Class III malocclusion can involve a lot of factors such as excessive mandibular growth, deficient maxillary growth, other environmental factors and maxillary trauma. The correction of this malocclusion can be with orthodontic treatment (camouflage) and when there is a more significant bone discrepancy, esthetic or functional problems; it can be solved with a combination of orthodontic-surgical treatment. In this case report, a 17-year-old patient with a dental and maxillofacial deformity (Angle class III malocclusion) due to a deficient vertical and sagittal maxillary growth, with no transverse discrepancy; excessive mandibular growth, brachyfacial with concave profile, a 1mm incisor display when smiling which had a major impact on the patient’s aesthetic perception of herself. An orthodontic-surgical treatment was planned using Roth 0.018”×0.025” slot appliances. The surgical treatment was a maxillary inferior repositioning and advancement using an autogenous chin graft. Maxillary segmentation was performed to coordinate both arches. Le Fort I surgery is an effective procedure in the correction of dentofacial discrepancies with maxillary deficiency. The aesthetic and functional results obtained by using this type of surgery were successful and treatment was continued with postsurgical-orthodontic treatment to get a detailed finishing of the case.
ConclusionMaxillary repositioning is used nowadays to achieve long term stability in the correction of class III skeletal discrepancies, when in the past the only solution was to treat with mandibular surgery only, thus producing poor facial aesthetics.
La maloclusión clase III puede envolver muchos factores, como crecimiento mandibular excesivo, falta de desarrollo maxilar, factores ambientales y trauma de los maxilares. La corrección de esta maloclusión se llega a realizar con tratamiento de ortodoncia (camuflaje) y en casos donde existe mayor discrepancia ósea, problemas estéticos, funcionales, etc. Se puede tomar la decisión de seguir un plan de tratamiento ortodóncico-quirúrgico. La paciente era una joven de 17 años que se presenta con deformidad dentomaxilar (maloclusión clase III de Angle) debido a deficiencia vertical y sagital del maxilar, no así transversal, así como crecimiento excesivo mandibular, biotipo braquifacial, perfil cóncavo, 1mm de exposición del incisivo a la sonrisa, el cual tenía un impacto estético mayor para la paciente. Se decide un plan de tratamiento ortodóncico-quirúrgico, utilizando aparatología fija con prescripción Roth 0.018”×0.025”.Se definió como plan quirúrgico el avance y descenso maxilar con injerto óseo tomado del mentón y cirugía segmentaria sagital para coordinar arcadas. La cirugía de Le Fort I es un procedimiento efectivo en la corrección de deformidades dentofaciales de origen maxilar corrigiendo la discrepancia esquelética donde fue originada; el procedimiento se realizó con éxito, tanto funcional como estético y se continuó con ortodoncia postquirúrgica para detallar el caso.
ConclusionesLa reposición maxilar es un procedimiento que se lleva a cabo en la actualidad con seguridad y estabilidad, permitiendo solucionar la deformidad dentofacial clase III, logrando mejores resultados que años anteriores, donde todas las deformidades se solucionaban con cirugía mandibular, sacrificando en ocasiones la estética facial.
Surgical-orthodontic treatment emerges from the need to treat patients with dentoalveolar or skeletal discrepancies in whom orthodontic treatment itself will not provide truly satisfying results.1,2 In order to make the decision to perform surgical orthodontic treatment, limits of orthodontic treatment must be taken under careful consideration. These limits vary according to different factors such as a) the dental movement required; Dr. McLaughlin states that the maximum inclinations for a class III patient are 120° for the upper incisor to the palatal plane and 80° for the lower incisor with the mandibular plane as well as 100° for the upper incisor with the palatal plane and 100° for the lower incisor with the mandibular plane for class II patients to obtain an acceptable stability,3 b) limits established by soft tissues, c) function, and d) esthetic and psychosocial considerations.1
Once the decision of carrying out a surgical orthodontic-treatment has been made by the orthodontist and the oral surgeon, the type of surgical procedure to be performed must be decided and whether it will be performed in one or both maxillary bones to obtain the best benefit for the patient. In the case of class III malocclusions, different anomalies might be present such as excessive mandibular growth, lack of maxillary development, environmental factors and trauma.4 The case hereby presented is a surgical-orthodontic correction of a patient with a skeletal class III malocclusion due to maxillary deficiency treated with advancement and inferior positioning of the maxilla and an autogenous graft taken from the chin.
BackgroundIn previous years the only path that orthodontists could take to correct maxillary vertical deficiencies was to extrude the upper teeth thus making a camouflage treatment of the skeletal discrepancy.5 By compensating the skeletal problem with tooth movement or soft tissue treatment, the basic skeletal deficiency is not corrected and frequently the results are not ideal.2,5 When combined with other procedures such as inferior repositioning, intermediate bone grafts and rigid fixation Le Fort I surgery, introduced by Obwegeser in the 60’s,6 provides the orthodontist with the opportunity to attack vertical deficiency problems directly and with a higher success rate.
Although the surgical inferior repositioning of the maxilla has been carried out with success, the degree of stability after the surgery has not been ideal and is frequently unpredictable.5 It has been mentioned before that of the movements performed in the maxilla the inferior repositioning is the least stable.7-9 When trying to explain the relapse mechanism of this procedure, certain parameters are taken into considerations such as: traction of the soft tissues, amount of movement, bone grafts, presence of cleft palate, type of fixation and associated orthodontic treatment.6,7,10 The most recent research shows that the use of rigid fixation reduces the vertical relapse of the maxilla which occurred with wire fixation techniques; the use of bone grafts and osseo integrated implants has contributed to improve the problem of relapse because it increases osteogenesis thus providing a new matrix for new bone formation and increasing the mechanical stability of the surgical site.8,10
According to the research, a relapse of 0 to 100% was reported in cases of maxillary inferior repositioning with wire fixation; therefore, it has been observed that rigid fixation is much more stable.2,5,8,10-13
Thies Hendrik et al suggest a type of osteotomy in the shape of a double M to maintain bone contact after the maxillary inferior repositioning and advancement to reduce relapse.9 Although it is also important to consider that many reports are performed with very diverse and small samples and do not take into consideration the potential effects of orthodontic leveling which can impact long-term stability.11
Case reportA 17-year-old patient comes in to the Orthodontic Clinic of the National University of Mexico with the following chief complaint: «I bite with the lower teeth in front of the upper and I do not like my smile». Her medical records showed that she had asthma in the past but that at present day she did not exhibit any symptoms; she is allergic to penicillin, pollen and tobacco smoke.
Clinical examinationThe patient’s characteristics were as follows:
- a)
Frontal esthetic analysis: The patient has a brachifacial biotype, poor anterior projection of the middle third due to a zygomatic deficiency, flat paranasal areas, deficient lip support, slight facial asymmetry which included a left deviation of the chin and a low left pupil, reduced facial lower third (Figure 1A), negative smile frame with poor exposure of the upper incisors and excessive exposure of the lower incisors (Figure 1B). Perioral muscle tone was normal.
- b)
Profile analysis: She presented a concave profile and a protrusive lower lip but good mento-cervical distance.
- c)
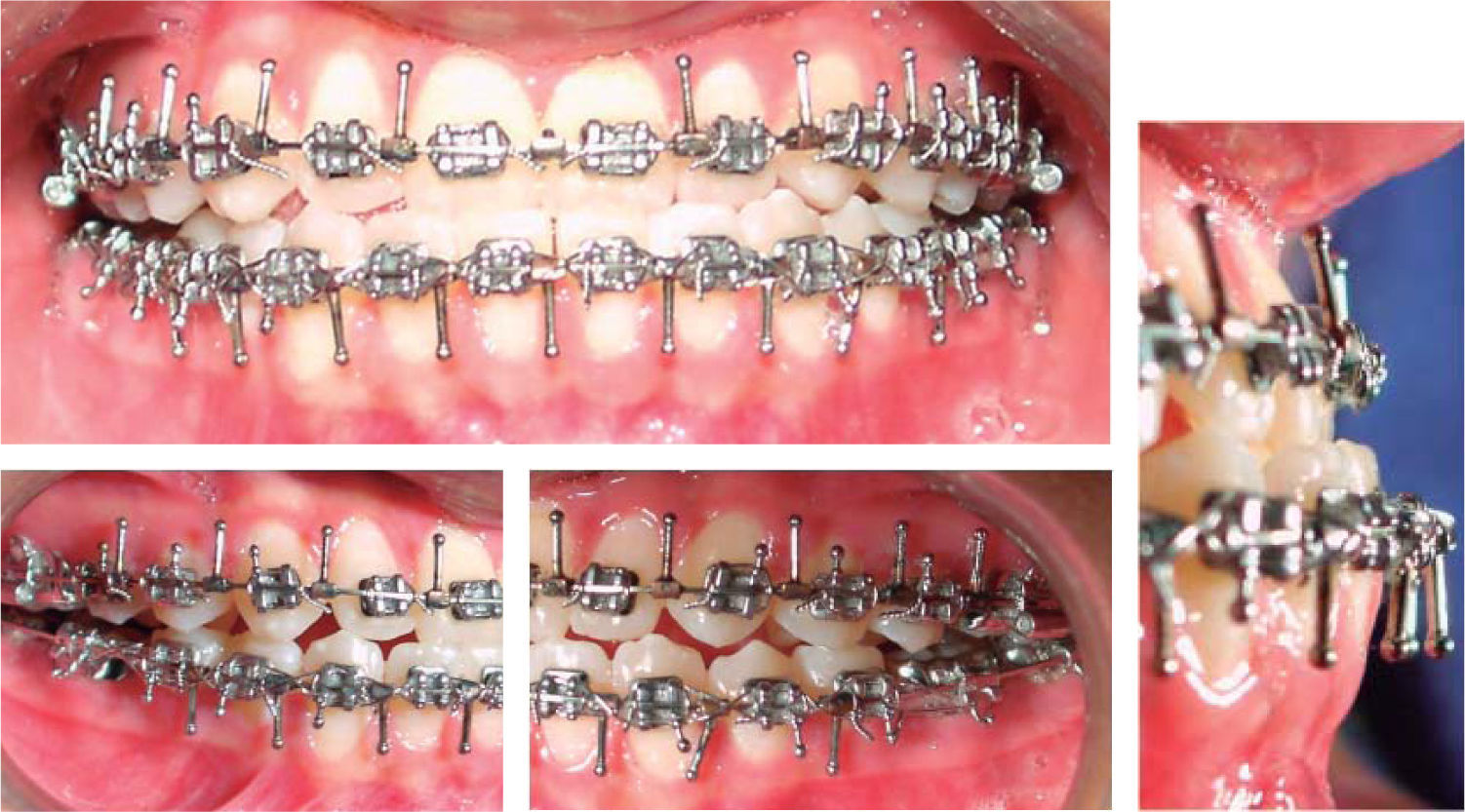
Intraoral characteristics: An anterior crossbite was present and the lower dental midline was deviated to the left corresponding to a chin deviation towards the same side (Figure 2A), right molar and canine class III relationships (Figure 2B); left molar and canine class I (Figure 2C).
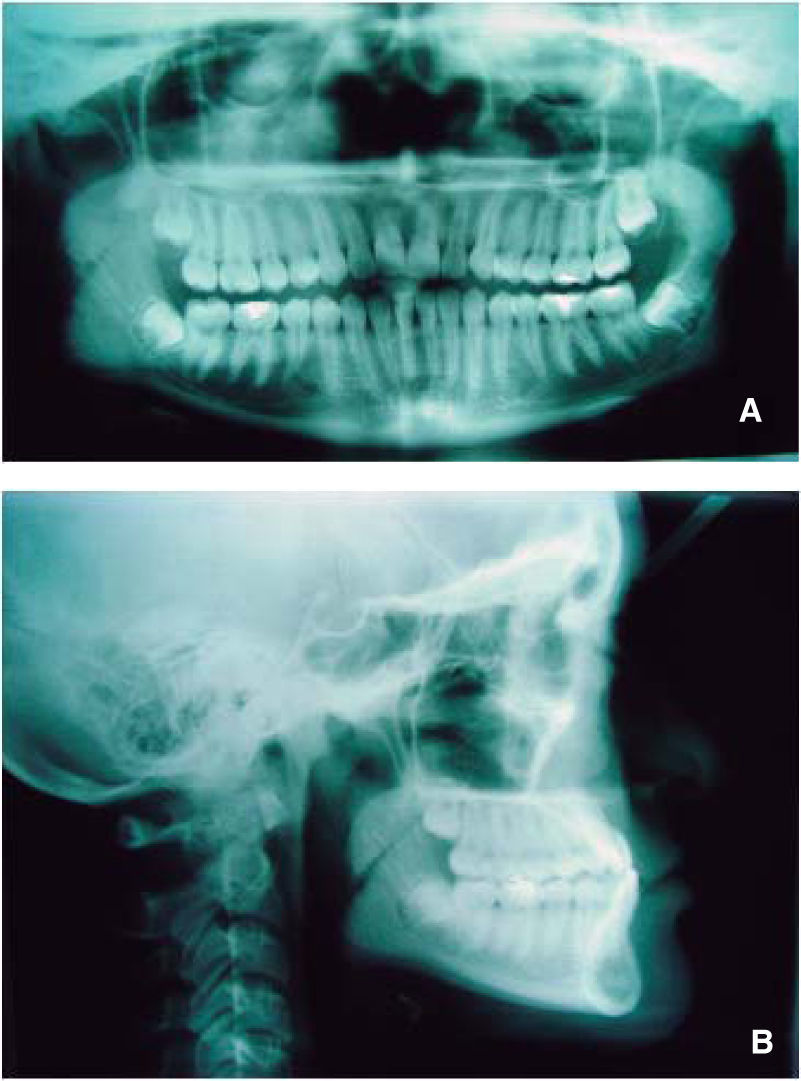
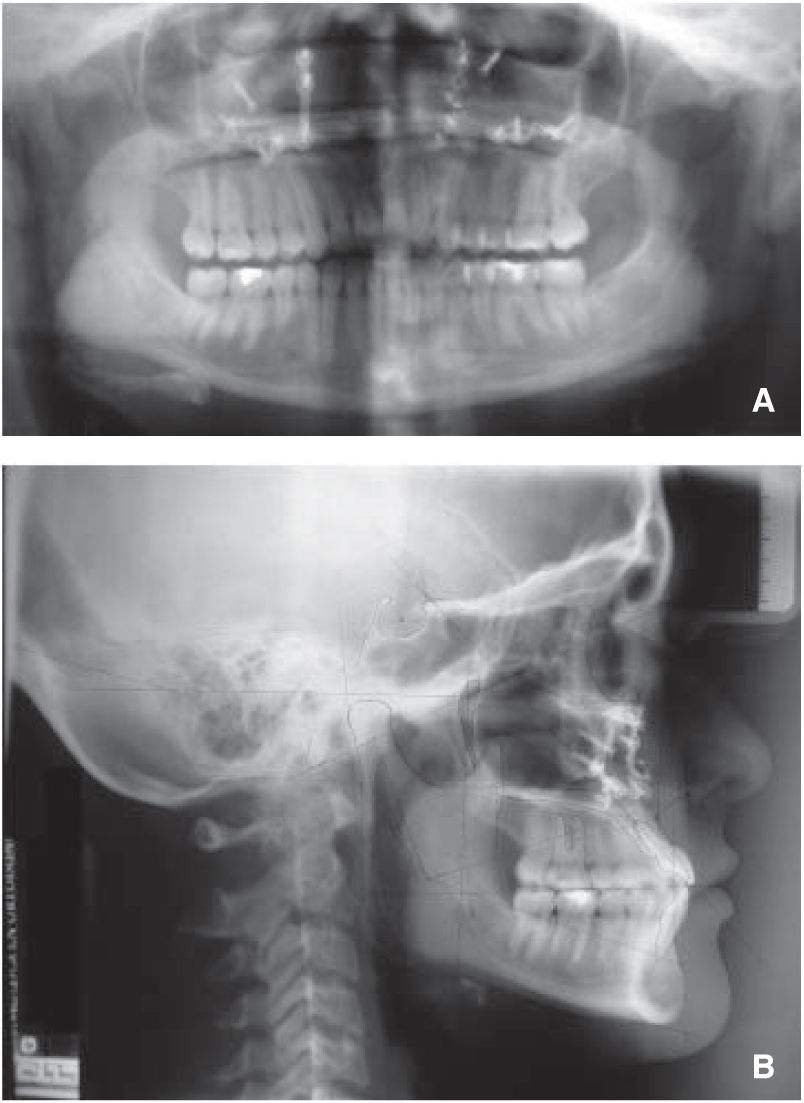
Jarabak’s analysis showed a counter-clockwise growth percentage (77%) as well as an ANB of -8°, a SNA of 84o, SNB of 92° and upper dental proclination (SN/U1: 127o) (Figure 3A y B).
Rickett’s analysis demonstrated the same problem: a convexity of -7mm, a maxillary depth of 92.5° a facial depth of 102°, reduced maxillary height (55°), a palatal plane of 3° and a normal upper lip length (24mm) and a facial axis of 101°.
In the measurements related to growth pattern showed by both analyses a strong tendency to counter-clockwise growth direction is shown and a facial biotype with three standard deviations towards a brachyfacial type which can also be related with the vertical maxillary deficiency suggested by Ricketts analysis (maxillary height of 55°).
Diagnosis and treatment planThe objectives of the treatment plan were to correct or modify the maxillary deficiency (antoposterior and vertical) trying to obtain the greatest amount of esthetic benefits for the patient; to correct the anterior crossbite; to obtain an adequate overjet and overbite, eliminate crowding, achieve a good upper and lower lip position and class I molar and canine on both sides.
It was decided to perform a combined orthodontic-surgical treatment.
- a)
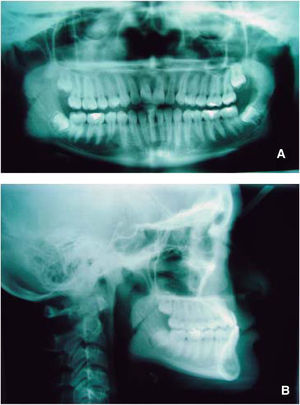
Surgical preparation: A Roth 0.018×0.025 appliance was placed including second molars. On October 9th 2003 we began aligning and leveling with the archwire sequence prescribed in the Roth philosophy. This phase of treatment was completed on March 25th 2004 when 0.016×0.022 surgical archwires were placed (Figure 4).
- b)
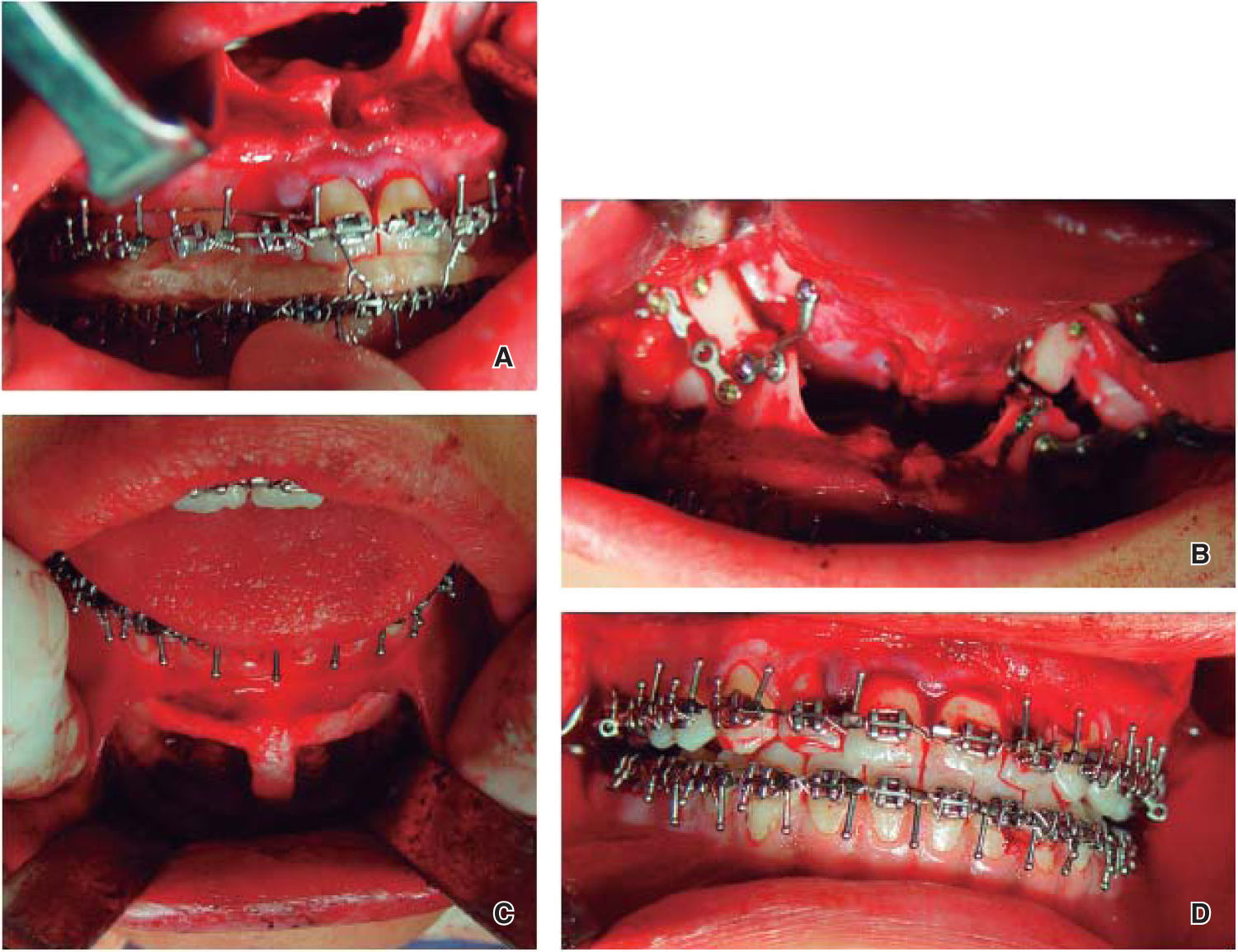
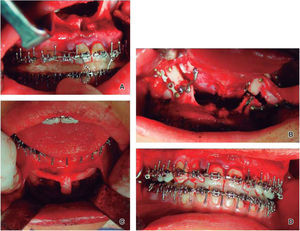
Surgery: A Le Fort I osteotomy with rigid fixation was performed for the advancement and inferior repositioning of the maxilla as well as a segmental osteotomy to collapse the maxilla in the transverse dimension and coordinate arches. The fixation wasrigid with plates and bone grafts taken from the chin in an attempt to reduce relapse as much as possible (Figure 5).
- c)
Postsurgical treatment: On May 7th 2004 postsurgical orthodontic treatment was resumed and root position correction and occlusal settling were performed. On November 25, 2004 fixed appliances were removed and retainers were placed (Figures 6and7).
Treatment objectives were accomplished in a satisfying way by combining orthodontic and surgical therapy. The changes took place in different fields: facial, intraoral and cephalometric.
- a)
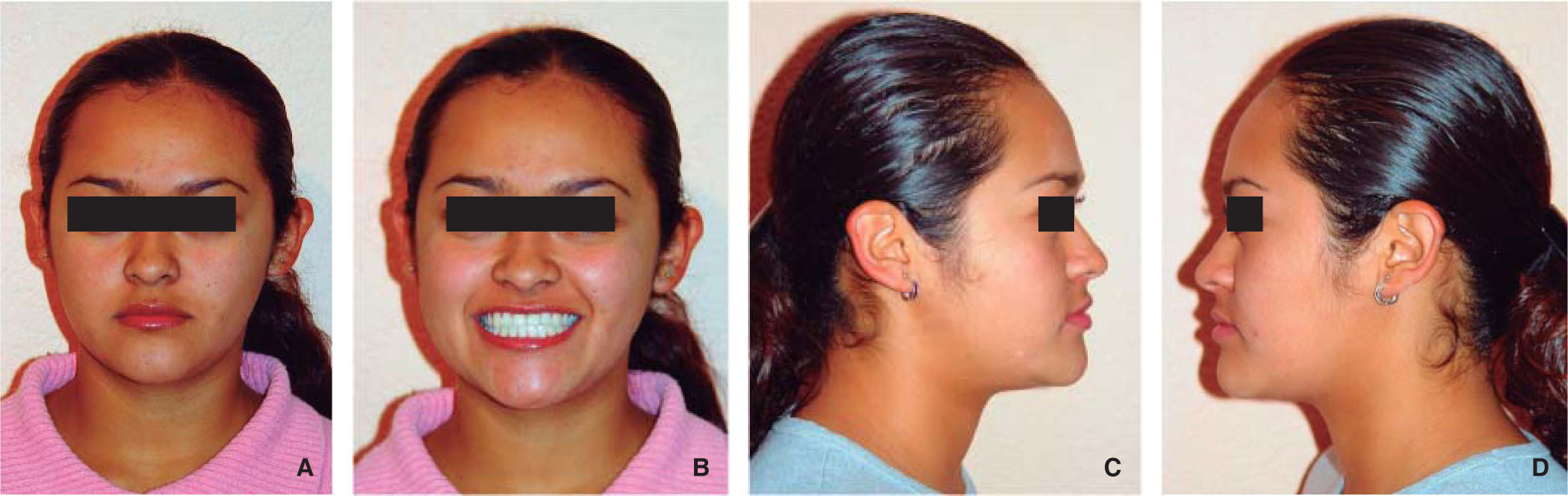
Frontal esthetic result: An adequate anterior projection of the middle third was obtained, with more volume on the zygomatic area, an adequate nasolabial fold, an upper lip with good dentoalveolar support and the correction of the facial asymmetry. On the other hand, correction of the facial thirds was accomplished and a pleasant smile was obtained by a good anterior teeth display (Figures 6a and 6b).
- b)
Profile esthetic results: The patient presents a straight profile, facial harmony and an adequate lip posture, where the lower lip is at the same level as the upper and has well-defined nasolabial and mentolabial folds as well as a good mento-cervical distance (Figures 6c and 6d).
- c)
Intraoral results: Bilateral molar and canine class I, adequate overjet and overbite and centered dental midlines were achieved (Figure 7).
- d)
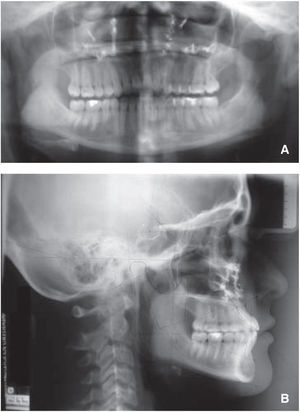
Cephalometric (bone) results: An ANB angle of -3.5° was obtained, a significant correction if we take into consideration the -8° ANB angle that the patient had at the beginning. The growth percentagedecreased from77to a 76% and there were no changes in the inclination of the upper incisor with SN unlike the lower that showed a variation from the initial 89° to a final 94°. Likewise, the interincisal angle was modified to 118° (Figure 8).
On the other hand, in the initial Ricketts analysis the convexity was -7mm and the final as -5mm; the maxillary height was 55° at the beginning and the final was 57°; the palatal plane at start was 3° and upon the end of treatment, -1° and finally, the facial axis began at 101° and ended in 98° (Figure 8).
DiscussionClass III dentofacial deformities due to maxillary deficiencies were long time treated with mandibular surgical procedures or by means of orthodontic camouflage with good but esthetically insufficient results which is why it is suggestedamaxillary approach for the correction of such deformities.
ConclusionsNowadays it is essential to provide a multidisciplinary service to the dental patient since this will give us the satisfaction of performing treatments with better function, esthetics and also reassuring the patient that the received attention will be provided by a professional specialized in a specific area.