The attention of patients with cleft lip and palate on the basis established by McNeil, Burston, Hotz, Gnoinski among others is hereby presented using a stimulating palatal obturator with 10 patients of the Orthodontics Service at the Children's Hospital of Mexico «Federico Gómez». Two patients didn’t return and one died before the second appointment. The benefits of presurgical orthopedics were observed, improving the patient's functional and physical appearance, such as swallowing, tongue position in the oral cavity, improvement in the relationship of the maxillary segments and narrowing of the fissure. Following the protocol established by the Children's Hospital of Mexico «Federico Gómez» based on the Zurich approach (McNeil, Hotz, Burston, Gnoinski, et al), the procedure resulted suitable for surgical preparation of palatoplasty and cheiloplasty in patients with unilateral cleft lip palate.
Se plantea el manejo de atención a pacientes con labio y paladar fisurado con base en lo establecido por McNeil, Burston, Hotz, Gnoinski, entre otros. Utilizando la placa obturadora estimuladora en 10 pacientes del Servicio de Ortodoncia del Hospital Infantil de México «Federico Gómez», de los cuales dos pacientes no regresaron a sus citas y uno falleció antes de la segunda cita; observándose beneficios de la ortopedia prequirúrgica mejorando el aspecto funcional y físico, como deglución, posición lingual en la cavidad oral, mejoría en la relación de los segmentos maxilares y estrechamiento de la fisura, siguiendo el protocolo establecido en el Hospital Infantil de México «Federico Gómez» con base en el enfoque Zurich (McNeil, Hotz, Burston, Gnoinski, et al), resultando muy adecuado para la preparación quirúrgica de queiloplastia y palatoplastia en pacientes con fisura labiopalatina unilateral.
The cleft lip and palate malformation occurs between the 6th and 12th weeks of embryonic life. As we know these are critical weeks in the development of the lip and palate.
A combination of normal connection failure or inadequate development in the abovementioned weeks, can affect the soft tissues and the bony components of the upper lip, the alveolar process as well as the palate thus the cleft lip results from the lack of fusion of the mesenchymal masses of the medial nasal and maxillary prominences while the cleft palate is a consequence of the lack of union between the mesenchyma of the palatal prolongations.
It has been determined that the etiology of this congenital malformation is very diverse and varied, however it is possible to classify the etiologic factors in two large groups: genetic and environmental.
In 25% of the affected children the cause of the cleft lip and palate is unknown and in the remaining 75%, the etiology is associated mainly to polygenic or multifactorial inheritance, as it is attributed to the result of complex interactions between a variable number of «minor» genes that act by additive action (polygenic) usually from hardly identifiable action and number and denominated in general terms as genetic predisposition and usually unknown environmental factors. It should be noted that from that 75% of the cases, only 25% has a family history of cleft lip and palate in its various expressions. It has also been observed that the majority of cases refer a prenatal history of drug ingestion, previous abortions and disorders during pregnancy, emotional disorders, maternal age of more than 40 years, metrorrhagia in the first trimester of pregnancy and gestational diabetes.
Current data suggest that the overall incidence of maxillofacial clefts is between 1:500 and 1:700 births, although in recent years because of birth control and genetic counseling, the incidence has decreased.
Dr. Ignacio Trigos published in the Journal of Plastic Surgery that in Mexico, cleft lip and palate, occupies the first place in birth defects, reporting 1.39 cases per 1,000 registered live births, that is one case per 740 live births. These data make it possible to identify that in Mexico there are 3,650 new cases per year, a figure considered as annual incidence of cleft lip and palate at a national level.1
It has been shown that lip clefts are more frequent in males, whereas isolated clefts of the palate are more common in women. Similarly, the cleft lip is more common on the left side than to the right. These phenomena lack of explanation and the underlying cause of the deformity is only partially understood.
Presurgical orthopedicsSince the 1950's, in Europe and the United States in the clinics of the cleft lip and palate the ideas of C. Kerr McNeil, Scottish prosthetist, have been considered as fundamental. He supported the use of presurgical neonatal maxillary orthopedics. Through his observations he learnt not to accept that middle third retrusions were due to a delay in development due to a traumatic surgery, and focused on what was established by James Scott who suggested that segments of cleft palate that were debrided downwards and forwards during surgery deprived the septum nasal of its growth impulse by keeping it short, deficient and thus causing depression of the middle third. So it was that McNeil initially suggested by assumptions and observations that repositioning of the maxillary segments using orthopedic appliances would produce an apparently normal maxilla. He created the theory that the action of the appliance would reduce nasal and labial distortion bringing the palatal segments closer together. McNeil stated that the use of orthopaedic appliances from the moment of birth for the alignment of the palatal segments in an ideal relationship corrects the bone deficiency by stimulating growth of the palatal segments. He interpreted that the cause of many middle third deficiencies was a strict condition of development deficiencies due to the debridement of the vomer during surgery. He even ventured for the first time (without evidence) that growth stimulation through a plate could eliminate almost all palatal fissures before performing the surgical procedure. The McNeil plates were initially built from a series of modified models where the cleft palate was gradually reduced. Each consecutive plate gradually corrected the position of the segments of the palate. These plates had areas of stimulation that pressed gently the palatal mucosa at a distance slightly short of the margins of the fissure. By doing this, he assumed that the light pressure would stimulate growth of the underlying bone thus reducing the width of the cleft.2
After the introduction of neonatal maxillary orthopedics also called presurgical orthopedics by C. Kerr McNeil more than half a century ago, it has been quickly adopted around the world, however, scientific evidence of its benefits has not been sufficient. From this moment on, different types of orthopaedic surgery have been described in the literature from fixed appliances with pins to passive plates on the opposite side. Arbitrarily these devices have fallen into three categories: active, semi-active or passive. In summary, active devices are those that will force the maxillary segments to be in a specific position using springs or screws; semi-active systems are those where the segments in a study model were moved to the most favorable position and subsequently by the plate is made on this new model, suggested initially by McNeil and Burston.3
Passive devices are those that produce an induction to arch alignment during growth by making adjustments to the plate in specific areas to ensure the spontaneous development of the segments. The plate is held in place by suction and adhesion only, without the need for a mandatory extraoral force. Here is where the so-called «Zürich approach» proposed by Hotz and Gnoinski arises. It is the best known representative of presurgical orthopaedics.
Before the development of the modern school of presurgical orthopaedics there were already in use connections of the clefts by using adhesive tapes thanks to Brophy and his studies where he proposed to connect both sides of the alveolar clefts with the objective of strengthening them for a subsequent lower lip correction.4
The suggested procedures were always based on the never proven assumption that a narrow close and well aligned fissure would be easier to repair with less disruption and minor soft tissue mobilization. Hence, a narrower cleft would lead to less tension in the repaired lip, however, McNeil adopted a different theory, the one proposed by the anatomist Scott which suggested that debrided palatal segments of the nasal septum considered as the growth center of the maxilla would remain poor and would retrude the face. When modeling the palatal segments to the correct anatomical position by using a number of acrylic plates he believed that he could produce a normal maxilla reducing the alveolar and palatal fissure at the same time. It is important to mention the additional benefits of the acrylic plate reported by Burston: it also facilitates eating and allows the child to adjust from the beginning to the plates in case he or she needs to use them in the future.5
In spite of the pros and cons of presurgical orthopedics, since the 1950s there has been a consensus of thought in which multidisciplinary work within a care center is the primary option for the treatment of patients with cleft lip and palate. The team will work as an organization where each member should be aware of the different aspects of treatment. It is here where orthodontics becomes an essential part of the organization from the outset because in most cases there will be a distortion of the arches and maxillary collapse and the results of the surgical reconstruction of the lip will depend on this. Presurgical orthopedics aims to ensure a good maxillary arch form in relation to the mandible and restore normal oral function.6
From the several studies performed by McNeil it has been established that the most important aspect of the presurgical treatment of patients with cleft was controlling and correcting the lateral segments, either unilateral or bilateral, and that the effect on bone stimulation plays a critical role in this correction. Forces that are within the limits of biological tolerance have been said to stimulate bone growth if applied to particular regions and in a direction that can return normal intense forces.5
It has been demonstrated that it is possible to narrow the fissure in order to achieve a correct anatomical position of the maxillary segments during surgery, in contrast to what was done in the past where it was weeks before the cheiloplasty could be performed. Now, to manage the processes from birth until the time for surgery improves the angle of the palatal shells to a more horizontal position.4
Prahl and collaborators summarize the arguments by which the orthodontist's intervention and presurgical orthopaedic treatment during childhood will bring optimal results:
- •
They allow a better swallowing.
- •
Prevent a dorsal position of the tongue in the fissure.
- •
Arch shape improves as well as the position of the alar base.
- •
Facilitates the primary surgery.
- •
Reduces the width of the anterior and posterior fissure.
- •
Prevents the initial collapse after lip surgery.
- •
Reduces the risk of bronchial aspiration.
- •
Improves nasal breathing.
- •
Positive psychological effects in the parents.
In the mid 50's based on the principles of McNeil, neonatal maxillary orthopedics protocols began in Zurich influencing different European clinics. After a long-term evaluation it became clear that forced approximation of the maxillary segments was not fully recommended. Consequently, the procedure was extensively modified to what would be called the «Zürich approach».7
In accordance with the contributions of Gnoinski and Hotz, the primary objective of presurgical orthopedics is not only to facilitate surgery or stimulate growth as was initially postulated by McNeil, but to take advantage of the intrinsic development potential. From 1969 and 1970 presurgical orthopedics was essential in Zurich while the surgical intervention was postponed in function to minimize the disturbance of subsequent growth to create optimal conditions for the development of the maxillary segments to its maximum potential, maintain or improve arch shape and monitor the effects of the lip closure surgery.7
The appliance initially proposed by Hotz and Gnoinski was a passive plate made of soft and rigid acrylic that was used 24hours a day approximately from 16 to 18 months when the surgical closure of the palate was performed. The hard palate was closed after five years of age. Thus, during the course of treatment the lip was closed at about six months. The posterior extension of the plate tended to adapt the uvula more closely to the specific anatomy of the human being. Arch alignment was achieved by performing selective wear of the acrylic in specific areas.
In accordance with the scientific fashion of that time, the findings with respect to the effects of treatment were based mainly on observations: orthopedic guidance along with optimal timing of surgery would fully provide beneficial effects.7
Subsequent evaluations yielded better results. Two stages of palatal closure were proposed ideally to improve the patient's diction; it is important to mention that at that time it was not demonstrated if presurgical orthopedics had an influence or not in the postsurgical results.
Afterwards, the «Brogan» technique performed a combination of what was suggested by Burston and McNeil with the Zurich approach. After the alignment of the maxillary segments with a loose passive appliance and extraoral forces, a passive plate with internal adjustments and the need of extraoral force was used.8
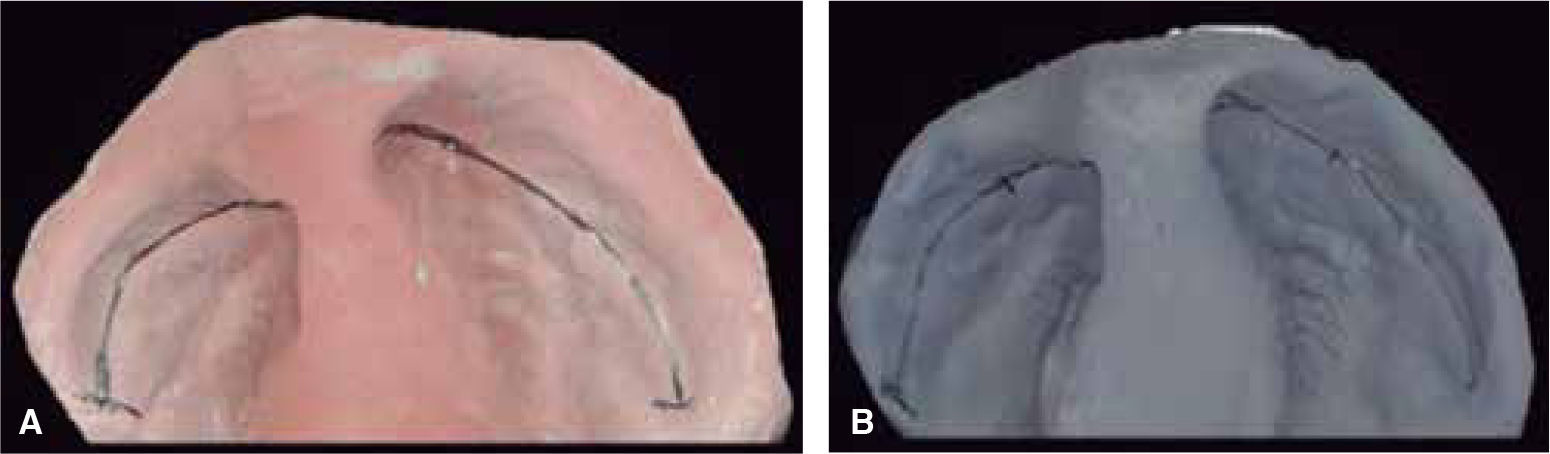
An important aspect related to the orthopaedic suggestion made by Hotz and his palatal plate is the possibility to make an adequate suction to the mother's breast and facilitate the patient's breastfeeding as the lack of contact in the palatal vault makes it impossible for patients with cleft palate to generate the negative pressure needed to press the breast and feed themselves. The Hotz appliance has an effect over feeding due to its mechanical seal that has been very well described. Therefore we find three important aspects in relation to food and the fuction of the Hotz plate: 1) it will help to achieve a good contact with the mother's breast as well as to close the fissure and the lip, 2) close the cleft of the hard palate, 3) provide a strong contact between the tongue and the «posterior palate» (Figure 1).7
The palatal plate on the appliance will close the connection of the upper airway when the tongue is pressed on the appliance. At this point the importance of maternal nutrition is emphasized due to the great amount of hormones acquired by breastfeeding, mainly estrogen, which helps the biological stimulation of the cleft bone segments and soft tissue to achieve maximum growth potential and an approximation of the same with greater ease and speed as cited above.
After the mentioned approach, it is possible to rescue that the principles of treatment of Dr. Hotz and Gnoinski have a strong impact on the treatment of cleft lip. It is possible that treatment sequence, the length of time it takes to perform it, the age of the patient as well as the surgical time are the decisive factors in treatment outcome.9
In particular, the stimulating plate is a modification of the one proposed by Hotz-Gnoinski. An artificial palate that helps prevent the tongue to enter in the nasal cavity and separate the segments of the palate, eliminating bad habits and directing it to be placed in the correct position on the palate, for correct language and swallowing was created thus achieving a seal on the palate that serves as a barrier between the nasal and oral cavities, preventing infection and injury, providing food and normal breathing; balancing the intraoral air pressure with the extraoral one, causing that during suction and swallowing air is compressed through the Eustachian tube (Figure 2).
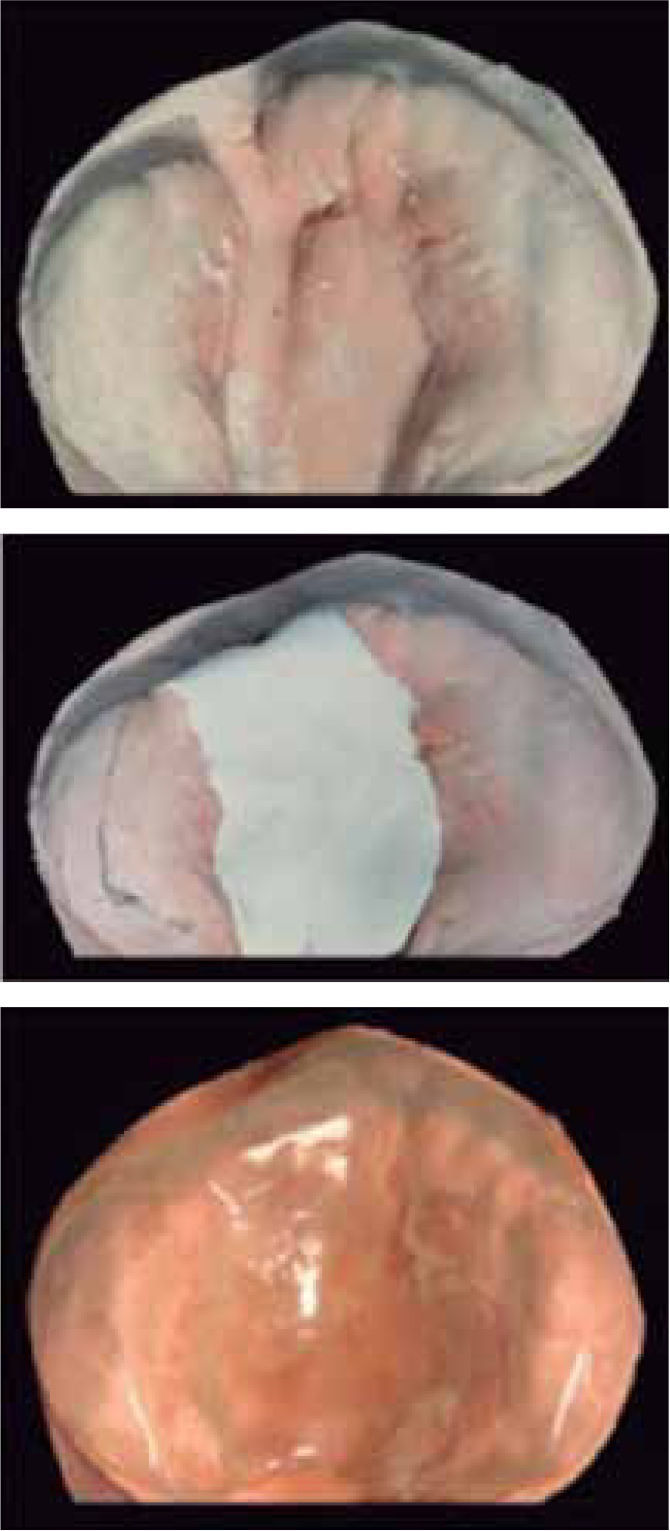
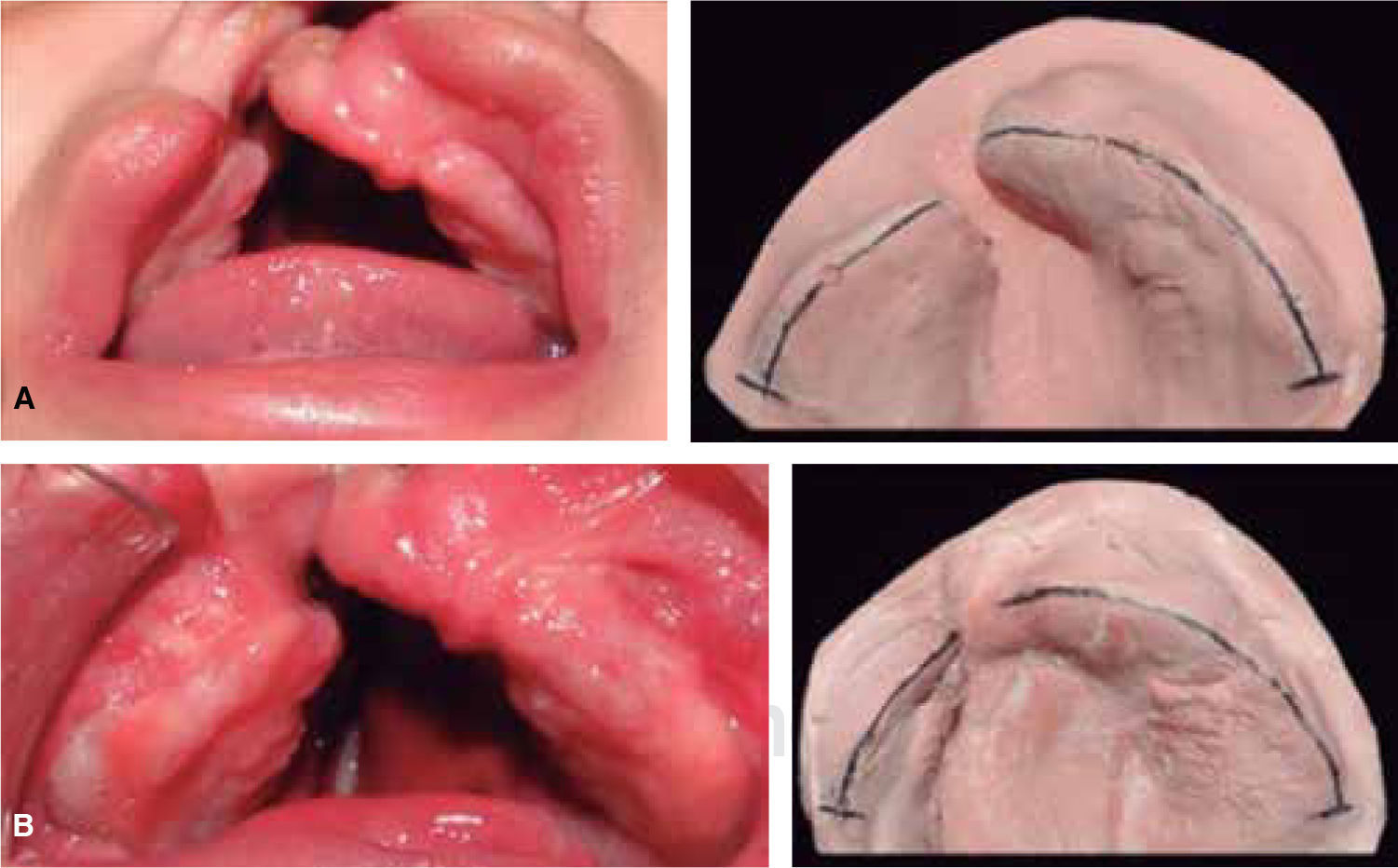
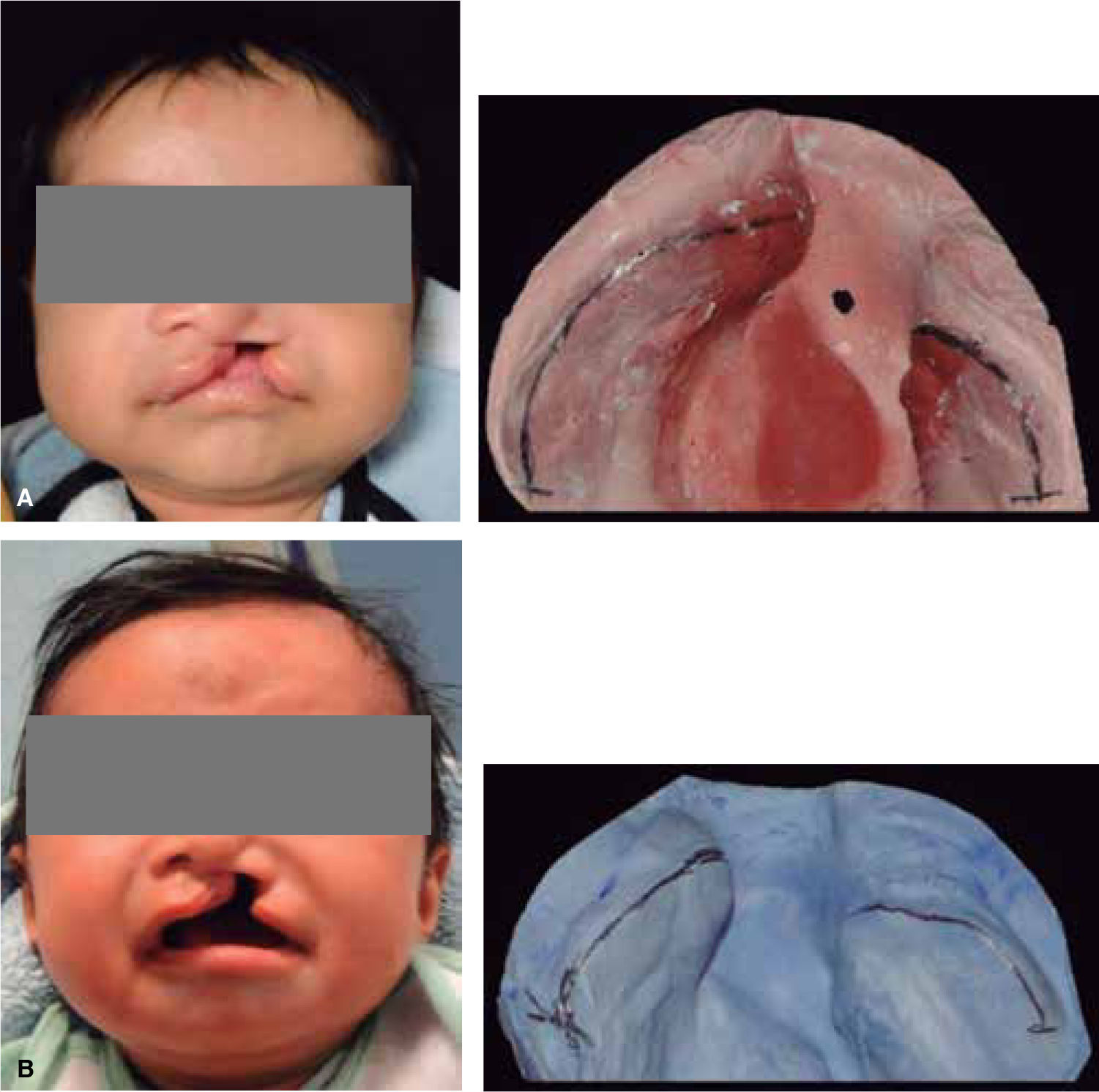
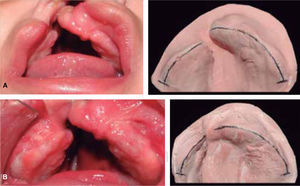
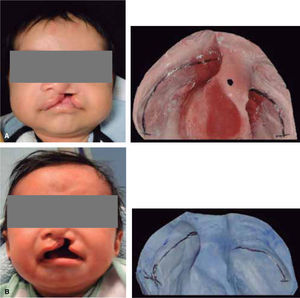
MATERIAL AND METHODSThis was a descriptive longitudinal study of series of cases where a presurgical management was conducted in 10 patients between 0 and 8 months of age with unilateral cleft lip and palate who attended the Orthodontics Service of the Children's Hospital of Mexico «Federico Gómez». During the study period, seven patients were constant, two did not return to consultation and one died a month old. Inclusion criteria consisted in patients with unilateral cleft lip and palate of 0-8 months of age (Figure 3) who arrived at the Hospital with a letter of acceptance and an informed consent signed by the patient's parent or guardian, as well as a pediatric assessment.
Patients who presented bilateral cleft lip and palate, patients older than 8 months, syndromic or with some kind of systemic problems were excluded from the study.
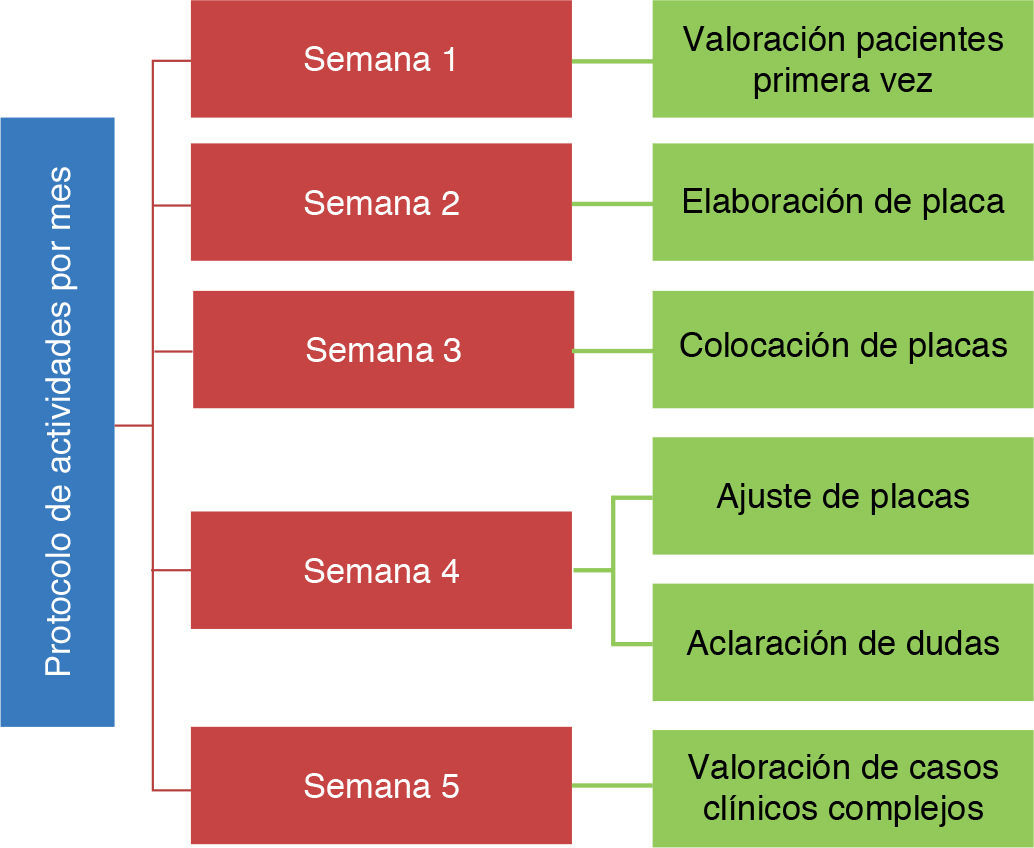
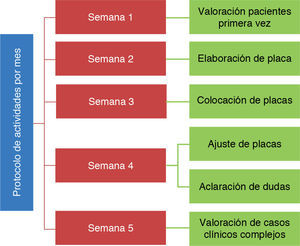
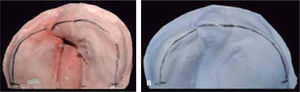
All patients were treated according to the protocol established at the Hospital Infantil de México «Federico Gómez» in accordance with the Zurich approach (Figure 4).
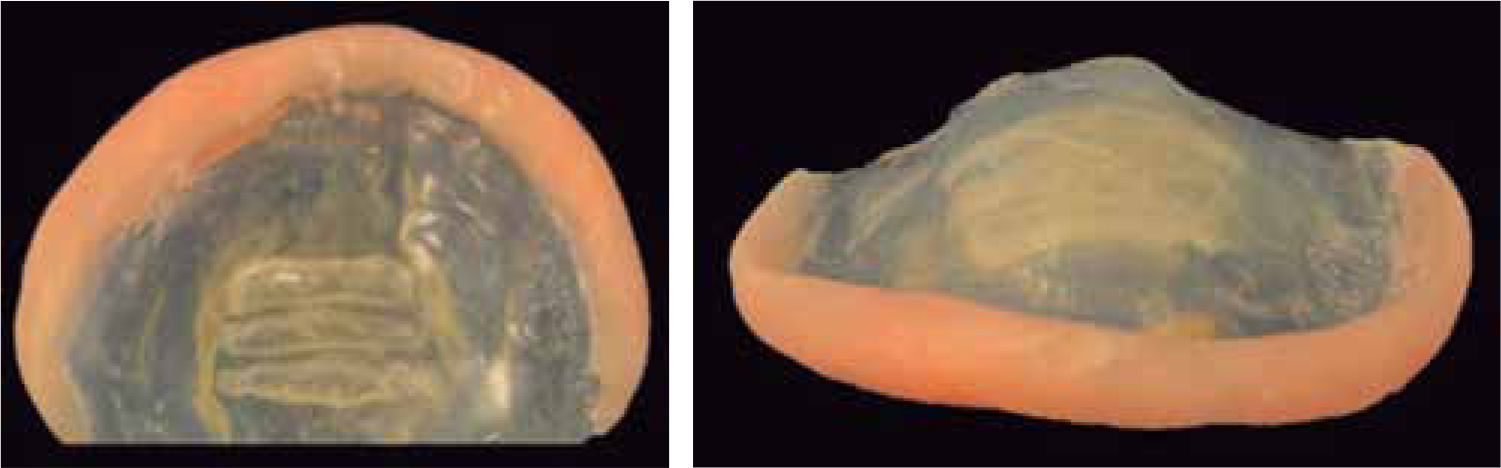
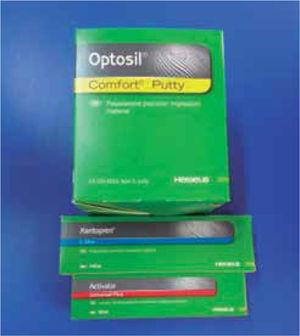
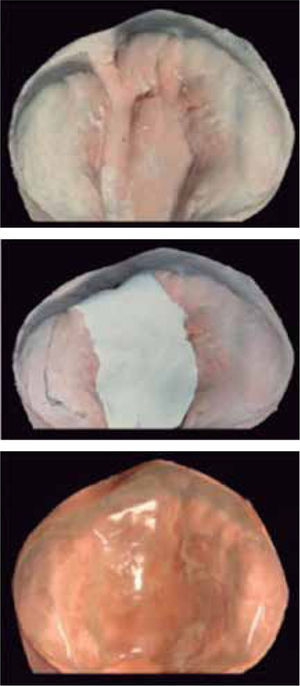
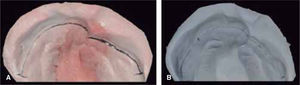
For the fabrication of the stimulating plate, an impression from the patient was obtained with a silicone impression material (Figure 5) and the patient's individual tray is prepared. Afterwards, a second impression is obtained as well as a positive with a cast type IV. Subsequently, modeling dough is placed in the model, in areas of alveolar ridges and regions of the hard and soft palate. In this phase, mainly, wax applied to the smallest segment of the buccal part and the largest segment of the palatal surface. After the waxing phase, the plate is prepared (Figure 5).
The circumferential edges of the prepared plate must be curved to avoid lacerations in the mucous. The posterior edges should be in contact with the soft palate and the extension must be tilted down; the posterior contact of the appliance should be reviewed carefully as it should never be too long to avoid inducing vomiting in the patient, nor too short to allow the food to escape into the nasopharyngeal area.
The majority of infants can suck after the device is placed. The adaptation process can last from two to three days. If this is not possible, breast milk may be given with a bottle. If the infant is fed with a bottle, you must stimulate the infant to suck since this will help the development of the labial musculature. After the appliance application, initial control should be less and the following appointments were scheduled on a monthly basis to monitor the development of the segments and make modifications to the plate such as the ones performed on the ruga palatina for a better adaptation of the tongue, wear on the inside and placement of acrylic on the outside edge of the plate. Added to this, since the initial appointment the patient was given a segment of Transpore 3M Unitek tape to join the labial segments and thus facilitate the lip adhesion at the time of the cheiloplasty (Figure 6).
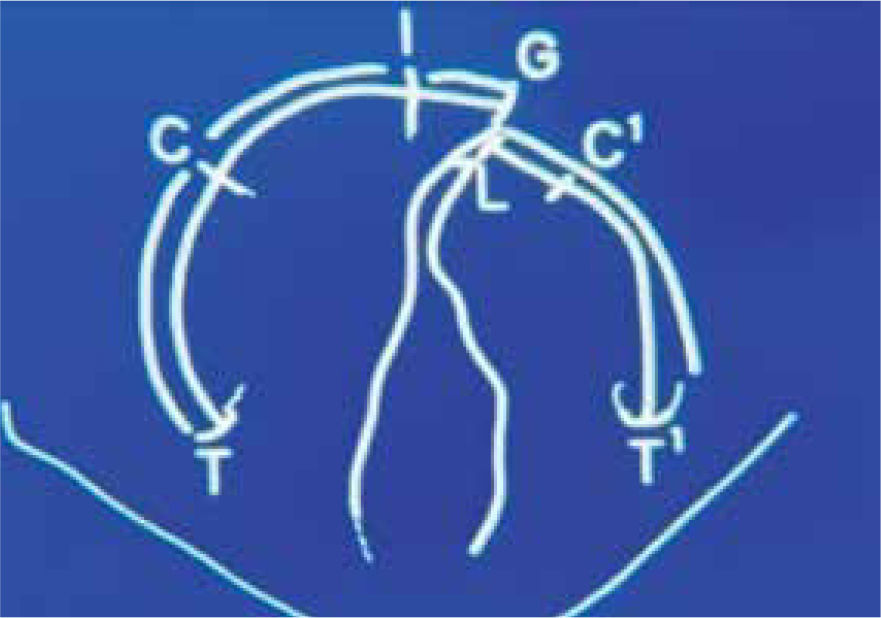
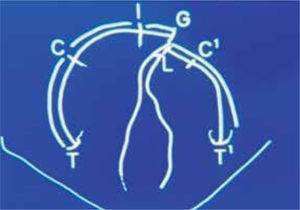
The location of the reference points for measuring was based on the ones performed by Rosenstein (1982) as shown in figure 7.
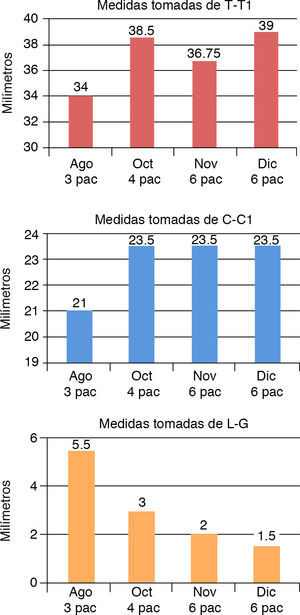
Data analysis to assess the change in time of each of the measurements was calculated using median values for each variable which were graphed to show the temporal trend.
For the descriptive statistics, the SPSS software version 18 was used.
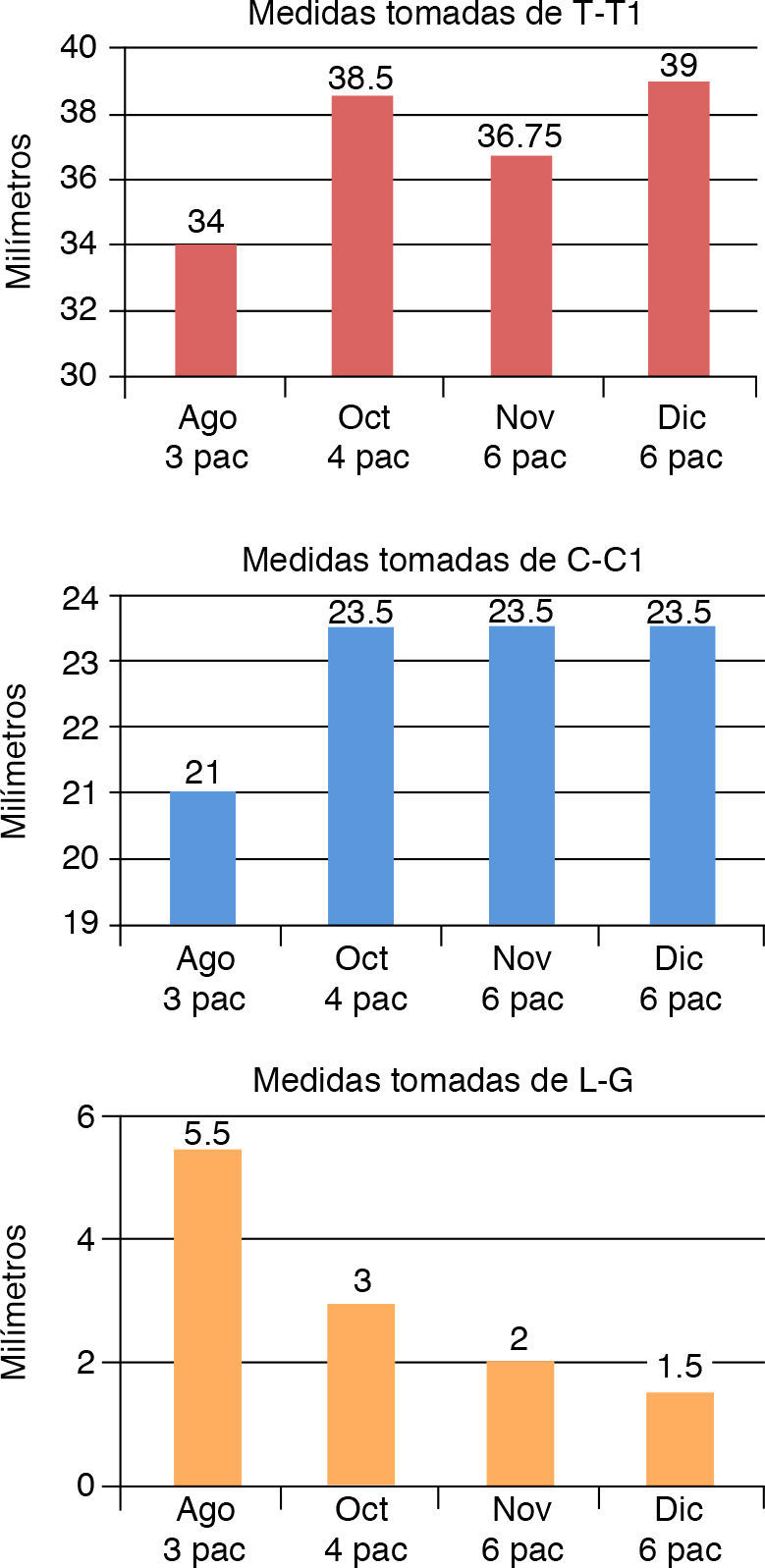
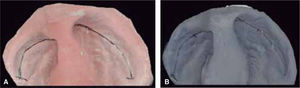
RESULTSIn this protocol, patients who used the stimulating obturator plate generally obtained good results as shown in the graphics (Figure 8).
The measurements of T-T1 and C-C1 indicate that the development of the processes had a good growth, expanding the arch shape.
The measurement of L-G, which is shown in the graph indicates that with the stimulating modeling plate the cleft was significantly reduced.
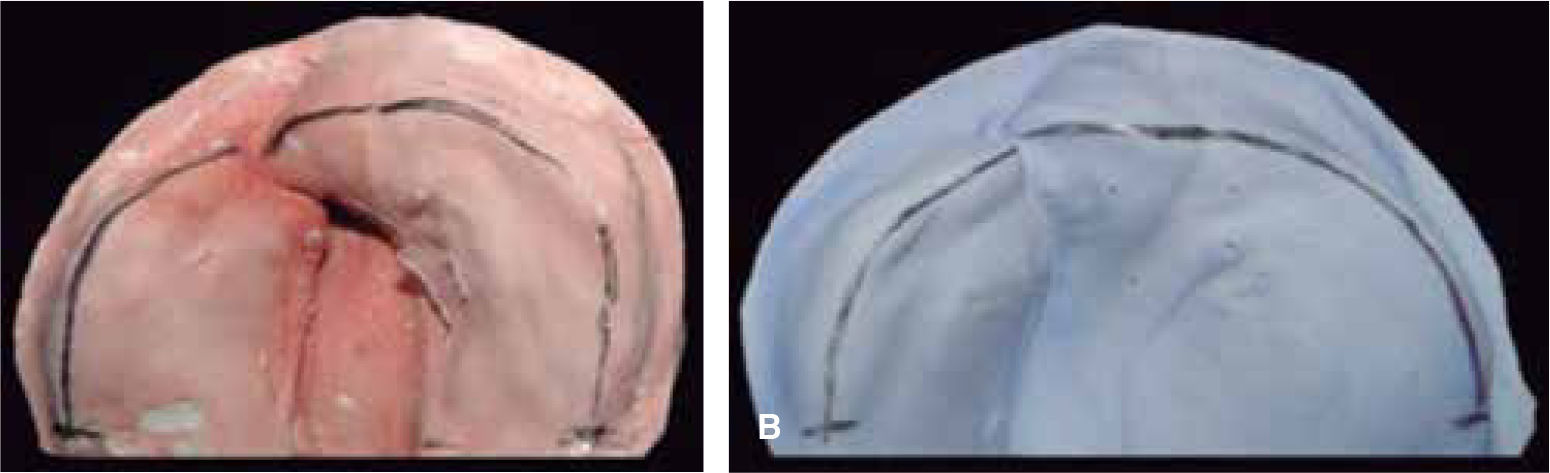
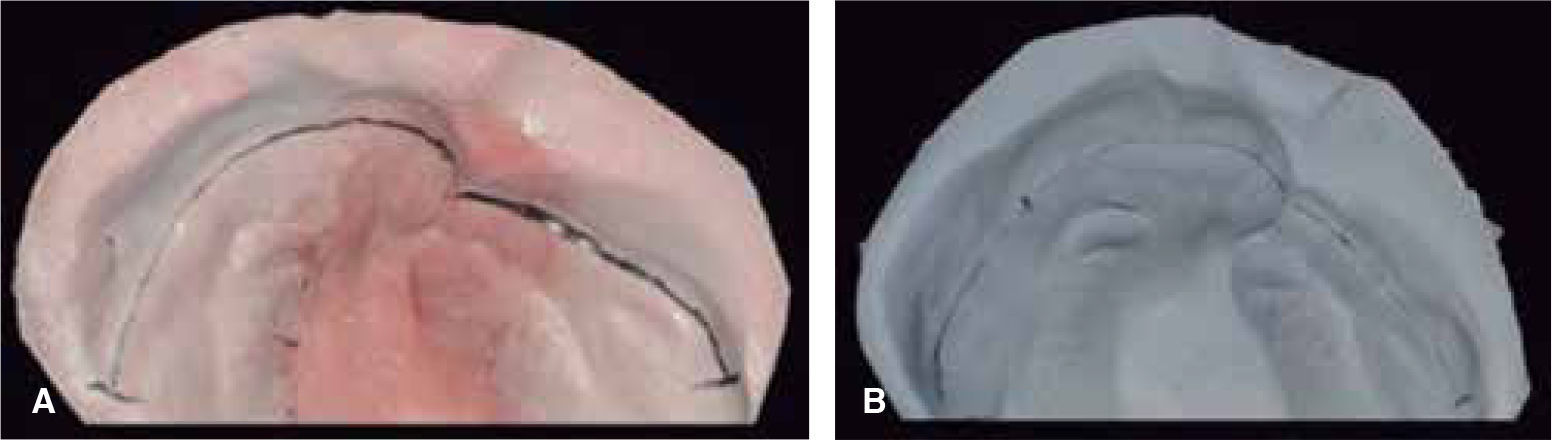
These measurements were made in each of the patients, thus observing the changes obtained in the patients (Figures 9 and 10).
The changes with the use of the stimulating modeling plate may be observed in photographs of the patients’ study models (Figures 11 to 14).
In the present study, we sought to emphasize the objectives obtained by presurgical orthopedics in patients with unilateral cleft lip and palate taking into consideration the anatomical-physiological bases of the anomaly and through this, determine the specific goals using the presurgical orthopedic therapy.
Based on the information provided by McNeil, Burston, Hotz and Gnoinski and their so-called Zurich approach, it was the intention to use a specific protocol to be able to provide treatment and follow-up of patients who present these anomalies that have a very high frequency. The modifications suggested by Freedman were performed on the appliance to fulfill the objectives sought in presurgical orthopedics.
It is evident that the number of clinical cases shown is small and this was due to several factors such as logistics, economic status of the patients, geographical location of each patient as some were referred from clinics in the province of the country; however the established protocol will lead to an increase in the study universe in the near future and a statistical assessment of the results looking for significance.
The results obtained in relation to the use of the stimulating plate and the suggested protocol provide data of utmost importance for future work in this regard, as these results were very favorable in most of the cases and according to what was reported by Hotz and Gnoinski in their study, our results were not too distant from theirs.
It was possible to observe improvement in the anatomical and physiological aspects of the patients as well as in the psychological aspect of the mother during follow-up. In the majority of patients, it was observed that feeding patterns improved showing a favorable weight gain in the patients; arch form and proximity of the segments improved significantly thus we hope that the postsurgical results are extremely favorable. From the psychological aspect of the parents, an improvement was observed since the mother of each patient visited with increasing interest the service at the time of consultation and referred a good response from the patient when using the stimulating plate. From the aspect of feeding, specifically breastfeeding, swallowing and an increase in weight were also observed thus favoring the development of the segments and the relationship between them. These results match what was reported initially in the investigations made by Hotz.
The use of a passive appliance in neonatal patients supported the patient in every aspect since a noninvasive method will allow a good physical, physiological and psychological development of the newborn.
Despite the fact that some articles refer that the use of presurgical orthopedics is a treatment that does not lead to favorable results and some even indicate unfavorable results, we have the strong belief that this treatment does provide good results as it was shown in this paper. It is important to mention that the postsurgical results after the orthopedics will be described in a subsequent study to obtain an adequate follow-up of the patients and as was already mentioned, statistics to assess the results of presurgical orthopedics in a larger population.
The proposed protocol is easy to be carried out as long as the staff is qualified and trained to perform the steps described above; it is important to mention that it is a protocol with a high cost-benefit ratio that can be implemented in clinics of all levels.
Due to ethical issues, it was determined to treat all patients with the same method and obtain measurements at the start of treatment and observe the evolution with the use of the stimulating plate. It was not the intention of this study to generalize the results but show the benefits obtained with the therapy. It is important to mention that these procedures were performed with consent from the patient's parents according to the regulation of the Children's Hospital of Mexico «Federico Gómez» orthodontic service.
CONCLUSIONSThe results observed after the use of the stimulating plate are consistent with what was reported by Hotz, Gnoinski and others. The good arch relationship and the narrowing of the fissures are evident in the majority of cases so that it can be concluded that presurgical orthopedics with the use of a stimulating plate is an acceptable therapy and is recommended for patients with complete unilateral cleft lip and palate.
With the patients included in the presurgical orthopedics protocol we found that it is recommended to increase the numbers of patients to perform a statistical analysis in the future.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia