The purpose of this study was to compare the resistance when debonding the braces of the enamel after 60 minutes and 24 hours of its fixation with two different adhesive systems. 60 bicuspids where divided into 4 groups of 15 samples each one and were treated with self-etching adhesive SEP Transbond Plus 3M Unitek (group 3 and 4) and conventional adhesive Transbond MIP 3M Unitek (group 1 and 2). The samples were submitted to tangential forces with the universal machine Instron with speed load shedding 1.0mm/min to obtain the resistance when debonding. After doing the statically analysis ANOVA showed that there are not significant statically difference at the debonding forces between Transbond MIP at 24 hours (mean=6.8, SD=2.9) and SEP Transbond at 24 hours (mean=6.1, SD=2.8) (t=0.73 p=0.46). There is no statistically significant difference between Transbond MIP at 60 minutes (mean=6.01 SD=5.2) and SEP Transbond Plus at 60 minutes (mean=7.35, SD=5.1) (t=-.71 p=0.48). It was seen lees than the middle of the remnant adhesive in most of the sample.
El propósito de este estudio es comparar la resistencia al desprendimiento que tienen los brackets del esmalte después de 60 minutos y 24 horas de su fijación con dos sistemas diferentes de adhesión. Se utilizaron 60 premolares divididos en 4 grupos de 15 muestras cada uno, fueron tratados con adhesivo de un solo paso SEP Transbond Plus 3M Unitek (grupos 3 y 4) y adhesivo convencional Transbond MIP 3M Unitek (grupos 1 y 2). Las muestras fueron sometidas a fuerzas tangenciales en la máquina universal Instron con una velocidad de carga de 1.0mm/min para obtener la fuerza de resistencia al desprendimiento. Después de haber realizado el análisis estadístico ANOVA se demostró que no hay diferencias estadísticamente significativas en la fuerza al desprendimiento entre Transbond MIP a 24 horas (media=6.8, DE=2.9) y SEP Transbond Plus a 24 horas (media=6.1, DE=2.8) (t=0.73 p=0.46). No existiendo diferencias estadísticamente significativas en la fuerza al desprendimiento entre Transbond MIP a 60 minutos (media=6.01, DE=5.2) y SEP Transbond Plus a 60 minutos (media=7.35, DE=5.1) (t=-.71 p=0.48). En la mayoría de las muestras se observó menos de la mitad de adhesivo remanente en el esmalte dental al aplicar la prueba de índice de adhesivo remanente (ARI).
The introduction of the etching technique1 for bracket adhesion has come to be an important method in the clinical orthodontic treatment.2,3 The conventional method for bonding brackets to the enamel surface needs three different agents: enamel conditioner, adhesive and composite. Orthophosphoric acid is the most commonly used enamel conditioner. It has been reported that ortophosphoric acid at 30 to 40% concentrations produces the etching patterns with the most retention.4
The introduction of new self-etching adhesives has drawn considerable attention due to the fact that they combine the etching and the adhesive application steps in one thus eliminating the need to rinse and possibly, damage to the gingival tissues. It has also been reported that they minimize the quantity of lost enamel during etching.5 In the beginning self-etching adhesives were used for dentin. Essentially the acid part of the adhesive dissolves the smear layer. It also demineralizes the dentin and captures collagen fibers as well as hydroxyapatite crystals. The adhesive components of the composite then flow into the adhesive- treated dentin which produces a «hybrid layer». The Prompt-L-Pop system was the first sixth-generation adhesive in being introduced to the dental market.6 The same chemical composition was used in the self-etching adhesive (Transbond Plus Self Etching Primer; 3M Unitek, Monrovia, California) for orthodontics. Numerous in vitro studies have been published about the effectiveness of this new self-etching primer.7,8 No differences have been observed between the bracket shear bond strength and the enamel treated with a self-etching primer and the conventional method.7,9–11
The bracket resistance to debonding must be sufficient to endure functional forces to the point that allows bracket debonding without enamel damage. Very high resistance values are not desirable because of the excessive force that it is needed to debond the bracket thus resulting in enamel damage.12 Several studies suggest shear bond strengths of 6 to 10 Mpa as clinically adequate.13The shear bond strengths observed in an in vitro study can be higher than the ones observed clinically. However these studies provide a guide for the selection of the bracket/adhesive.9
Aljuburi14,15 observed a significant reduction in the resistance to fracture with self-etching primers, however, Buyukylmaz et al and Bishara8 reported significantly greater values.
In most of these studies the effectiveness of the self-etching primer Transbond Plus was assessed 24 hours after the bonding procedure.7,9,10 However, this 24 hours period does not reflect the clinical orthodontics in which the archwire is normally placed immediately after bracket bonding, the period of time between bracket bonding and initial archwire insertion varies according to the number of bonded teeth and the clinician’s experience. The initial shear bond strength of the brackets is important because the majority of orthodontists insert the archwire into the bracket slot 10 to 15 minutes after bonding. There are a limited number of studies that focus on the adhesive’s fracture resistance of the self-etching primer Transbond Plus during the first 30 minutes16,17 and another study at 5 and 15 minutes.18
The Transbond XT adhesive system is an example of conventional adhesive systems used inorthodontics. There are different adhesive systems available for bracket bonding in orthodontics. The objective of this study is to compare the bracket’s resistance to debonding after 60 minutes and 24 hours after bonding with two different bonding systems.
MethodsTeethSixty upper and lower right and left premolars were extracted for orthodontic reasons between January and February at the maxillofacial Surgery clinic at the Postgraduate Studies and Research Division of the School of Dentistry. After being extracted, the teeth were stored in refrigeration at 4 °C in bidistilled water which was changed weekly to avoid bacterial growth. The inclusion criteria for teeth selection were: intact buccal enamel, absence of previous treatment with chemical agents (such as hydrogen peroxide), absence of cracks, caries and that they had been extracted maximum three months before use.
BracketsStainless steel premolar brackets (3M Unitek Gemini Metal Brackets .022 (0.56mm) MBT Px, Cuspid hooks, 0 degrees Torque Cuspids 3M Unitek, USA Batch A7432, REF 119-142) were used for this study. The mesh area of the bracket is 10.62mm.
Adhesion procedureThe 60 teeth were divided randomly in 4 groups of 15. Prior to bracket placement, the premolars were cleaned with pumice and a rubber cup for 10 seconds.
The brackets were bonded according to the following protocols:
- •
Protocol I. Groups 1 and 2: (conventional method (CM)) once the teeth were clean, we applied 37% orthophosphoric acid for 15 seconds, rinsing with copious amounts of water. Then the teeth were dried with oil and a water-free air source until a matt appearance was obtained. A uniform layer of adhesive (Transbond MIP; 3M Unitek, USA) was applied to the enamel surface for 2 to 5 seconds. The adhesive resin (Transbond XT Light Cure Adhesive Paste 3M Unitek, USA) was placed on the bracket base and the bracket was positioned over the enamel surface with a positioned (Boone caliber MASEL 4000-900) to align the buccal surface of each tooth parallel to the bracket base. The excess resin was removed with an explorer. The adhesive resin was light-cured for 20 seconds from two directions (mesial and distal) using a LED curing light (Bluephase C5 Ivoclar Vivadent Clinical, USA, ser. No. 1651190, 100-240 V AC, 50-60 Hz) with an output power of 600 mW/cm2.
- •
Protocol II. Groups 3 and 4: A self-etching primer (self-etching primer (SEP) 3M Unitek Transbond Plus Self Etching) was applied to the enamel surface for 3 seconds and was airbrushed. The adhesive resin (Transbond XT Light Cure Adhesive Paste 3M Unitek, USA) was placed over the bracket base and then it was positioned over the enamel surface with a positioner (Boone Caliber MASEL 4000-900) to align the buccal surface of each tooth parallel to the bracket base. The excess resin was removed with an explorer. The resin was light-cured for 20 seconds from two directions (mesial and distal).
Each tooth was mounted on self-curing acrylic resin in a cylindrical block, leaving the sample’s buccal surface exposed. They were mounted placing the tooth with the bracket in the center of the sample maker with help from a 0.016×0.022 wire and an elastomeric ligature tie with the purpose of placing the bracket parallel to the Instron universal testing machine’s wire. The samples were stored in bidistilled water at 37 °C to prevent dehydration.
Bracket debondingThe debonding test was performed after 60 min and 24 h in an Instron universal testing machine set at a crosshead speed of 1.0mm/min, applying the traction force parallel to the longitudinal axis of the tooth until debonding was accomplished. A recording of the values of each sample was obtained in Mpa.
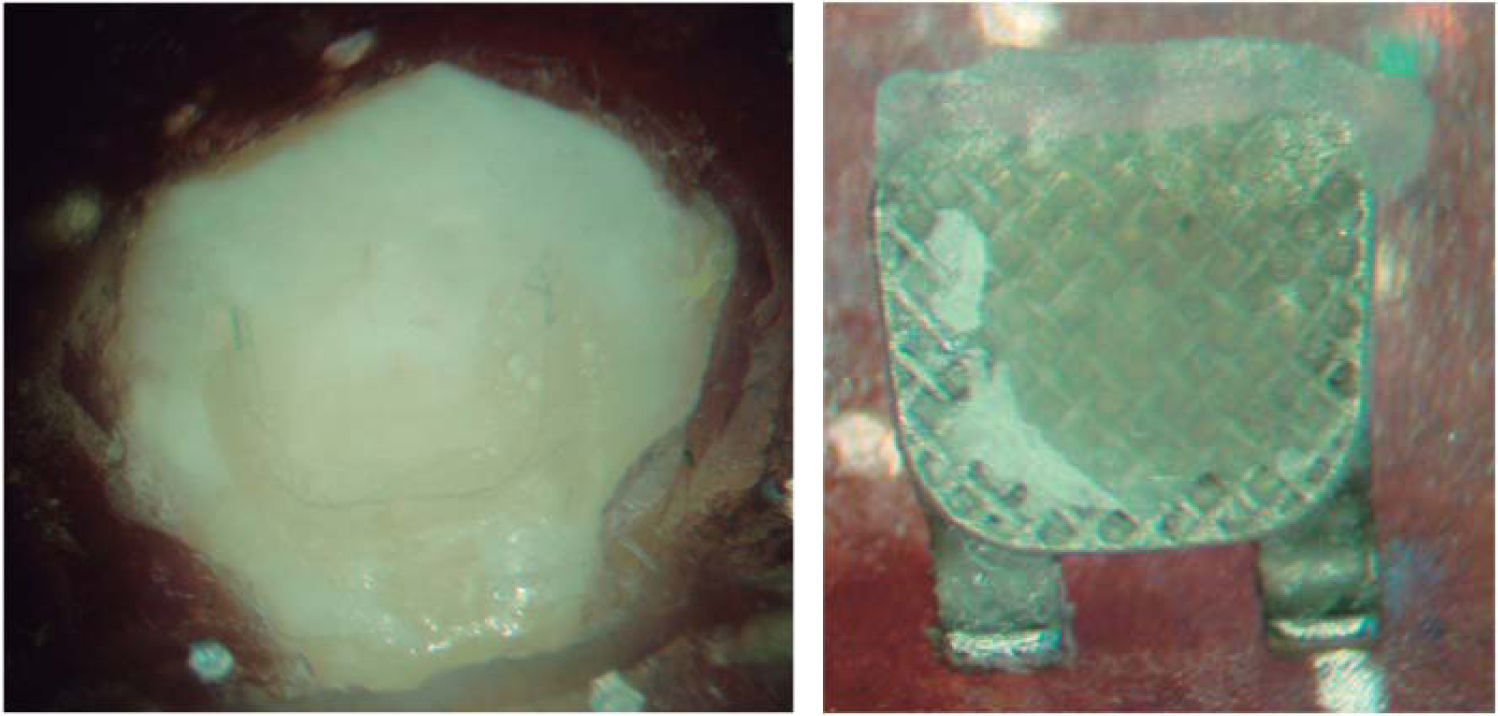
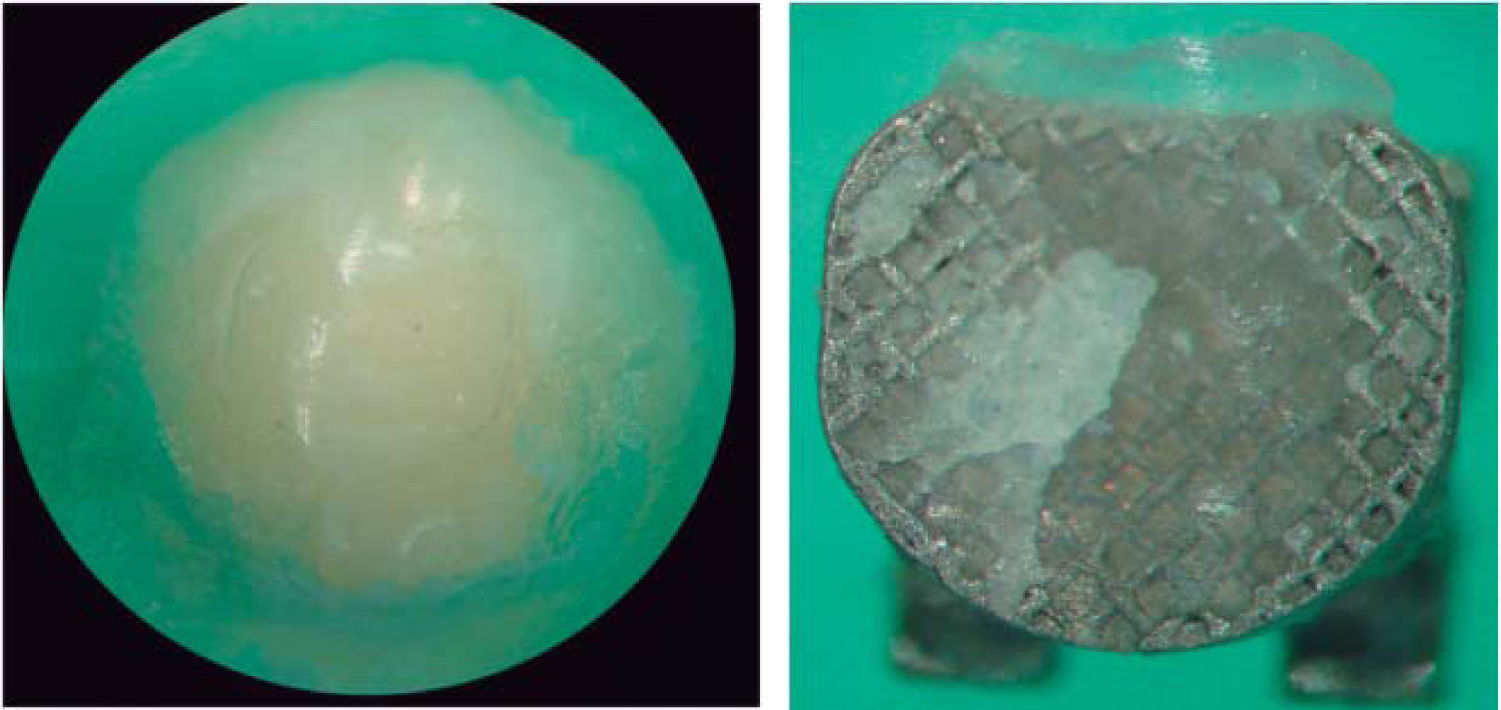
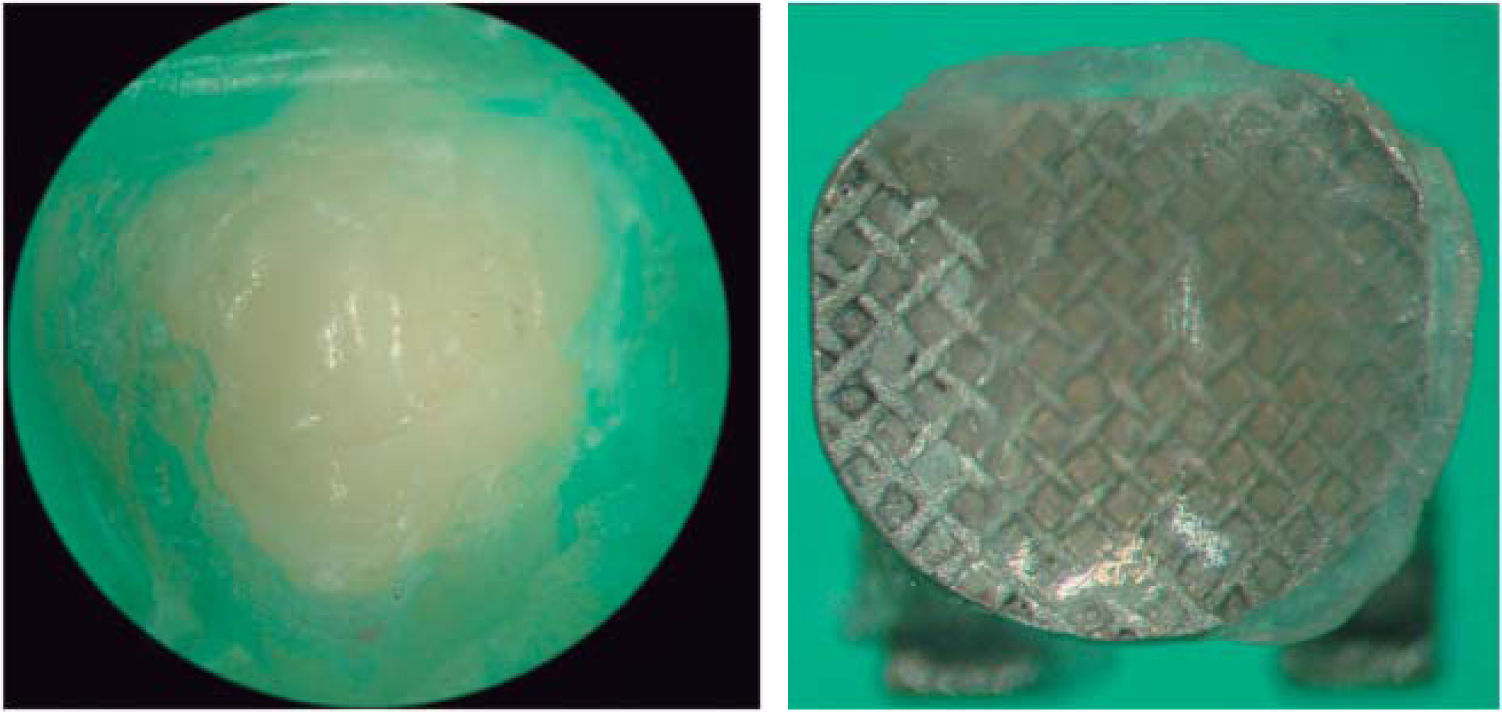
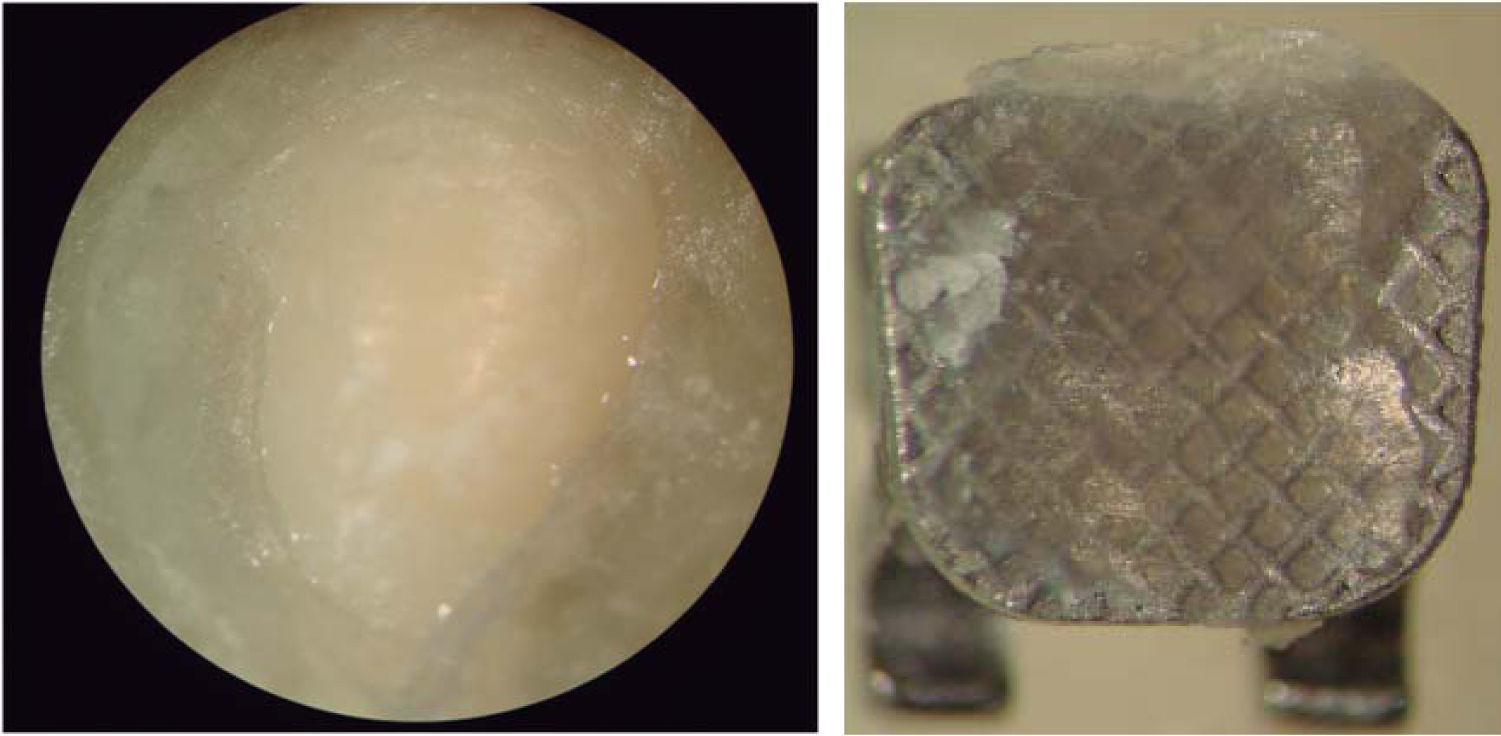
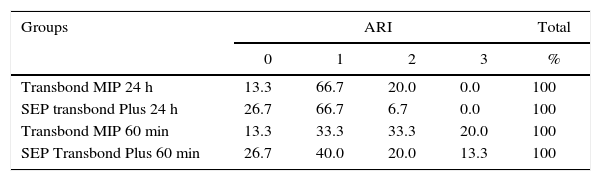
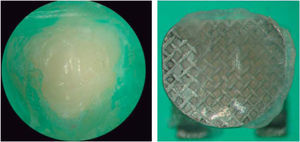
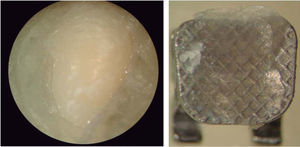
Remnant adhesiveThe surface of each tooth was examined with a 10X optical microscope to determine the location of the failure in the adhesive interface by using a modified adhesive remnant index. The ARI scale has a 0 to 3 rank; the 0 value represents no adhesive in the enamel surface, 1 less than 50% of the adhesive left on the enamel, 2 more than 50% of the adhesive left on the enamel and 3 100% of the adhesive left on the enamel.
Statistical analysisThe ANOVA analysis was used for both groups to obtain significant differences between etching protocols, debonding times and their interactions. All the combinations of treatment to evaluate shear bond strength were compared using the Levene’s test for equality of variances. The χ2 test was also used to determine the ARI significant differences between groups (P < 0.5).
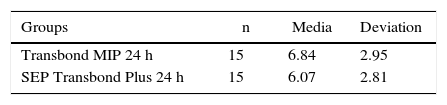
ResultsThe total sample size consisted in 60 teeth divided into four groups of 15. We used as adhesive systems Transbond Plus and Transbond MIP with debonding at 60 minutes and 24 hours respectively. The results were conducted with the ANOVA analysis thus obtaining in table I the comparison of the shear bond strength (MPa). The results show that there are no differences in the shear bond strength between Transbond MIP at 24 hours (mean=6.8 SD=2.9) and SEP Transbond Plus at 24 hours (mean=6.1, SD=2.8), the differences in the groups’ mean are not statistically significant (t=0.73 p=0.46).
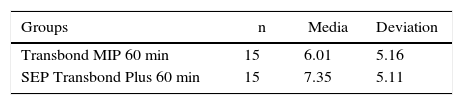
The comparison of the shear bond strength (MPa) is shown in table II. It demonstrates that there is no difference in shear bond strength between Transbond MIP at 60 minutes (mean=6.01 SD=5.2) and SEP Transbond Plus at 60 minutes (mean=7.35, SD=5.1), the differences in the groups’ mean are not statistically significant (t=0.71 p=0.48).
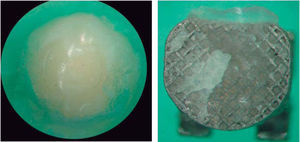
emspTable III shows the percentage distribution of the adhesive remnant index (ARI) test. Figures 1 to 4 show the representative photographs of the enamel surface and the bracket surface at 24 hours and 60 minutes after debonding.
Distribution of the percentage analysis of remnant adhesive (ARI).
| Groups | ARI | Total | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | % | |
| Transbond MIP 24 h | 13.3 | 66.7 | 20.0 | 0.0 | 100 |
| SEP transbond Plus 24 h | 26.7 | 66.7 | 6.7 | 0.0 | 100 |
| Transbond MIP 60 min | 13.3 | 33.3 | 33.3 | 20.0 | 100 |
| SEP Transbond Plus 60 min | 26.7 | 40.0 | 20.0 | 13.3 | 100 |
X2 = 12.07 p = 0.20 total
In our study we used two adhesive systems: Transbond MIP and SEP Transbond Plus. The debonding test as performed at 60 minutes and at 24 hours in the Instron universal testing machine. The modified adhesive remnant index (ARI) was also performed.
Turk18 evaluated the effect of two adhesive systems, SEP Transbond Plus and Transbond MIP at different debonding times: 5, 15, 30, 60 minutes and 24 hours with 100 premolars divided in ten groups of ten premolars each. We used those same adhesives and performed the debonding at 60 minutes and 24 hours on 60 premolars divided into four groups of 15 each. Turk obtained values for SEP Transbond Plus at 60 minutes of 13.13 MPa, at 24 hours of 19.11 MPa. For the Transbond MIP group at 60 minutes he obtained 12.32 MPa and at 24 hours, 16,82 MPa. These results do not correspond with the ones obtained in this study since we found lower values at 60 minutes and 24 hours than the ones they reported. On the ARI index they report a value of 3 for the majority of the sample. We agree in the ARI Index for SEP Transbond Plus at 60 minutes but not for the 24 hours group. For Transbond MIP at 60 minutes and 24 hours we agree. The variation in the results can be due to the sample size, the etching time since they etched with 37% orthophosphoric acid for 30 s in the samples where they used Transbond MIP and we etched for 15 seconds, following the manufacturer’s guidelines; in the inclusion criteria of our study, we selected teeth that had been extracted maximum three months before and they were refrigerated at 4 °C after the extraction while their study does not offer any data of this sort.
Likewise, Wade20 evaluated the SEP Transbond Plus adhesive’s influence at different application times. He used 40 molars divided in two groups of 20, the bracket base size was 10.3mm2 and it was from a lateral incisor. In group I the adhesive was applied for 3 to 5 seconds as the manufacturer recommend. In group II, the adhesive was applied for 15 seconds. He obtained values for group I of 8.0±4.6 MPA and for group II, 8.9±3.4 MPA. We agree with the values of group I where the manufacturer’s guidelines were followed and because their sample management was similar to ours.
Bishara8 compared debonding with two adhesive systems, light-curing with a halogen lamp (20 seconds) and with a LED light-curing unit (10 seconds) in 80 central incisors divided into 4 groups of 20 each. He placed metallic and ceramic brackets. They obtained a shear bond strength value for Transbond MIP of 4.6 MPa and SEP Transbond Plus of 8.6 MPa. In spite of the methodological differences we agree with the debonding values for both adhesives on metallic brackets so one can infer that the type of light-curing unit and the bracket base size do not affect the shear bond strength of these adhesive systems.
In a different paper Bishara20 evaluated the effects of two adhesive systems in orthodontics without finding any statistically significant difference between adhesives. Their methodology differs from ours in sample size, bracket base and debonding times but still under these variations we agree on the debonding values.
Lopez21 evaluated the retention force after applying the same adhesives we used with two types of bracket base and performing the debonding at 48 hours. They obtained values for SEP Transbond Pus of 7.65±2.83 MPA and for Transbond MIP, an average value of 6.95±2.06 MPa. These values correspond with ours thus confirming that placing the archwire to the fixed brackets 60 minutes or 24 hours later does not affect the shear bond strength.
Trite22 compared the bond strength and the ARI with three adhesive systems and different debonding times, obtaining in the majority of the sample a 1 value, in agreement with our values.
We suggest that more research is needed on self-ecthing adhesives in order to compare laboratory results with clinical cases. Future studies must be performed to structurally identify and analyze the enamel surface after bracket debonding to evaluate the integrity of the enamel during etching and at debonding in relation to the values obtained during the tests with the Instron machine. On clinical practice we need to do a follow-up to know the bonding failure percentage using different adhesive systems and times of archwire placement and also insect the debonded brackets during the orthodontic treatment.
ConclusionsUnder the methodology used for this study the results suggest that there are no statistically significant differences on shear bond strength at 60 minutes and 24 hours between SEP Transbond Plus and Transbond MIP with conventional method as adhesive systems.
In most of our sample less than half of the adhesive was left on the enamel surface.
To Master Jorge Guerrero Ibarra, professor from the Dental Material Research Laboratory of the Division of Postgraduate Studies and Investigation of the Dental School of the National University of Mexico.