Osteogenic distraction is used nowadays for tissuelengtheningdue to the bone formation that occurs during the progressive segment separation after corticotomy, being very useful in dentofacial anomalies, especially in severe hypoplasia. We present the case report of a patient with Nager’s syndrome, acrofacial dysostosis of the preaxial type, severe mandibular hypoplasia and oligodonthia who was treated by means of distraction osteogenesiswith ramus osteotomies to lengthen the mandible. He was treated with a Spring Bite-type orthopaedic appliance after the osteotomies. We conclude that treatment with mandibular distraction should be comprehensive and supported with the use of miofuncional advices.
La distracción osteogénica es actualmente utilizada para el elongamiento tisular, gracias a la neoformación ósea que ocurre durante la separación progresiva de los segmentos después de la corticotomia de los mismos. Se ha utilizado con excelentes resultados en anomalías dentofaciales especialmente en hipoplasias mandibulares severas. Reportamos un paciente con síndrome de Nager, disostosis acrofacial del tipo preaxial con hipoplasia mandibular severa y agenesias dentales, quien fue tratado con distracción mandibular a través de corticotomías en ramas mandibulares y posterior manejo ortopédico funcional con aparatología tipo Spring Bite. Con la presentación de este caso podemos sugerir que el manejo de la distracción mandibular debiera ser apoyado con el uso de aparatología miofuncional.
Nager’s syndrome was described for the first time by Nager and De Reynier in 1948; there have been 100 cases reported in the literature up to now.1–3
It belongs to the vast group of otofacialmandibular disostosis such as the Treacher Collins Syndrome, Nager’s Syndrome, Pierre Robin Anomaly, Hemifacial Microsomia, among others. These are malformations associated with a hypoplasia or agenesis of the earlobe and mandibular hypoplasia among other facial deformities which can be found isolated or in association with other malformations.3,4
Nager’s syndrome is a preaxial acrofacial disostosis that consists in facial malformations associated with radial effects (absence of the radial or tibial axisfirst metacarpian and first toe).1–5 It has a recessive autosomal genetic pattern and an alteration of the 9q32 chromosome, 1q12q21 deletion with an average neonatal birth rate of 20%, growth delay of 10% and usually normal intelligence.2–4
With craniofacial characteristics in 25% of the cases, it presents cygomatic and maxillaryhypoplasia, severe mandibular micrognathia, outwards and downwards palpebral fissures, absence of the lower lid eyelashes, lower lid coloboma, broad nasal bridge, depressed tip of the nose, limited mandibular movements secondary to alterations in the mandibular ramus and the temporomandibular joint, macrostomia, cleft lip and palate, soft palate agenesis, short soft palate, high and narrow palate, dysplasic earlobes, atresia of theear meatus, conductive deafness, enamel hypoplasia and oligodonthia. In the muscular skeletal system, it is characterized by radial anomalies, 75% of them being radial hypoplasia or aplasia, sinostosis of the carpal bones, absence of the 5th metacarpian, agenesis of toes and anomalies of pelvic limbs. Cardiovascular anomalies such as Fallot tetralogy and/or ventricular septum defect may be present.1–5 It can also be associated with vesicoureteral reflux or renal agenesis.3
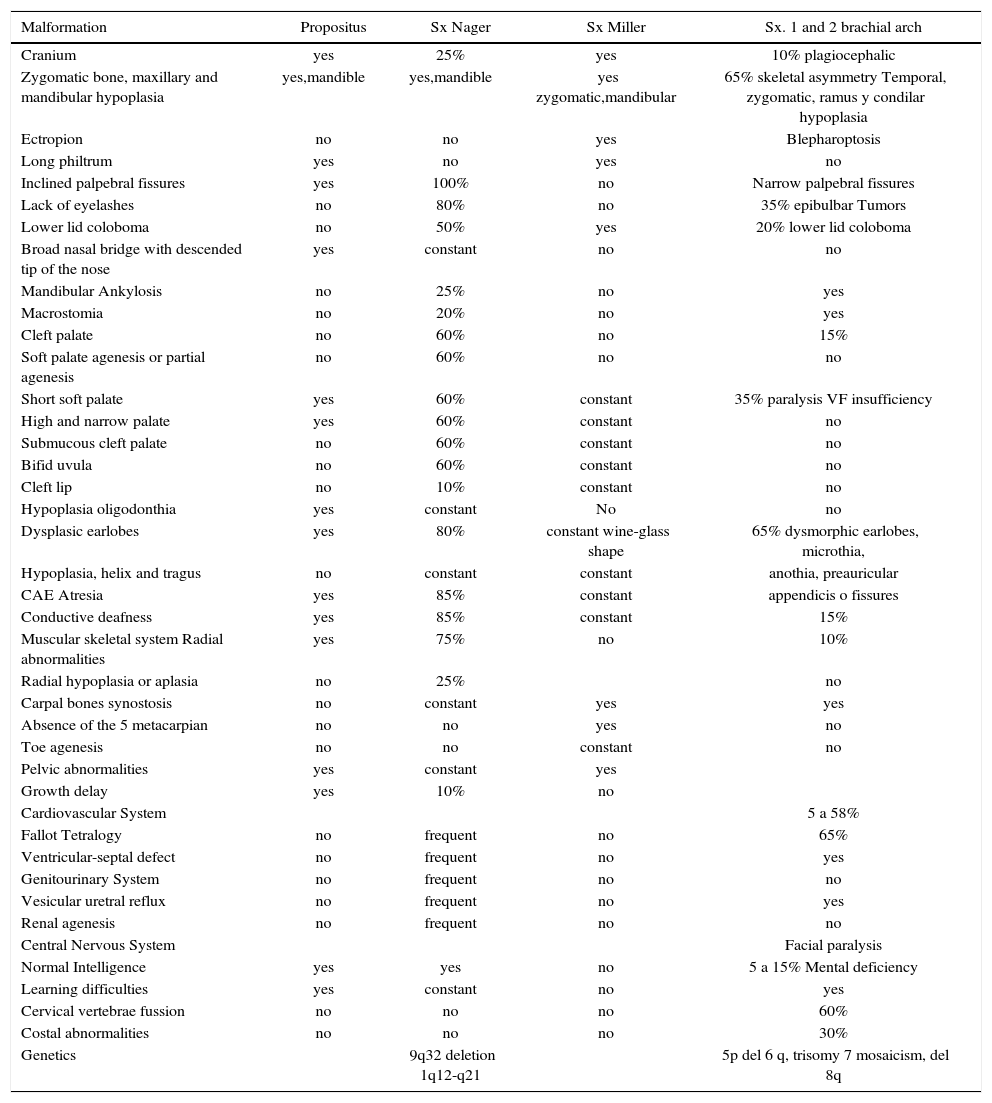
Acral deformities associated with a facial disostosis allow it to be differentiated from the Treacher Collins syndrome, the Nager syndrome and other dysplasiasof the 1st and 2nd facial arch (Table I).3,4
Nager’s syndrome associated malformations compared with others with similar phenotype.
| Malformation | Propositus | Sx Nager | Sx Miller | Sx. 1 and 2 brachial arch |
|---|---|---|---|---|
| Cranium | yes | 25% | yes | 10% plagiocephalic |
| Zygomatic bone, maxillary and mandibular hypoplasia | yes,mandible | yes,mandible | yes zygomatic,mandibular | 65% skeletal asymmetry Temporal, zygomatic, ramus y condilar hypoplasia |
| Ectropion | no | no | yes | Blepharoptosis |
| Long philtrum | yes | no | yes | no |
| Inclined palpebral fissures | yes | 100% | no | Narrow palpebral fissures |
| Lack of eyelashes | no | 80% | no | 35% epibulbar Tumors |
| Lower lid coloboma | no | 50% | yes | 20% lower lid coloboma |
| Broad nasal bridge with descended tip of the nose | yes | constant | no | no |
| Mandibular Ankylosis | no | 25% | no | yes |
| Macrostomia | no | 20% | no | yes |
| Cleft palate | no | 60% | no | 15% |
| Soft palate agenesis or partial agenesis | no | 60% | no | no |
| Short soft palate | yes | 60% | constant | 35% paralysis VF insufficiency |
| High and narrow palate | yes | 60% | constant | no |
| Submucous cleft palate | no | 60% | constant | no |
| Bifid uvula | no | 60% | constant | no |
| Cleft lip | no | 10% | constant | no |
| Hypoplasia oligodonthia | yes | constant | No | no |
| Dysplasic earlobes | yes | 80% | constant wine-glass shape | 65% dysmorphic earlobes, microthia, |
| Hypoplasia, helix and tragus | no | constant | constant | anothia, preauricular |
| CAE Atresia | yes | 85% | constant | appendicis o fissures |
| Conductive deafness | yes | 85% | constant | 15% |
| Muscular skeletal system Radial abnormalities | yes | 75% | no | 10% |
| Radial hypoplasia or aplasia | no | 25% | no | |
| Carpal bones synostosis | no | constant | yes | yes |
| Absence of the 5 metacarpian | no | no | yes | no |
| Toe agenesis | no | no | constant | no |
| Pelvic abnormalities | yes | constant | yes | |
| Growth delay | yes | 10% | no | |
| Cardiovascular System | 5 a 58% | |||
| Fallot Tetralogy | no | frequent | no | 65% |
| Ventricular-septal defect | no | frequent | no | yes |
| Genitourinary System | no | frequent | no | no |
| Vesicular uretral reflux | no | frequent | no | yes |
| Renal agenesis | no | frequent | no | no |
| Central Nervous System | Facial paralysis | |||
| Normal Intelligence | yes | yes | no | 5 a 15% Mental deficiency |
| Learning difficulties | yes | constant | no | yes |
| Cervical vertebrae fussion | no | no | no | 60% |
| Costal abnormalities | no | no | no | 30% |
| Genetics | 9q32 deletion 1q12-q21 | 5p del 6 q, trisomy 7 mosaicism, del 8q |
Osteogenic distraction is a method for bone lengthening that allows the correction of deformities and bone deficiencies with the subsequent correction of the soft tissues6 by means of a distracting appliance.
It was first used by Dr. Codevilla in 1905, when he performed femur osteotomies. This technique remained forgotten for several decades until Dr. Ilizarov in 1950 made it popular in the field of trauma and orthopedics.8,9 Its clinical and systematic application in craniofacial deformities began with McCarthy in 19929–11 mainly by using it in children with hemifacial microsomias for mandibular distraction.11–14Its indications have broadened for the correction of facial asymmetries of diverse etiologies such as severe maxillaryand mandibular retrognathias.9,10
Osteogenic distraction is a biological procedure of new bone formation by applying constant traction forces during a period of time. These forces are applied with a distraction device on a bone area that has been previously weakened by corticotomy.6–8 Thedistraction device is an expansion screw that has been universally graduated in such a way that every 360 degree turn will provide a 0.5mm18,19 movement; all this process is under biological principles such as: vascular preservation, adequatelatency period, distraction rhythm and consolidation period. During this last phase the objective is to keep the bone segment immobile to achieve a correct organization and condensation of the elements that will offer the characteristics of resistance to the newly formed tissue.6,7,18
Physiologically, the process of distraction begins when the loading stimulus is detected by the osteoblast thus triggering a fast and continuous signaling cascade; in this process the bone growth and differentiation is established, the osteoblastic proliferation is followed by cell differentiation and finally by the mineralization of the extracellular matrix; also, specific factors have been identified associated with the beta 1 transforming growth factor (TGFB-1), the insulinic growth factor(IGF-1) and the E2 prostaglandin (PGE2). The created bone gap is initially filled by fibrillar connective tissue with collagen fibers oriented parallel to the force vector of the distraction forces.6–8
Once the tissue neoformation objective has been accomplished, a tissue regeneration phase of this newly formed tissue follows.18,19
The success of the distraction will depend on numerous factors such as: small incisions, preservation of the periostium and vascularity, latency period without distraction of 5 to 7 days, an expansion rhythm of 1mm once a day, a stabilization period or consolidating phase of 8 to 12 weeks and finally, a remodeling period.18
On this last period one can have more certainty on the formation of new bone tissue as well as in the histodistraction; in this stage the distraction appliance may be removed. Equally important is to verify this process by periodical image techniques to monitor the correct function and evolution of the distraction.19–22
Difficulties have been found such as the distractor selection, the determination of the direction of the vector, the site for the osteotomy and patient cooperation.23,24
The orthodontist should be present during the complete process of study and treatment of these patients, playing an important role in the diagnosis, treatment planning and postsurgical management.
The wide variety of mandibular anomalies associated with a syndromic deformity makes it difficult to predict the treatmentresult, in spite of the surgical, orthodontic and physiotherapeutic management. Alsorelapse appears to be inevitable and overcorrection may not compensate central growthalterationsand poor muscular function.Nevertheless, osteogenic distraction has proved to be the most useful method for solving breathing and swallowing problems in patients with severe mandibular hypoplasia asides of improving facial esthetics.9,10
In mandibular retrognathias there is a severe hypoplasia of the mandibular ramus, body and chin so by creating new bone in the posterior part of the mandible (body and ramus) a more anterior positioning of the mandible is obtained,however a moreeffective chin is not always obtained.13,14Once growth has ended the convenience of performing only a mentoplasty or mandibular osteotomies must be reconsidered to achieve the esthetic results.
It is so that osteogenic distraction has quickly become the treatment of choice in craniofacial syndromes with severe mandibular deformities because it is possible to perform during childhood opposite to conventional treatments which may only be performed upon completion of growth; this statement has been controversial due to the fact that multiple studies also report successful results by performing mandibular osteotomies in children.8,19,25
Finally, inaddition to being controversial it is difficult to predict that a mandibular distraction during childhood will definitely substitute an advancement osteotomy in the adult.10,11,13
Mandibular osteotomiesPoswillo and Obwegeser in 1974 stated that surgical trauma in children may alter the mandibular functional matrix and interfere insubsequent facial growth.26,27 However, Converse, Horowitz, Coccaro and Woodsmith in 1973 recommended mandibularsurgery in children pursuing the following objectives:
- 1.
To improve mandibular symmetry by performing bilateral osteotomies in the ramus during the mixed dentition.
- 2.
To provide maxillary growth in response to mandibular growth.
- 3.
To provide an adequate height of the ramus by using an interocclusal splint.
- 4.
By expanding the facial skeleton early,the soft tissues will respond adequately.26,27
In 1941 Converse and Rushton reported the first mandibular osteotomies in children using horizontal osteotomies performed superior to the inferior dental nerve and placing interpositional iliac grafts after the placement of interocclusal splints that increased vertical dimension and thus the augmentation of the mandibular ramus.26
Osborne supported the benefits of mandibular osteotomies performed prior to six years of age. He stated that an early surgery on the mandible provides an opportunity for normal development of the maxilla which is also affected by a hypoplasic mandible.26–28
In 1970 Delaire recommended mandibular surgeries even at an earlier stage, between the ages of 4 to 6 elongating a short ramus with inverted L osteotomies and placing a rib interpositional graft.26–29
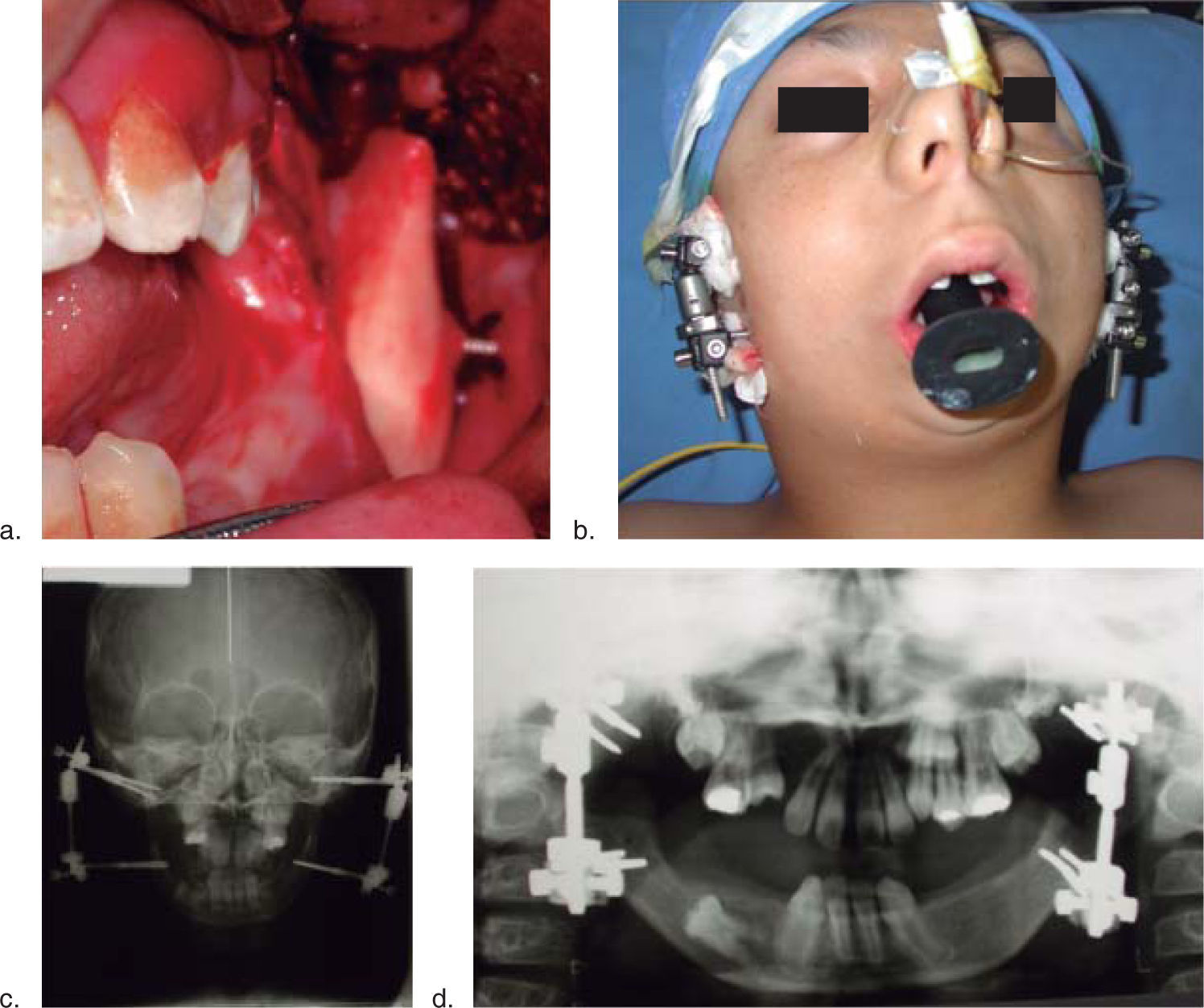
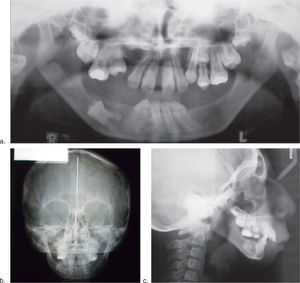
Case reportWe present an eight-year-old male patient diagnosed with acrofacial dysplasia compatible with Nager’s syndrome with characteristic phenotype and the following relevant findings: inclined palpebral fissures, broad nasal bridge, severe mandibular hypoplasia, atresia of the acoustic meatus, conductive deafness, protruded earlobes, oligodonthia, excessively short soft palate, brachydactilia and pes cavus (claw foot) (Figure 1).2,4,5
An interdisciplinary consult with our serviceis performed for the evaluation and management of the severe mandibular hypoplasia and the oral hypometria of 20mm.
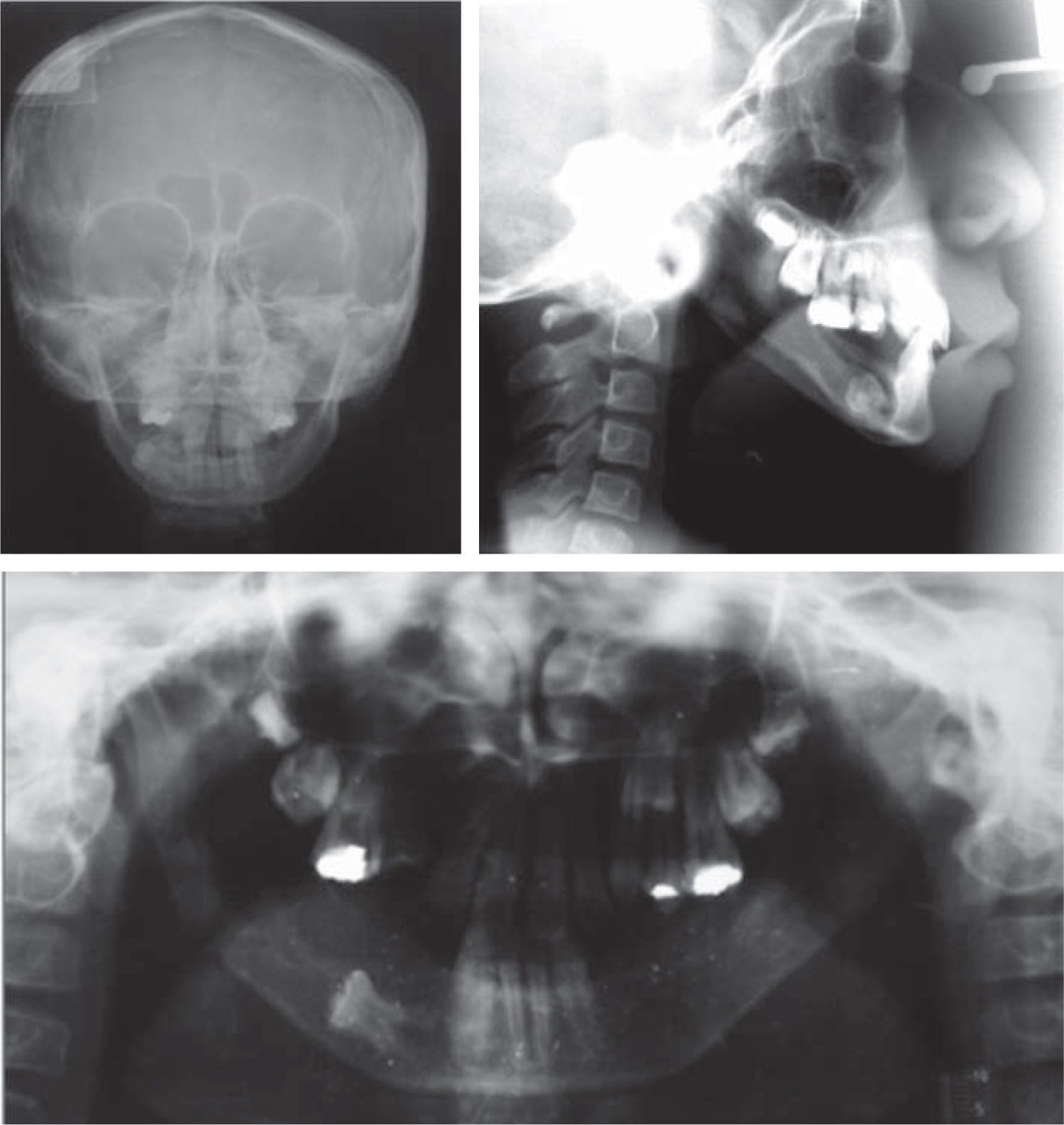
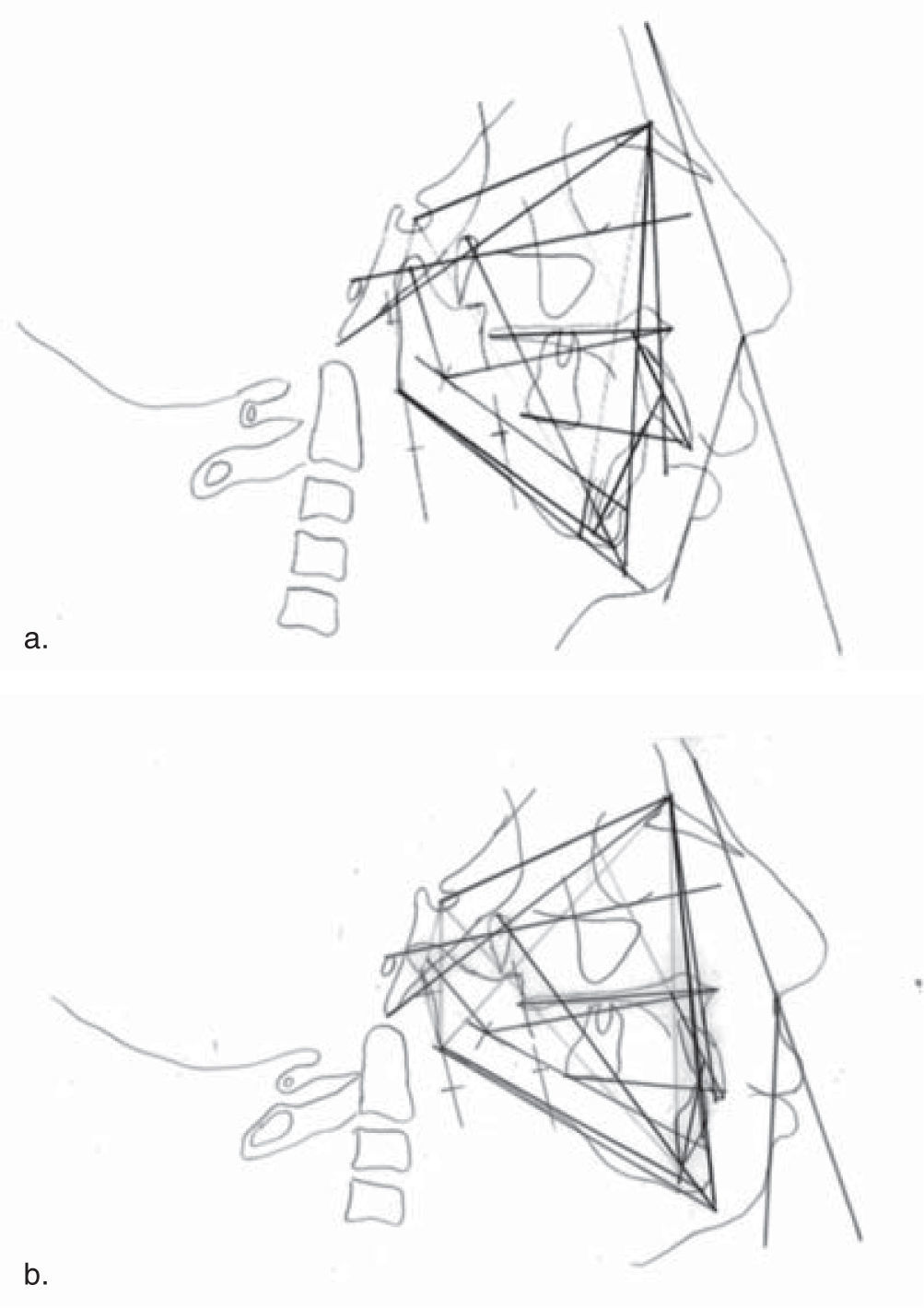
A complete study of the case is performed with a clinical facial esthetic analysis and lateral cefalometry in which a severe mandibular hypoplasia with a delayed growth is evident. Temporomandibular joint pathology is discarded (Figure 2).
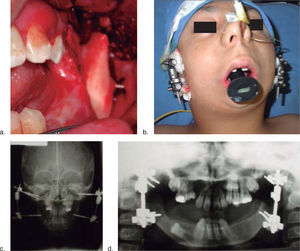
The patient enters a protocol for mandibular osteogenic distraction in which placement of bilateral extraoral mandibular distractors is suggested. A distraction for a total mandibular advancement of 25mm is planned (Figure 3).
Surgical techniqueThe procedure is begun under balanced general anesthesia. The patient presented a difficult airway so the use of nasofibroendoscopy was required for an optimum nasotracheal intubation.
Asepsis of the intervention area was performed and sterile fields were placed.
Throughan intraoral approach, a 2 cm incision was performedin the oblique line region, a mucoperiosteal flap was dissected and ramus corticotomies were marked using an oscillating saw (Stryker Corporation, Kalamazoo, Mich. USA). On both sides of the osteotomy two 2.4×30mm bicortical intraosseous screws (w. Lorenz-Bioment Microfixation HTX-Drive JacksonvilleFL)were placed percutaneously and attached to the external one-way distractor (25mm. Eby fix w. Lorenz-Bioment Microfixation HTX-Drive Jacksonville FL). The same procedure is performed on the other side (Figure 3).
The position of the screws was determined prior to the surgical procedure taking underconsideration the degree of mandibular shortening, the location of the tooth germ and the prediction for mandibular growth (Figure 3b).
The distraction process is begun on the 5th day post-surgery, at a 1mm per day rate for 21 days with a consolidation period of 8 weeks.
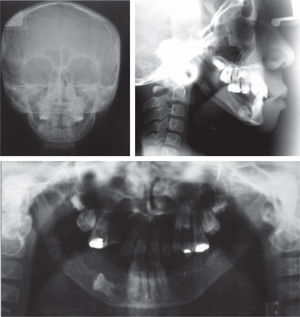
Mandibular growth, occlusion and facial symmetry were assessed and regular radiographic controls were performed as well. Myofunctional therapy was continued due to the oral hypometria an also the management with excursive movements with a spring bite-type appliance (Figures 4and5).
ResultsThe final result was assessed at the endof the distraction period, upon removal of the distractor, 1 year and 2 years after the procedure (Figure 1). Cephalometric tracings were performed and they showed an overall improvement of the mandibular position. An important mandibular advancement was obtained until a 4mm overjet was reached (Figure 5).
A profile improvement was accomplished, obtaining a mandibular advancement of 20mm and a 36mm mouth opening. Due to the use ofmyofunctional appliances astimulus for mandibular growth was evident and an adequatevertical dimension was obtained. By doing so, horizontal growth was accomplished despite the use of a one-way distraction in the ramus and the fact that the patient presented dental agenesias which prevented an adequate interocclusal relationship (Figures 1e and f, 6).
Facial characteristics and interocclusal relationship as well as the anterior guidance were satisfying, contributing to the esthetic improvement of the patient (Figures 1 c, d, f, and6) Table II).
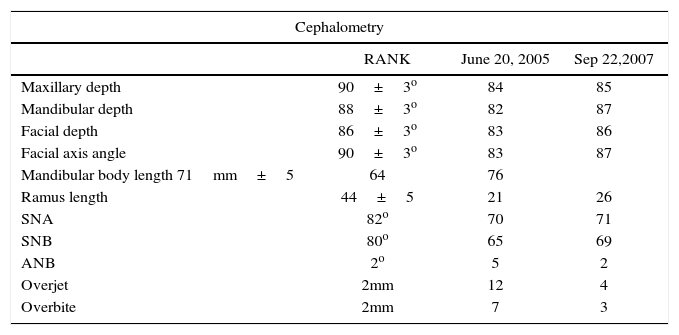
Cephalometric tracing measurements, multiple authors (Rickets, Jarabak, Steiner, Epker).
| Cephalometry | |||
|---|---|---|---|
| RANK | June 20, 2005 | Sep 22,2007 | |
| Maxillary depth | 90±3o | 84 | 85 |
| Mandibular depth | 88±3o | 82 | 87 |
| Facial depth | 86±3o | 83 | 86 |
| Facial axis angle | 90±3o | 83 | 87 |
| Mandibular body length 71mm±5 | 64 | 76 | |
| Ramus length | 44±5 | 21 | 26 |
| SNA | 82o | 70 | 71 |
| SNB | 80o | 65 | 69 |
| ANB | 2o | 5 | 2 |
| Overjet | 2mm | 12 | 4 |
| Overbite | 2mm | 7 | 3 |
The patient remains under growth and development control with the intention of overcorrecting his overjet, stimulating mandibular growth and trying to create more interarch space foreseeing the subsequent rehabilitation by means of endoosseous dental implants thus achieving a normal vertical dimension and restoring masticatory function.
DiscussionMandibular hypoplasia is the most commonly found dentofacial deformity.11,13,14
Severe mandibular deficiency maybe nonsyndromic, an isolated finding or a morphological component of some dentofacial anomaly, in this case specifically, Nager’s syndrome among others.1–5
Functional consequences of severe mandibular hypoplasia includeairway obstruction, obstructive sleep apnea, speech and feeding difficulties and many times, lack of psychosocial adaptation.11,13,14
On the long term, children who are affected by this condition may suffer a delay in growth, cardiopulmonary changes, (pulmonary hypertension and rightcardiac failure) and in some cases, death.9,10
For many years this dentofacial deformity has been treated withosteotomies of the mandibular body and ramus and interpositional graft placement with acceptable results although some authors state that such osteotomies may alter the functional matrix of the mandible.26,17,28,29Additionally, it is known that mandibular advancements of more than 10mm. with sagittal and inverted L osteotomy techniques are unpredictable and their long term stability may be compromised.25,30
Since its introduction, osteogenic distraction hasprovedto possess many advantages for the treatment of severe mandibular hypoplasias, especially when it comes to patients with syndromic-type dysgnathias in whom structural anatomy is altered18,19 and the magnitude of the corrective treatment is far greater. In the same manner, the postsurgical stability favored by distraction, which is not only of the bones but of the soft tissues as well, could be superior to that of osteotomies in some specific cases.9,10
A disadvantage of maxillofacial distraction is its incapacity to achieve precise movements just as the ones achieved with bilateral distractors as well as the management of vectors.23,24
In the case report hereby presented, the following were achieved: increase in mandibular body and ramus length in addition to the soft tissues, all thanks to the use of osteogenic distraction and orthopedic therapy, promoting a counterclockwise rotation of the mandible and thus achieving a better interocclusal relationship.
Nevertheless, using osteogenic distraction as the only method for achieving a functional and harmonic occlusion is still a controversy.15,17
It has also been reported that one of the late complications of osteogenic distractionis the correct management of vectors, with an incidence between 7.2 to 8.8% and even more with the use of a one-way distractor.23,24
In children younger than six years old, osteogenic distraction techniques have been able to achieve very satisfying mandibular advancements that could have been very difficult to accomplish previously.
Osteogenic distraction and conventional osteotomies may be viable options for mandibular advancement depending on the specific case to treat. Therefore, it is necessary to take under consideration other factors such as mandibular morphology, bone quality, the surrounding soft tissue and the developing dentition.9–14,30
Finally, this patient obtained an improvement in oral hypometria due to the increase in the ramus growth and a better positioning of the mandibular body and secondly, the effect on muscular relationships. Still, the effect of myofunctional appliances over muscular relationshipsremains controversial.15–17
In the same manner, mandibular advancement during early childhood does not eliminate the need for orthognatic surgery when the patient has reached its skeletal maturity, thus it is necessary to reevaluate the case once the last peak of growth has ended.9,10,30
ConclusionsAt present there are very well known protocols that describe the process of osteogenic distraction, establishing its latency period, rate,frequency and remodeling period. Still there are no treatment protocols which include the use of myofunctional appliances at an early stage after performing the mandibular distractions.
This type of treatment must be considered in patients with severe mandibular deficiencies, significant oral hypometria, oligodonthia and lack of appropriate interocclusal relationships that would allow an adequate vertical dimension. All of these factors contribute to a more difficult direction of the vector, even more if we are dealing with one-way distractors.23,24
In this specific case, the patient will remain under growth and development control so that once the last peak of growth has concluded we can reassess the mandibular projection and determine the need for mandibularadvancement osteotomies or just a sliding mentoplasty for better chinprojection.Equally importantis the need for an adequate interocclusal relationship so that endoosseous dental implants can be placed.