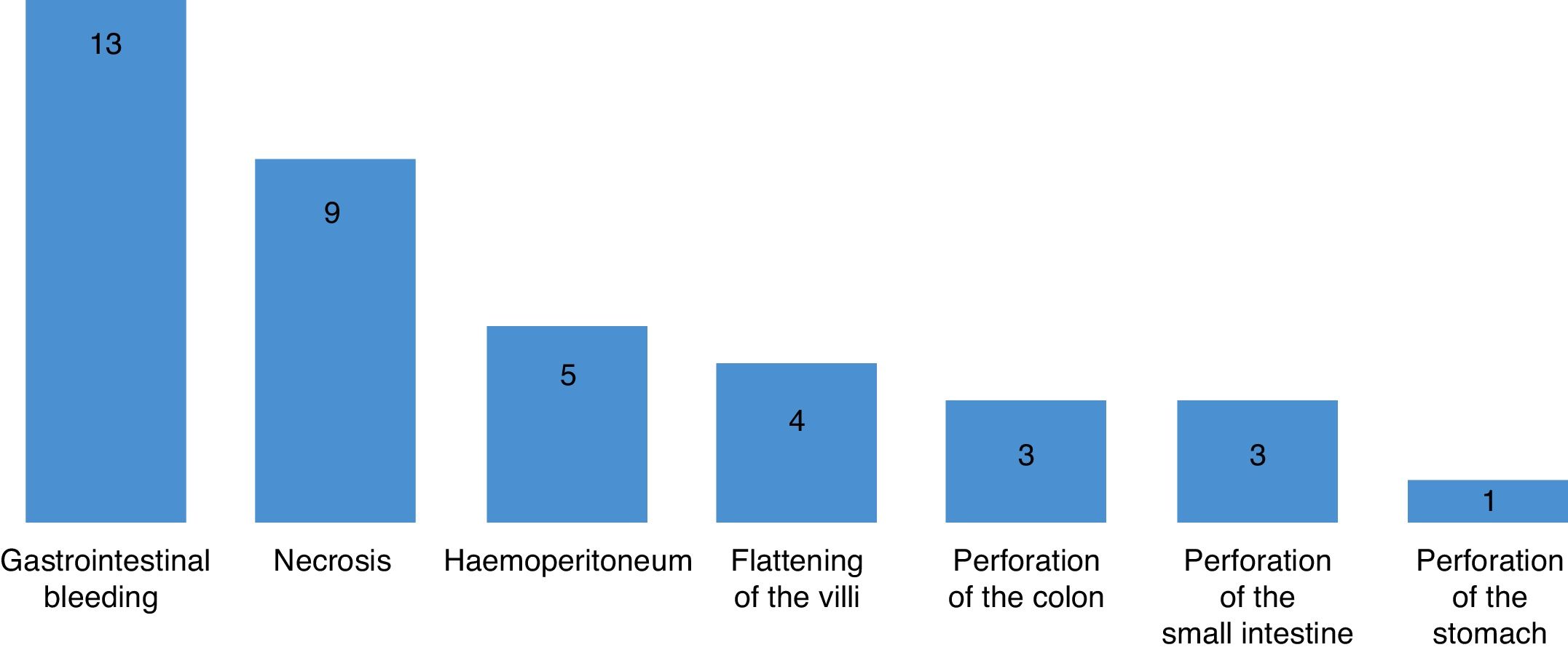
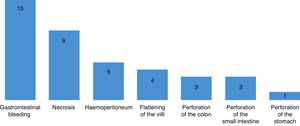
ResultsOf all 24 cases diagnosed with necrotising enterocolitis, only 15 were diagnosed clinically; all others (9 cases) were diagnosed post mortem. During autopsy, the most common finding was bleeding in different gastrointestinal segments (n=13 patients [53.9%]), followed by necrosis (n=9 [37.5%]) and perforation (n=10 [41.6%]). Four of the eight cases in which the Bell's clinical stage was reported could not be correlated with the pathological findings.
ConclusionsAs NEC is a disease with a high mortality rate, it is necessary to increase our knowledge of the demographic and clinical characteristics of patients with the disease to make a diagnosis that enables the patient to have early access to efficient therapeutic interventions. Our results demonstrate broad difficulty in the clinical diagnosis of this condition, as well as a weak relationship between the clinical stage reported and the pathological characteristics found during autopsy. The significance of this case series lies in its demonstration of the lack of accurate knowledge and identification of the clinical and demographic characteristics of patients with necrotising enterocolitis and the need for greater understanding of the pathophysiological foundations of this disease.
La enterocolitis necrotizante (ECN) es un padecimiento agudo inflamatorio del colon que involucra un amplio espectro de enfermedades con un resultado final, la necrosis. Esta entidad nosológica es muy frecuente en neonatos pretérmino; ya que se considera que del 5 al 10% de los prematuros que pesan menos de 1.5kg la padecen, teniendo una mortalidad cercana al 50% de los casos.
ObjetivoDescribir las características clínicas y anatomopatológicas de 24 pacientes con diagnóstico de ECN establecido, e identificar sus características demográficas, de diagnósticos concomitantes y respuesta a tratamiento con el fin de proveer datos preliminares para diseño de estudios prospectivos e intervenciones médicas futuras.
Materiales y métodosSe recopiló y analizó retrospectivamente la información de 24 casos de autopsia de neonatos que murieron a causa de complicaciones de ECN en el periodo de 1993 a 2013.
ResultadosDel total de 24 casos con diagnóstico de enterocolitis necrotizante en solo 15 el diagnóstico fue establecido clínicamente, ya que en el resto (9 casos) el diagnóstico fue postmortem. Durante la autopsia el hallazgo más frecuente fue la hemorragia en diferentes segmentos gastrointestinales n=13 pacientes (53.9%), seguido por la necrosis n=9 (37.5%) y la perforación n=10 (41.6%). En cuatro de los ocho pacientes en los que se reportó el estadio clínico de Bell no pudo correlacionarse con los hallazgos anatomopatológicos.
ConclusionesAl ser una enfermedad con una alta tasa de mortalidad es necesario aumentar nuestro conocimiento acerca de las características demográficas y clínicas de los pacientes con ECN, para poder establecer un diagnóstico que permita al paciente acceder a intervenciones terapéuticas eficientes de manera temprana. Nuestros resultados demuestran amplia dificultad en el diagnóstico clínico de este padecimiento, así como poca relación entre el estadio clínico reportado y las características anatomopatológicas encontradas durante los estudios de autopsia. La importancia de esta serie de casos radica en demostrar la falta de conocimiento e identificación certera de las características clínicas y demográficas de los pacientes con enterocolitis necrotizante y la necesidad de una mayor comprensión de las bases fisiopatológicas de esta enfermedad.
Necrotising enterocolitis (NEC) is the main cause of death in patients in the neonatal intensive care unit.1–3 It is an acute inflammatory condition of the colon involving a wide range of diseases with one end result: necrosis and subsequent intestinal perforation, leading to devastating consequences in some cases. It is common in preterm infants and a significant cause of morbidity and mortality in this age group, based on reports which indicate that 5–10% of premature babies weighing less than 1.5kg suffer from it. Its mortality rate is up to 50% of cases, depending on the severity of the clinical signs and symptoms.5,6
Prematurity is the main predisposing factor for NEC due to the anatomical and functional immaturity of the gastrointestinal system, characterised by defects in motility, digestion and regulation of intestinal circulation, resulting in failures in the function of the intestinal barrier. NEC rarely occurs in full-term infants. Therefore, an older gestational age is a protective factor.7–9 Similarly, the severity of NEC has been found to be inversely proportional to birth weight, as have other risk factors such as membrane rupture, urinary tract infection and respiratory distress.9,10 The most widely accepted hypothesis that explains the pathophysiological mechanisms of damage is a defect in fluid interchange from the blood vessels to the intestinal lumen, resulting in hypoxia and ischaemia of the mucosa.11 Similarly, abnormal colonisation by commensal bacteria, especially clostridia, has been involved as another key factor in pathogenesis.4,9 For this reason, NEC is considered an entity of multifactorial, yet unclear, aetiology.12,13
Various clinical, paraclinical and pathological signs are relevant to its early identification. The purpose of this description of 24 autopsied cases in which the main diagnosis was necrotising enterocolitis at Hospital General de México from 1993 to 2013 is to characterise and thereby facilitate the recognition of such signs.
MethodsA retrospective analysis was performed of autopsy protocols as well as the medical records of 24 patients admitted to Hospital General de México “Dr. Eduardo Liceaga” between 1993 and 2013, all with a final diagnosis of NEC demonstrated through a pathology study during autopsy by at least two reviewers. A standardised format was used to collect data, and each patient was considered a single case and not duplicated in the registry. The variables evaluated were divided into general data such as newborn factors like weight, which was later catalogued as low (less than the 10th percentile), appropriate (between the 10th and 90th percentile) or high (greater than the 90th percentile). Length was classified as short, appropriate or long based on the corresponding percentiles. Survival was also considered using the Apgar, Silverman and Capurro scales. The latter was used to indicate gestational age; infants were classified as preterm (33–36 weeks of gestation) moderate preterm (29–32 weeks of gestation), extremely preterm (less than 28 weeks of gestation),6 full-term (37–41 weeks of gestation) or post-term (>42 weeks of gestation).15,16 Accompanying comorbidities, most notably heart diseases, were also indicated. Some maternal variables, such as age of the mother and prenatal care by a physician, infections during pregnancy, type of birth (normal or difficult) and laboratory variables—blood chemistry, blood biometry, serum electrolytes and blood gases—were also considered. Finally, office studies and autopsy reports for each infant were analysed in detail.
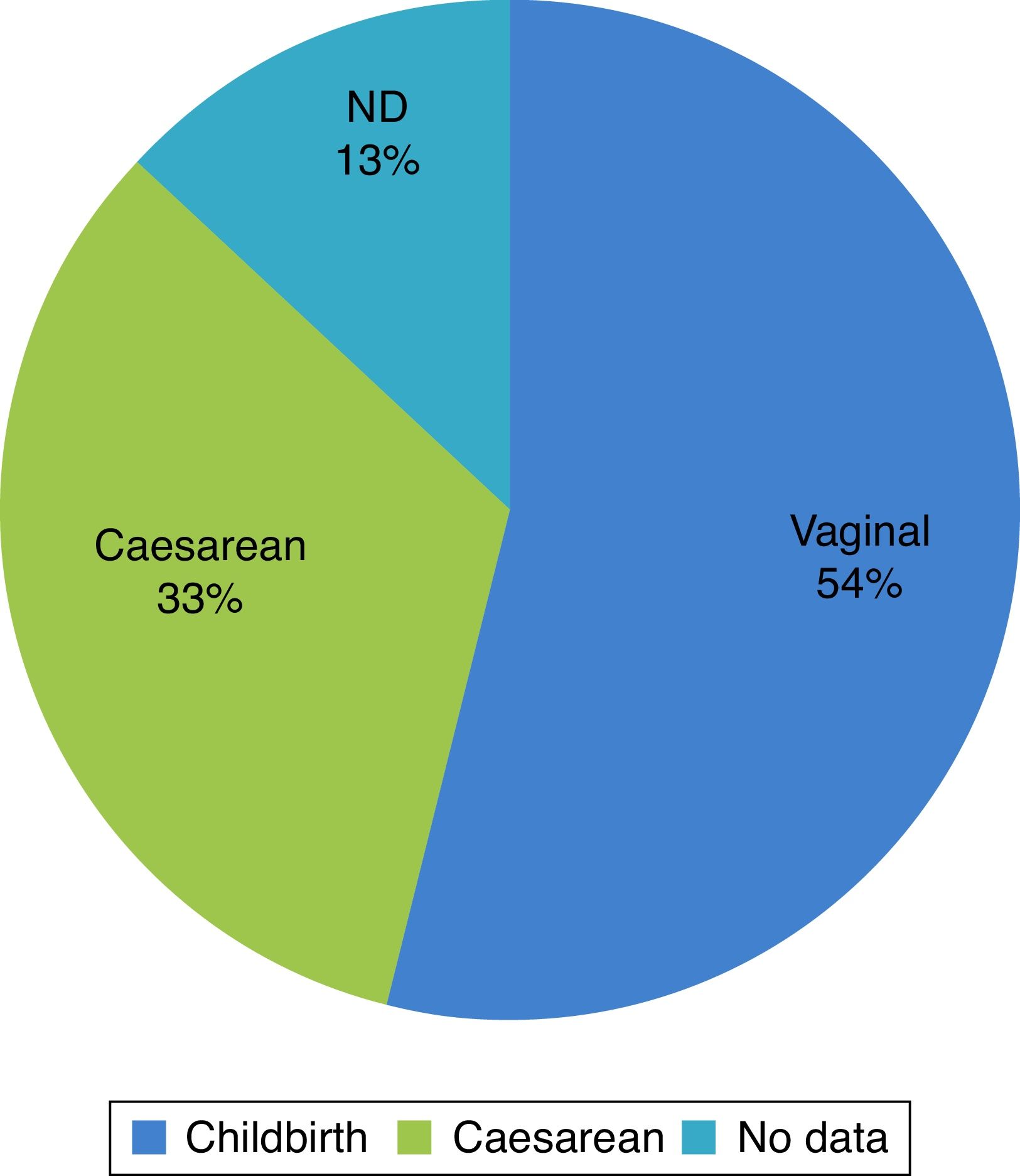
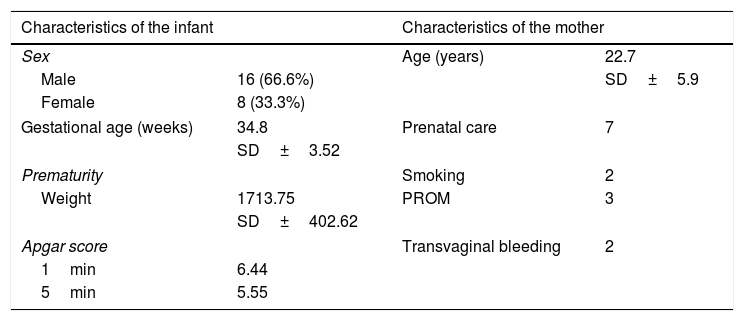
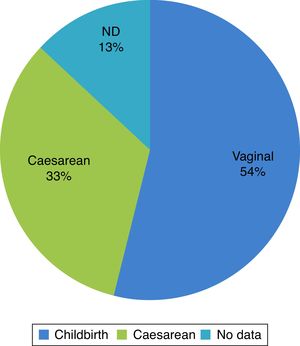
ResultsFor a total of 24 cases, the following results with respect to type of birth were reported: 54% of births were normal (n=13), 33% were Caesarean (n=8) and 13% (n=3) had no report of type of birth on the admission record (Fig. 1). The frequency was higher in males, with 16 cases in males (66.6%) and 8 cases in females (33.3%); 2 patients had some sort of associated genetic defect (Noonan or Down syndrome) and 2 patients had atresia of the gastrointestinal tract (oesophageal or duodenal).
Birth weight ranged from 850g to 2700g (mean weight 1757.75g SD±496.6), and length ranged from 33cm to 50cm (mean 42.8cm±4.9); only 2 cases had no report of birth weight or length. Mean survival was 9.9 days (mean 9.9 SD±8.1). Of the 24 cases studied, 17 (70.8%) were preterm patients, and of these, 6 (35.2%) were moderate preterm, 11 (64.7%) were mild preterm, 6 (25%) were full-term and 1 (4.1%) was post-term. The mean Apgar score was 6.4 at one minute and 5.75 at five minutes. The mean Silverman–Anderson score was 2.4 (SD±1.3). The average age of the mothers was 22 years (x=22 years SD±5 years). In 80% of cases there was some sort of complication in pregnancy; 9 women had a urinary tract infection during pregnancy, 3 women had premature rupture of membranes, 2 had transvaginal bleeding in any trimester. In addition, 2 patients did not get prenatal care and continued smoking during pregnancy (Table 1).
Demographic characteristics of patients with NEC and their mothers.
| Characteristics of the infant | Characteristics of the mother | ||
|---|---|---|---|
| Sex | Age (years) | 22.7 | |
| Male | 16 (66.6%) | SD±5.9 | |
| Female | 8 (33.3%) | ||
| Gestational age (weeks) | 34.8 | Prenatal care | 7 |
| SD±3.52 | |||
| Prematurity | Smoking | 2 | |
| Weight | 1713.75 | PROM | 3 |
| SD±402.62 | |||
| Apgar score | Transvaginal bleeding | 2 | |
| 1min | 6.44 | ||
| 5min | 5.55 | ||
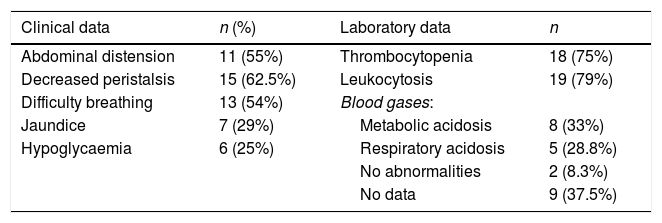
Concerning clinical diagnoses, 66.6% (n=16) were diagnosed with sepsis. Other clinical diagnoses reported were perforation of the gastrointestinal tract 25% (n=6) and disseminated intravascular coagulation (DIC) 12.4% (n=3). The most common signs and symptoms in these patients were abdominal distension, in 55% (n=11); decreased peristalsis, in 62.5% (n=15); periumbilical ecchymosis, in 8.3% (n=2); difficulty breathing, in 54% (n=13); jaundice, in 29% (n=7); and cyanosis, in 15% (n=3). The laboratory data found to be abnormal were as follows: mean haemoglobin was 15.29 (SD±3.03), mean platelets were 155, 75% of patients had thrombocytopenia, mean leukocytes were 30.4 (SD±54.9), 79% (n=19) had leukocytosis at the expense of mean neutrophils being 63.02 (SD±94.10), Na was 135.75 (SD±7.81) and mean glucose was 91.92 (SD±73.55). In addition, 25% of patients (n=6) had hypoglycaemia at some point in their clinical course, mean pH was 7.26 (SD±0.13), 33% (n=8) had metabolic acidosis, 28.8% (n=5) had respiratory acidosis, 8.3% (n=2) had no hydroelectrolytic imbalance and 37.5% (n=9) had no blood gas data recorded (Table 2).
Most common clinical and laboratory data in patients with NEC.
| Clinical data | n (%) | Laboratory data | n |
|---|---|---|---|
| Abdominal distension | 11 (55%) | Thrombocytopenia | 18 (75%) |
| Decreased peristalsis | 15 (62.5%) | Leukocytosis | 19 (79%) |
| Difficulty breathing | 13 (54%) | Blood gases: | |
| Jaundice | 7 (29%) | Metabolic acidosis | 8 (33%) |
| Hypoglycaemia | 6 (25%) | Respiratory acidosis | 5 (28.8%) |
| No abnormalities | 2 (8.3%) | ||
| No data | 9 (37.5%) | ||
Of the cases, 37.5% (n=9) followed a double antibiotic treatment regimen, 16.6% (n=4) were treated with a triple regimen, just one (4.1%) was treated with cefotaxime alone and 41.6% had no record of the medical treatment that they followed.
Radiological findings were reported in only 8 of the 24 cases and correlated clinically and radiologically.
During autopsy, 100% of patients were diagnosed with NEC and 35% of them had perforation of the colon (n=7).
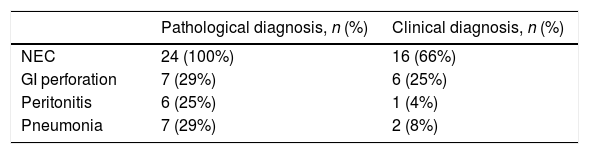
Regarding relevant autopsy data, 5 cases were found to have cranial cavity abnormalities: one case had cerebral oedema, and the other cases had subgaleal, subarachnoid, paraventricular and other paraventricular haemorrhage. In the chest cavity, the main findings were pulmonary oedema and/or bleeding, in 33.3% (n=8). Regarding the abdominal cavity, the most relevant findings are summarised in Fig. 2. The main pathological diagnoses are described and compared to the final clinical diagnoses in Table 3.
DiscussionPremature rupture of membranes and a history of urinary tract infections, which are significant risk factors for developing NEC reported in the literature, are consistent with the findings of this case series. In this study, 45% of pregnant women had a urinary tract infection in pregnancy. This is suggestive of poor prenatal care, which could lead to a greater risk of the neonate having NEC. Of the 24 patients, 17 were preterm (70.8%) (<36 weeks of gestation). This was the main risk factor for enterocolitis reported. The frequency of NEC was greater in male infants (66%) and infants born by vaginal delivery than in those born by Caesarean section (54%), although other articles have pointed to Caesarean birth as a risk factor for NEC. The current literature describes NEC as a disease of multifactorial origin, a phenomenon consistent with the analysis of this series. The mean weight of our patients was 1757g, which is classified as low birth weight; 4 cases had very low birth weight (<1500g), and one case had extremely low birth weight (<1000g). Therefore, birth weight was related to a greater tendency to have this disease in our patients. For preterm patients, mean survival was 20 days, and for full-term infants, mean survival was 10 days. Age was not correlated with survival.
In 2010, Reese reported the results of a study of a total of 211 children throughout Mexico diagnosed with necrotising enterocolitis; 45% were in Bell's stage I, 21% were in stage II and 33% were in stage III.14 This study found that, out of the 8 cases reported, 6 had stage IIA and 1 had stage IIIB.
A significant proportion of NEC survivors with Bell's clinical stage III are known to have the sequela of profound neurodevelopmental delay, which means a decreased quality of life for the patient and his or her family.17 Of the cases in which the Bell's stage was reported in the medical record, the case with stage III was found to have subarachnoid haemorrhage, and the other cases were found to have haemorrhage or intracranial lesions such as hypoxic encephalopathy. Although radiological findings were not reported in all cases, in those in which they were reported according to certified radiologists at this hospital, there was pneumatosis intestinalis (defined as the presence of gas in the bowel wall), which is referred to as nearly pathognomonic of NEC.2 Other findings in our patients were ascites and gas in the portal vein as an indirect indication of perforation.18 Radiologically identified pneumoperitoneum was found in seven cases.9,18 Findings such as free gas, lack of intestinal perfusion, local fluid collection, increased echogenicity of the intestinal wall, gas in the portal vein and pneumatosis intestinalis have been linked to findings with a poor prognosis.19
Clinically, the most common sign among patients was abdominal distension, which occurred in up to 55%. Most patients had leukocytosis; the average figure was 18,00012 (range of 10,000–30,000). Normal platelet count values are 150–400×109/l.28 In this study, the mean was 155,198. Although most newborns had a predominance of or a progression to thrombocytopenia, one case was characterised by thrombocytosis. When that case was excluded, the mean was 132, 553, below the lower limit of the range for platelets in a newborn. There were no abnormalities in the haemoglobin levels of any of the patients (mean 15.29 SD 3.03). Regarding blood gas data, the following was observed: average pH of 7.26 (SD 0.13), mean HCO3− of 17.25 and a pH of acidosis, which was identified as metabolic in most cases, which could be linked to necrosis and tissue hypoxia.20–27 These findings were consistent with those described in the literature.20–27 The average SaO2 was 75.48 (SD 22.17), indicating that most of them had hypoxaemia, and 33% of patients had metabolic acidosis.
In a significant percentage of cases of NEC, some of the examinations requested were consistent with bacterial infection, such as leukopenia and/or a left shift in the complete blood count, and where C-reactive protein was available, it was higher than 40mg/dl in most cases.
These laboratory findings, together with the signs and symptoms that occur in practically all neonates with NEC—poor general appearance, lethargy, thermal instability, pallor, poor peripheral perfusion, nutritional intolerance and/or vomiting, abdominal distension, etc.—suggested that these patients effectively had bacterial infection.
The common treatment in these patients was a double antibiotic regimen based on ampicillin and an aminoglycoside in 37.5%; the other patients had a heterogeneous treatment also based on antibiotics.
The autopsy results for these patients described abnormalities in the gastrointestinal tract in 100% of cases, which was defined as an inclusion criteria (necrotising enterocolitis). Ten of these children had perforation in some area of the gastrointestinal tract, and 4 of them had gastric bleeding.
However, it is important to note the inconsistency between the clinical diagnosis and the autopsy findings, since out of 100% of cases of NEC, only 66% were correctly diagnosed.
ConclusionsNEC is a disease with a high mortality rate in preterm patients. This study indicates some significant demographic and clinical characteristics of patients with NEC, such as low birth weight, prematurity and a maternal history of poor prenatal care and urinary tract infections.
Our results demonstrate a certain inconsistency between the clinical diagnosis and the autopsy findings.
The significance of this case series lies in the accurate identification of the clinical and demographic characteristics of patients with necrotising enterocolitis to make a more accurate clinical diagnosis and thus prevent a fatal outcome.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.