An orthodontic case report is presented. The patient was a 12 year old autistic male with class II, augmented overjet, vertical growth and anterior open bite. He also exhibited tongue-thrust habit. A surgical treatment was ideal for this case but because of his neurological problem, it was decided to use an alternative orthodontic treatment. The orthodontic treatment included: Hyrax, high-pull-headgear, double transpalatal bar with acrylic button and elastics. After a three year treatment, class I approximation was obtained, open bite was corrected and vertical growth was controlled. The patient's tonguethrust habit was controlled using a wrap-around retainer with tongue corrector. This retainer was placed on the maxillary arch and on the lower, a lingual bonded retainer was used. The camouflage orthodontic treatment was successful because good behavioral techniques for autism patients were used.
El presente caso clínico corresponde al tratamiento ortodóntico compensatorio de un paciente varón de 12 años con autismo. El paciente mostraba clase II, sobremordida horizontal aumentada, crecimiento vertical y mordida abierta anterior. También presentaba hábito de lengua. Un tratamiento quirúrgico-ortodóntico era ideal para este caso. Sin embargo, dada su condición neurológica se realizó un tratamiento ortodóntico compensatorio. El tratamiento incluyó diversos aparatos, entre ellos: Hyrax, arco extra oral de tracción alta, dobles barras palatinas con botón de acrílico y elásticos. Después de tres años de tratamiento, se consiguió obtener características aproximadas a clase I, cierre de la mordida abierta y control del crecimiento vertical. El hábito de lengua fue controlado mediante una retención con un arco circunferencial con trampa lingual. El tratamiento ortodóntico de camuflaje fue exitoso gracias al adecuado manejo de técnicas de la conducta para el control del paciente autista.
Malocclusions are an anomaly of the masticatory system function. Malocclusions from a dento-skeletal point of view have been classified in sagittal, vertical and transverse, depending on the space levels they involve. In the sagittal plane malocclusions are subclassified in class I, II and III; in the vertical plane, in open bite and deep bite and in the transverse plane in crossbite and telescopic bite. This case corresponds to the clinical treatment of an autistic patient class II division I malocclusion with anterior open bite.1
Class II division 1 malocclusion presents anomalies at skeletal level such as: collapsed maxilla, due to narrowing of the molar and premolar region; an increased Sella-Nasion-point A (SNA) angle or a decreased Sella-Nasion-point B (SNB) angle and an increased Nasion-point A-point B (ANB) angle; a convex soft tissue profile, a closed nasolabial angle, upper airway obstruction, hyperdivergent growth and an increased lower facial third.1–4
Open bite is the localized absence of contact between one or more teeth in the upper arch against one or more teeth of the lower dental arch. Open bite can occur at any age and in any region of the mouth, the anterior region being the most frequent. Open bite is classified into two: the dental open bite, in which only the teeth are affected and the skeletal open bite, in which there is already a deformity in the alveolar bone that is often accompanied by dolichofacial features. The etiology of open bite is multifactorial. Local factors such as habits of persistent sucking, atypical swallowing and oral breathing, as well as general factors such as heredity, birth defects, and muscle disorders promote the open bite.5–13
Treatment for open bite consists of three phases. The first phase or preventive is accomplished through removable or fixed appliances, the second phase or interceptive where high pull headgear may be usedas well as those mentioned above in the preventive treatment, and finally the third phase or corrective where fixed orthodontic appliances, elastics, molar intrusion or even a combined treatment of orthodontics with surgery are used.10–12,14,15
AutismAutism is a disorder that affects social interaction, language, behavior and the cognitive functions of the individual who suffers from it. Since orthodontic treatment time is variable (it can go from one year to several years) and rigorous, a special treatment for patients with autism is needed.16 In addition, collaboration of the parents is essential for orthodontic treatment to be completed favorably. Patients with autism patients are complicated hence behavior management techniques have been developed.13,17,18
Among these, there is systematic desensitization which consists in visually showing the patient every step of the treatment that will be performed on him or her, ask him or her to listen to the sounds of the equipment that will be used and to touch, if possible, all the materials that will be introduced in his/her mouth.18,19
CASE REPORTA 12-year-old male patient attended the Clinic of the Orthodontics Department at the Postgraduate Studies and Research Division of the Faculty of Dentistry of the National University of Mexico. The patient's mother refered that she brought him «to have braces placed on him to align his teeth since they are crooked». The medical clinical history stated that the patient suffered from Asperger syndrome, which is a disorder from the autism spectrum. Additionally, the patient underwent surgery at the age of five years for removal of the adenoids and tonsils. The dental clinic history described only routine treatments.
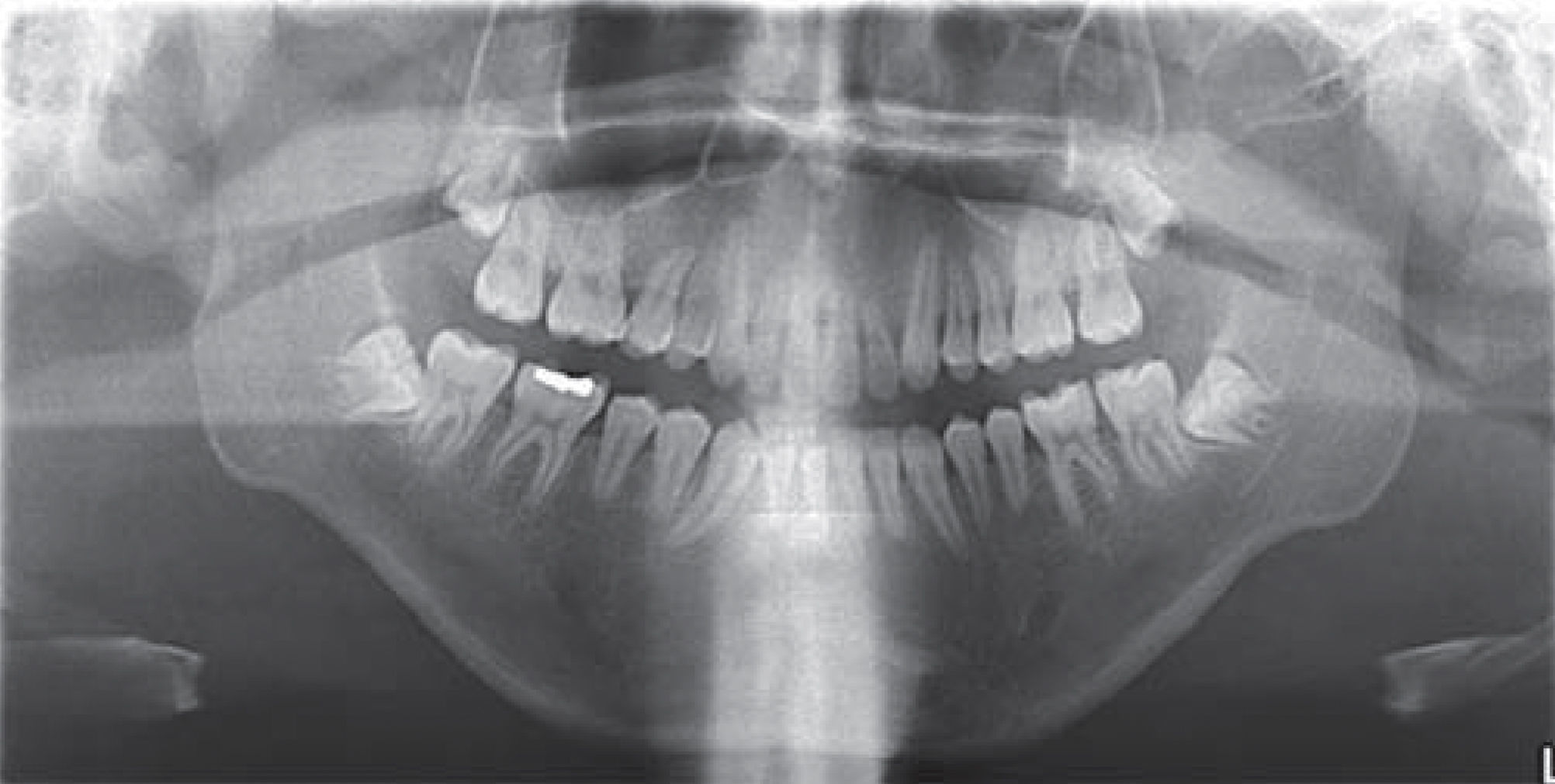
To complete the patient's file, the following studies were prescribed: panoramic X-ray, and lateral headfilm. In addition, study models and extraoral and intraoral photographs were obtained.
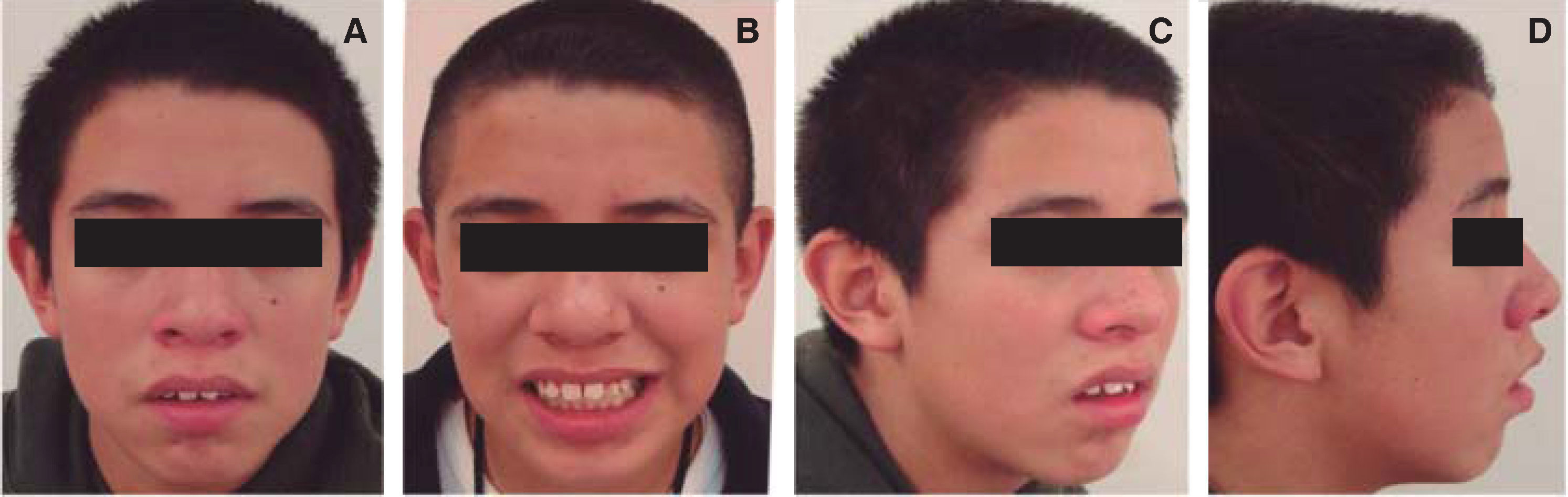
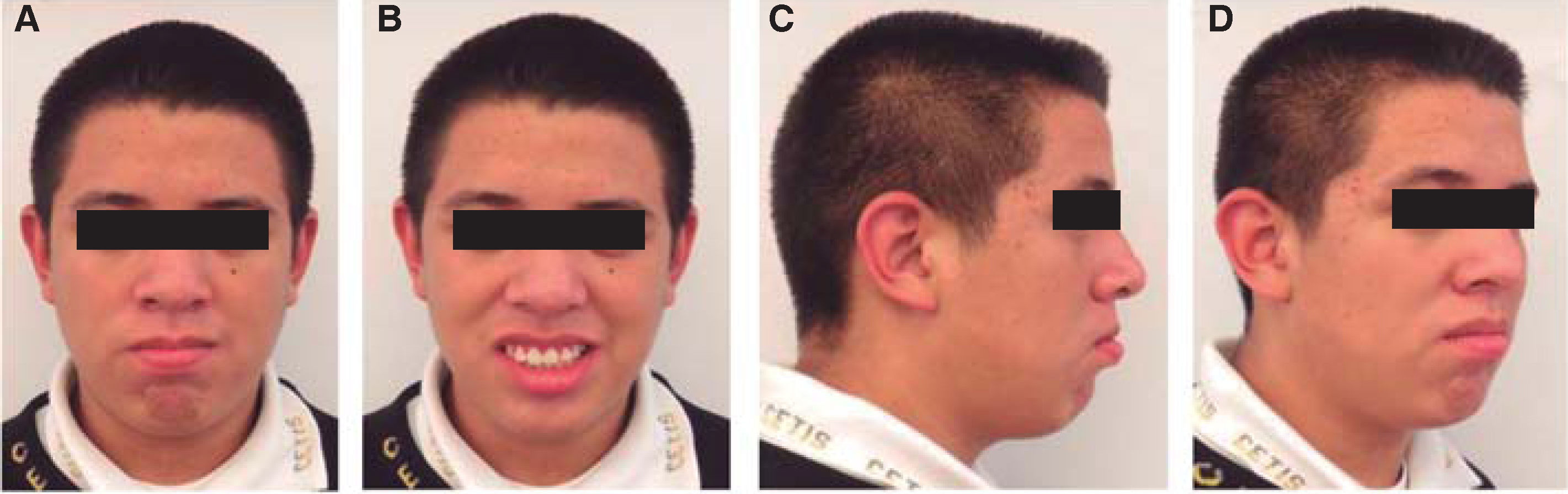
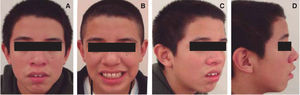
Facial analysis revealed that the patient was dolichofacial with an oval face form and had: convex profile, corresponding facial and dental midlines, chin muscle hypertonicity, thick and incompetent lips, anterior open bite, closed nasolabial angle which compromises profile aesthetics and exposure of 100% of the clinical crowns at smile (Figure 1).
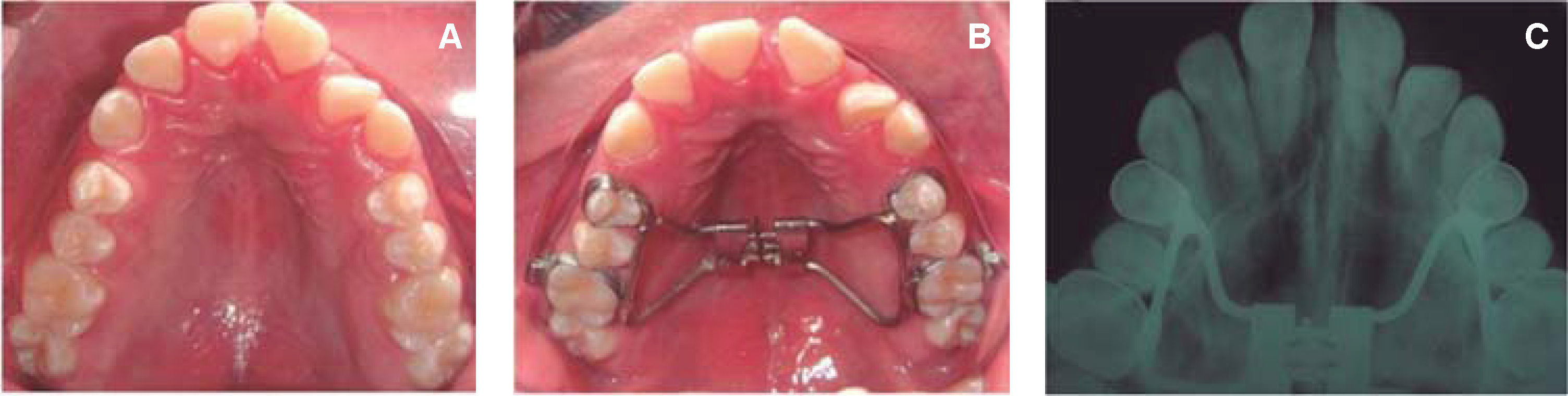
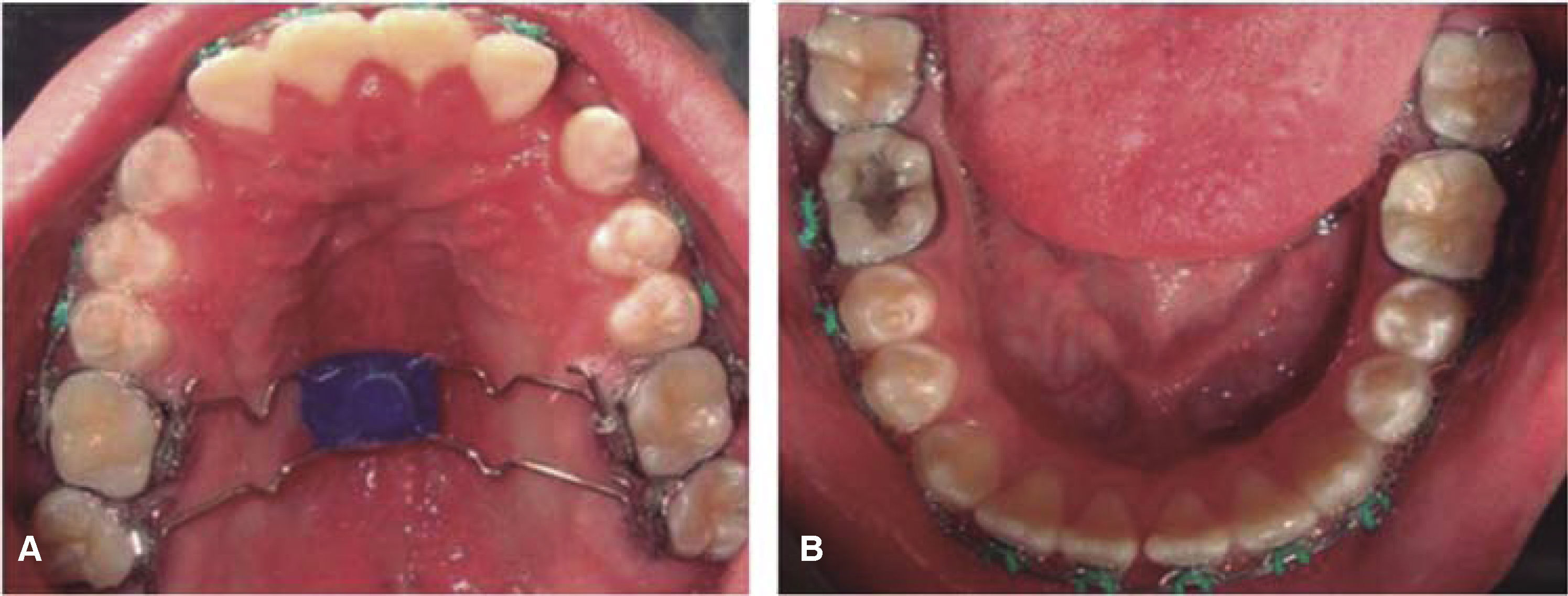
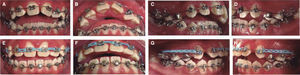
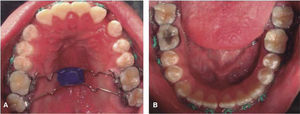
Intraoral clinical examination indicated that the patient had bilateral molar class I, bilateral canine class II, multiple interdental spaces in the upper arch, mild crowding in the lower dental arch, dental rotations, matching upper and lower midline, lack of arch coordination, a triangular-shaped and compressed upper arch, an ellipsoidal lower dental arch, a 10.5mm overjet and -2mm overbite (Figure 2).
The initial panoramic radiograph shows 28 permanent teeth erupted and four third molar germs. The root-crown ratio was 2:1. In addition, there was a lack of root parallelism, condylar asymmetry and short roots of incisors and premolars. The maxillary sinuses, the condyles, the asymmetry of the mandibular ramus, and the premolar roots in apical formation are also shown. No pathology was evident (Figure 3).
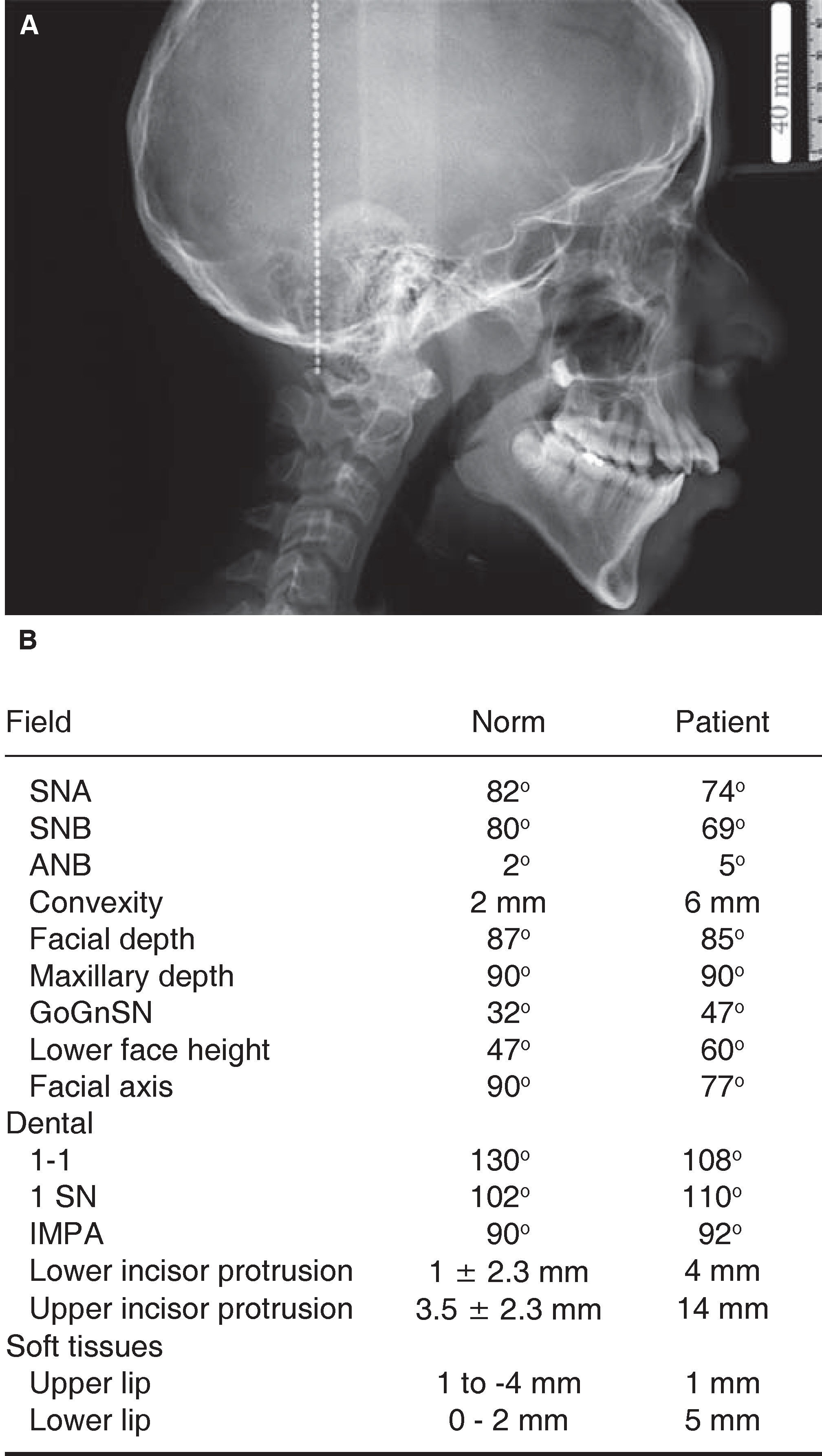
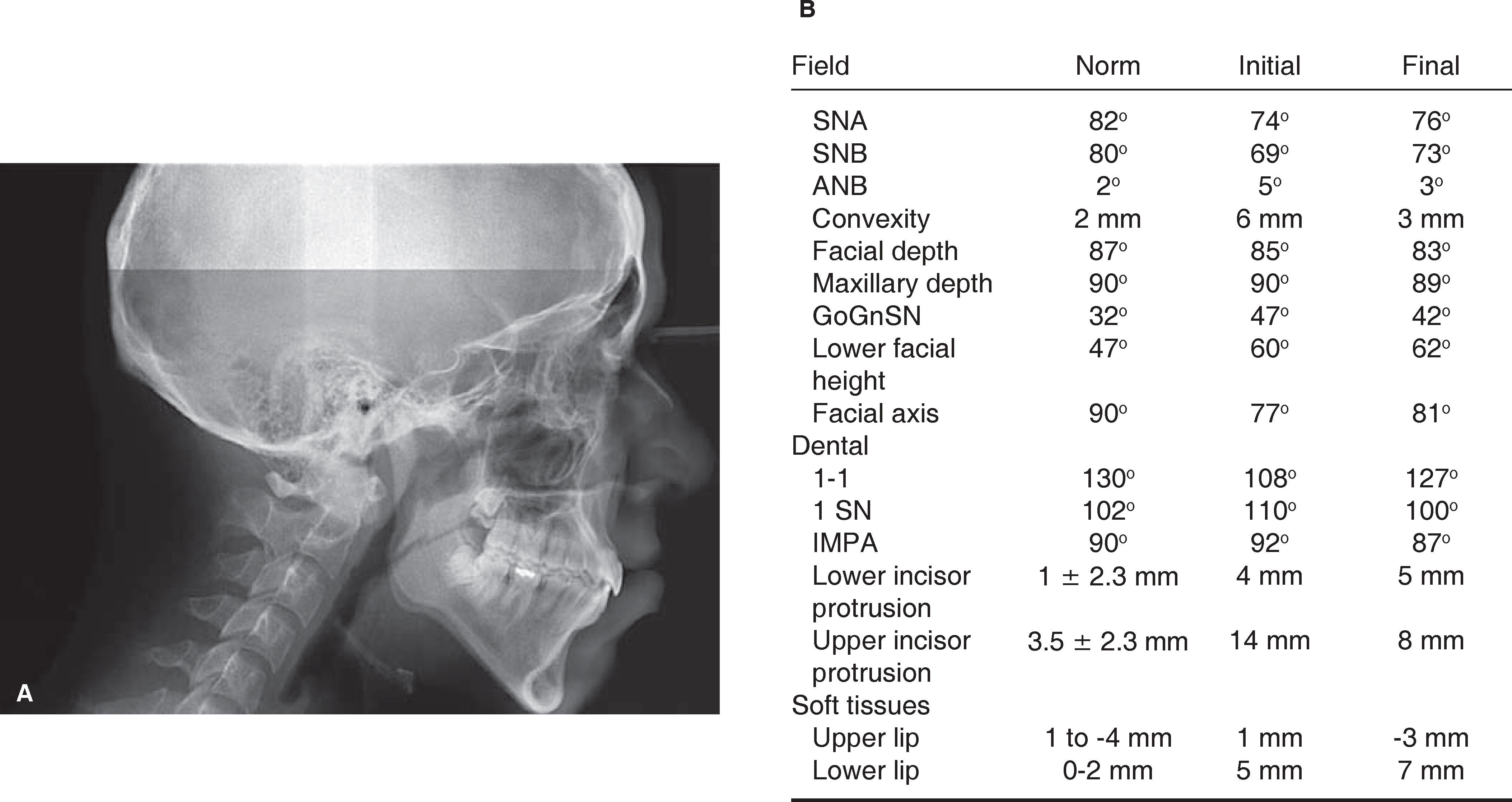
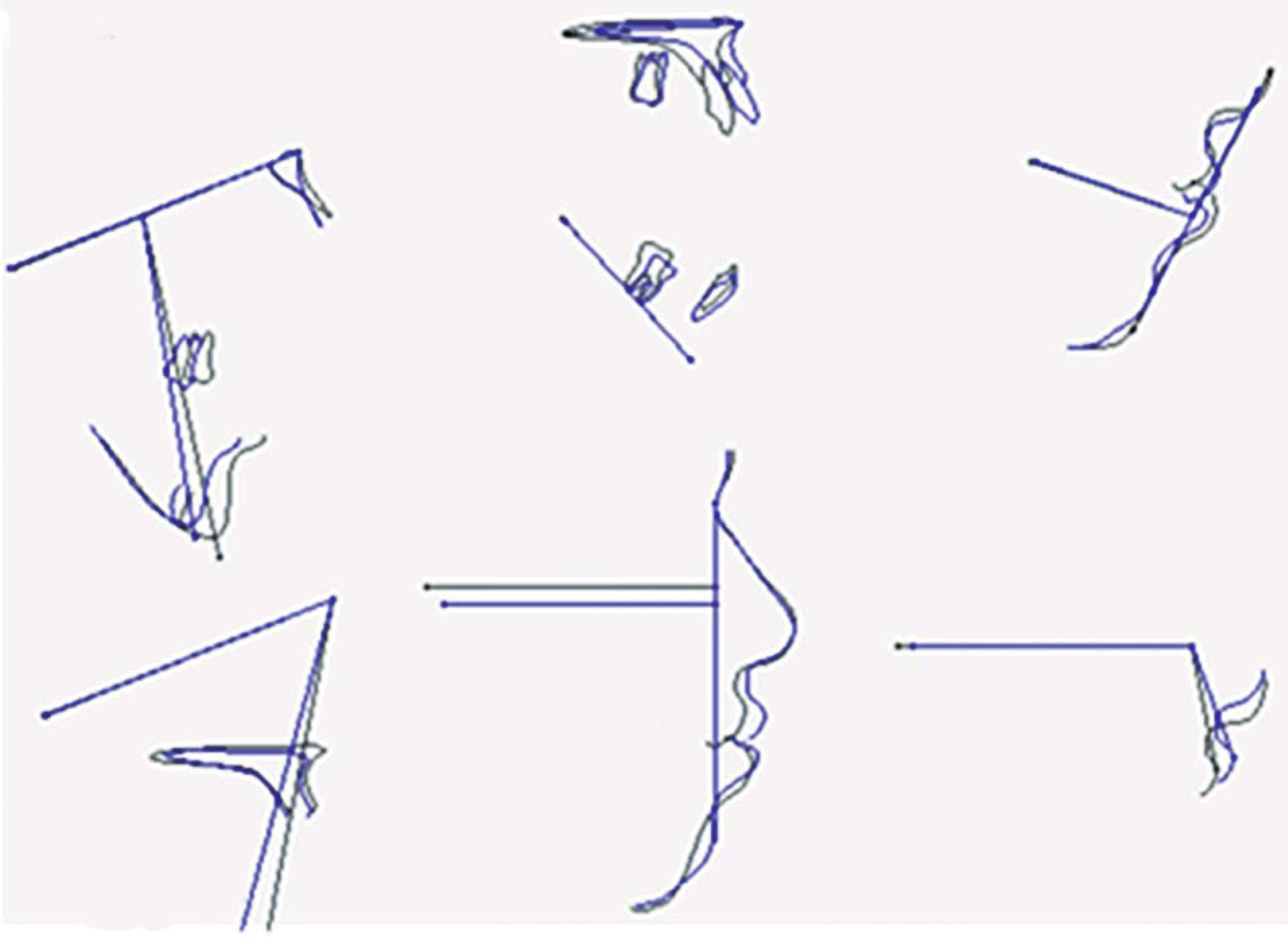
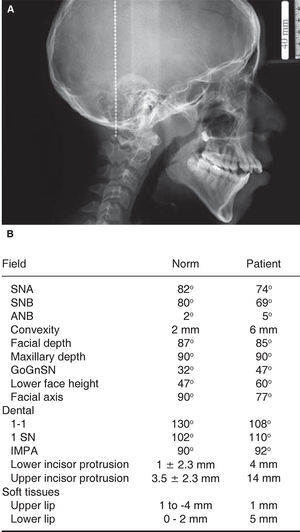
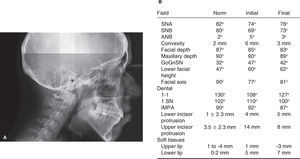
DIAGNOSISThe cephalometric analysis revealed a skeletal class II malocclusion due to the mandible and vertical growth, with anterior open bite (Figure 4A). Cephalometric measurements were high for the mandibular plane, the lower facial height, facial convexity, maxillary height and upper incisor inclination. In contrast, cephalometric measurements were low for the facial axis and interincisal angle (Figure 4B).
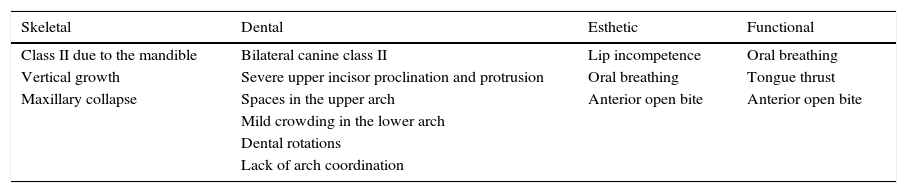
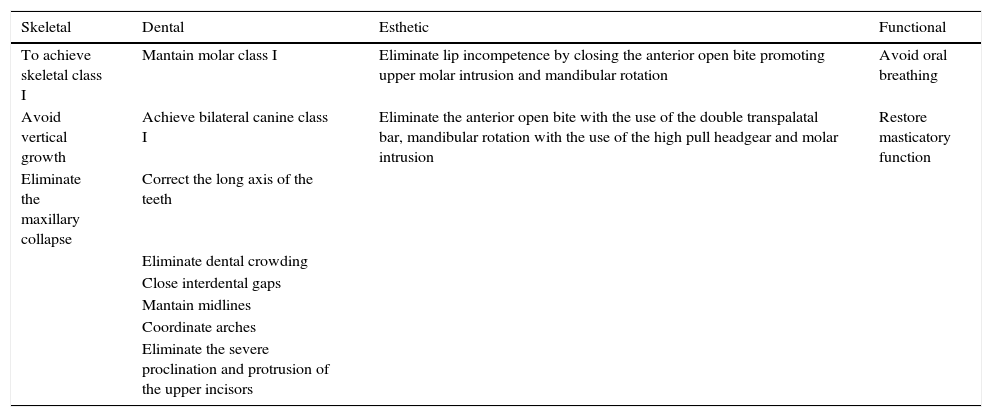
On the basis of the analysis, several problems were found at the skeletal, dental, aesthetic and functional levels (Table I). In order to solve these problems it was decided to correct the patient's malocclusion and recover dento-skeletal function (Table II).
Problems to address.
| Skeletal | Dental | Esthetic | Functional |
|---|---|---|---|
| Class II due to the mandible | Bilateral canine class II | Lip incompetence | Oral breathing |
| Vertical growth | Severe upper incisor proclination and protrusion | Oral breathing | Tongue thrust |
| Maxillary collapse | Spaces in the upper arch | Anterior open bite | Anterior open bite |
| Mild crowding in the lower arch | |||
| Dental rotations | |||
| Lack of arch coordination |
Goals and treatment.
| Skeletal | Dental | Esthetic | Functional |
|---|---|---|---|
| To achieve skeletal class I | Mantain molar class I | Eliminate lip incompetence by closing the anterior open bite promoting upper molar intrusion and mandibular rotation | Avoid oral breathing |
| Avoid vertical growth | Achieve bilateral canine class I | Eliminate the anterior open bite with the use of the double transpalatal bar, mandibular rotation with the use of the high pull headgear and molar intrusion | Restore masticatory function |
| Eliminate the maxillary collapse | Correct the long axis of the teeth | ||
| Eliminate dental crowding | |||
| Close interdental gaps | |||
| Mantain midlines | |||
| Coordinate arches | |||
| Eliminate the severe proclination and protrusion of the upper incisors |
The ideal treatment for this case was orthodontics and orthognathic surgery but due to the autism that the patient presented, it was suggested to the parents to opt for an exclusively orthodontic camouflage treatment.
For the class II correction, a Hyrax appliance was placed to expand the maxilla 5mm thus correcting the maxillary collapse (Figure 5).
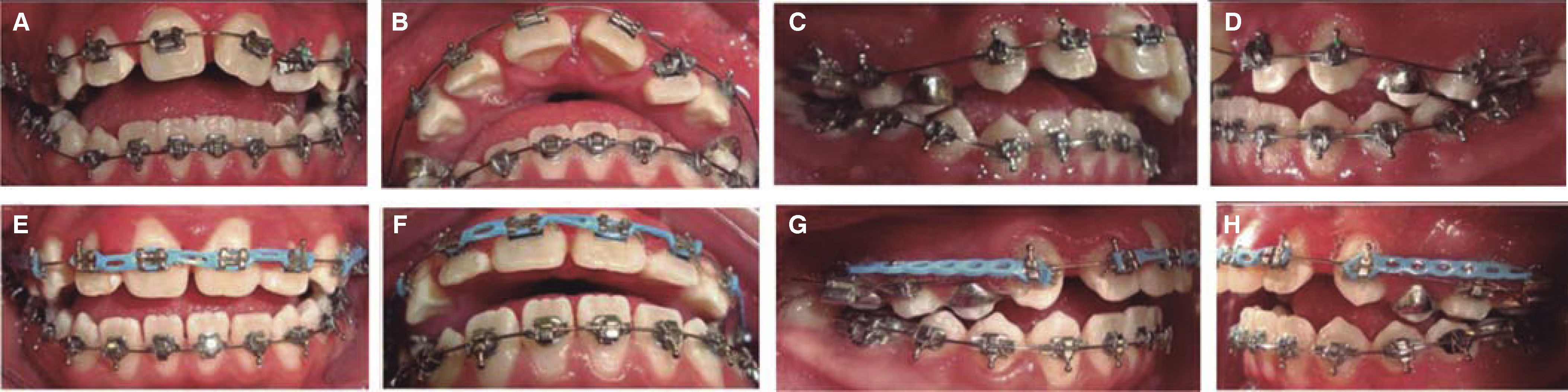
Subsequently, a high-pull headgear was placed with a daily use of 14 to 16hours. The extraoral headgear applied an initial force of height ounces and a maintenance force of 16 ounces for 8 months (Figure 6). After this time period, brackets were placed in the crowns of each tooth.
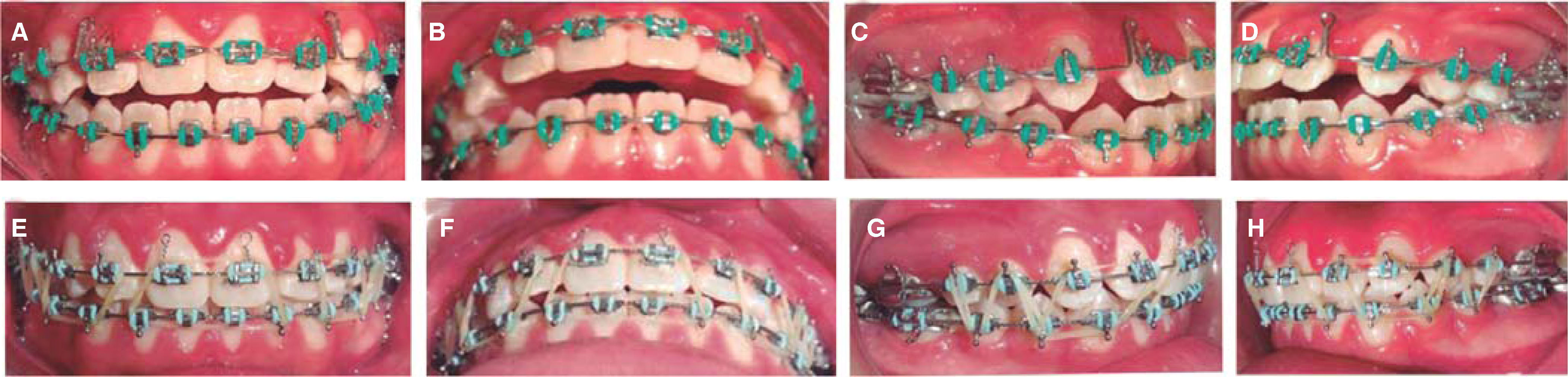
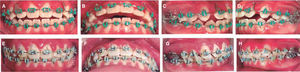
For aligning and leveling, 0.018” Alexander philosophy orthodontic appliances were used with 0.014” NiTi arches (Figures 7A-D). After the initial leveling, which lasted three months, a0.016” stainless steel archwire was placed and a high-pull headgear (Figures 7E-H).
Once the high pull headgear was removed, double palatal bars with an acrylic button were placed for vertical control and molar intrusion and0.016” x 0.022” stainless steel archwires with closing loops in the upper arch (Figure 8). The interdental segments retraction phase was performed with bull loops (Figures 9A-D). For the final phase of treatment, it was necessary the use of settling elastics (Figures 9E-H).
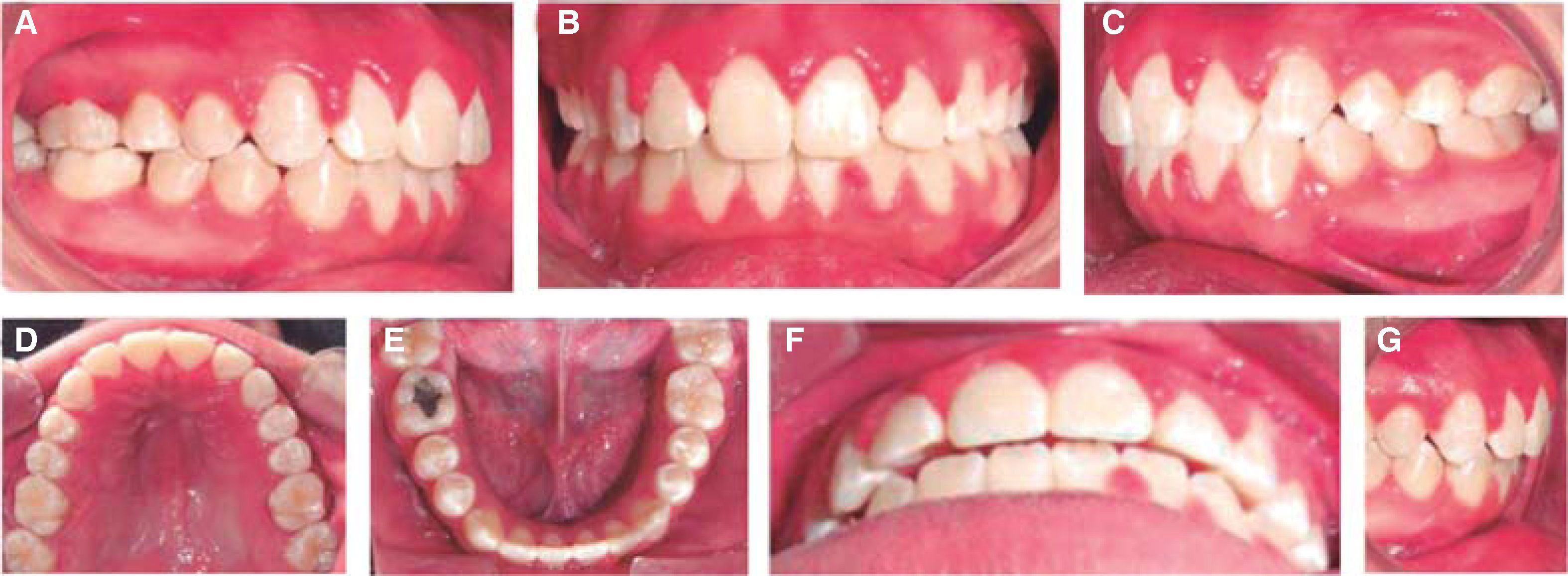
The appliances were removed after 37 months. A circumferential retainer with lingual tramp was placed on the upper arch and a fixed retainer bonded from canine to canine on the lower arch (Figure 10).
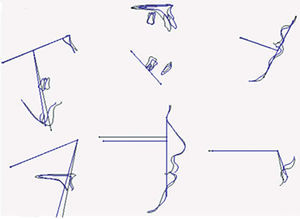
RESULTSSkeletal correction. An approximation to skeletal class I was achieved through retraction of the anterior segment in the maxilla. In the final lateral headfilm the closure of the open bite can be observed and a good overbite and overjet (Figure 11). This observation was verified with cephalometric measurements, where the ANB and convexity angles show values close to skeletal class I, the growth pattern remained vertical but did not increase and so did the lower facial height. The interincisal angle indicates that there was a better relationship between the incisors. It was observed that the upper incisor proclination and protrusion was eliminated.
Vertical growth was controlled by the use of a double palatal bar and the high-pull headgear which did not allow further expression of the normal extrusion movement of the molars thus correcting the class II, closing the open bite and promoting some mandibular rotation in spite of the fact that the vertical growth of the patient continued to be expressed (Figure 12).
Dental correction. The class I molar relationship was maintained, bilateral class I canine was achieved through retraction of the upper anterior segment and the use of class II elastics. Closure of the anterior open bite was achieved, the axial axis of the teeth were corrected, interdental spaces were closed, the midlines were matched and the excessive upper incisor proclination was corrected (Figures 10 and 13). Final parallelism was also noted and the maintenance of the radicular length with which the patient started treatment.
Aesthetic correction. There was better lip competence and the closure of the open bite that the patient presented (Figure 14).
Functional correction. By eliminating the anterior open bite the oral breathing that the patient presented was improved and a better masticatory function was obtained.
At superimposition of the initial and final X-rays: 1. The patient's vertical growth as well as a slight forward and upward rotation of the mandible continued to be expressed. 2. There was a slight forward displacement of point A due to growth remnant. 3. A slight retroclination of the upper incisor was noted; it was also observed that the upper molar maintained its position. 4. There was a slight retroclination of the lower incisor. 5. The upper lip retrusion was observed and that the lower lip maintained its position. 6. There is a lip protrusion that still exists although this is not very reliable because the patient at the time of taking the radiography exhibited hypertonicity of the chin muscles. 7. The retraction of the upper lip was observed (Figure 15).
DISCUSSIONOrthodontic treatmentOne of the greatest difficulties when treating hyperdivergent patients is trying to avoid increasing the mandibular plane. Different methods for treatment of patients with these characteristics have been used but the majority of them (headgear, orthopedic appliances such as the Frankel, ACCO, class II elastics) depend largely on patient's cooperation, Nanda reports that the type of force application has a significant effect on the changes in anterior facial height and posterior facial height.13 In this case in addition to the headgear, a low double palatal bar was used for vertical control of the patient and as it can be seen in the GoGnSN angle, the initial value was 47° and at the end of treatment it was 42°. There was a mandibular rotation which promoted the closure of the open bite, also the extent of the lower facial height that initially was 60° ended up with a final value of 62°. This value, as Spen and Gracco mentioned, indicates us that it was not increased too severely and that it can be considered that there was a good vertical control.15
Kuhn considered eruption control of the posterior teeth as a factor for modifying or maintaining lower facial height.11 The cephalometric data showed that the vertical values of the patient increased: the lower facial third height which started with a value of 60° ended at 63°; the facial axis started with 77° and at the end it was 81°. The reason why the mandibular plane was not expressed in spite of the increase of these values is because of the patient's rotational growth pattern and that the mandible rotated forward.
Autistic patient managementAs mentioned above, patients with autism do not have a good social interaction and exhibit problems with language and behavior. The orthodontic treatment success of this clinical case was due greatly to the implementation of various behavior management strategies. The first thing was to identify the critical points in the patient's behavior. That is, what kind of activities caused anxiety to the patient.17–19 To identify the critical points, we noted that approaching to him quickly, not talking to him and not telling him that he was about to be touched caused anxiety.
Based on these observations the orthodontist learned to approach the patient slowly and accompanied by one of the parents at the beginning. Afterwards, the patient requested to enter alone with the orthodontist. The way to approach the patient was always talking to him and telling him everything that was going to be performed. This strategy enabled us to establish a close link between patient and doctor. Orthodontic treatment was performed by one orthodontist only, restricting socialization.
In addition, instructions were given to the parents to teach the patient skills related to his appointment with the orthodontist. They were told to tell the patient that there would be regular visits to the office and that he should not be afraid. This consolidated the relationship with the orthodontist and enabled the patient to feel safe.
The patient was an oral breather with a tongue thrusting habit. Orthodontic treatment allowed the patient to close his lips, but he had the habit of not doing so. In this case the parents’ help was critical for the patient to re-learn how to close his lips. Finally, it was not possible to remove the tongue-thrusting habit but a system to control it was used.
CONCLUSIONS- •
A good vertical control was achieved through the use of double bars and high-pull headgear.
- •
The mandibular rotation that was favored by vertical control strategies resulted in anterior open bite closure.
- •
Parent cooperation was a key factor in treatment success due to the special characteristics that the patient presented because of the autism he suffers.
- •
The application of behavioral techniques as systematic desensitization has allowed for good cooperation on the part of the patient during their treatment.
- •
The autistic patient management requires knowledge of behavioral techniques and parents’ cooperation.
Orthodontics Specialty student.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia