Case report of an 11-year-old female patient with bilateral cleft lip and palate sequelae complete on the left side, incomplete on the right side with absence of upper lateral incisors and enamel hypoplasia on tooth #21. Treatment objectives were: to achieve functional occlusion, improve facial and dental esthetics, improve her quality of life by encouraging her self-esteem. An orthodontic treatment was performed with the use of 0.022 Roth brackets and with the extraction of lower first bicuspids as well as the remaining temporary teeth. Vertical elastics where used to settle the bite. At the age of 16 a removable denture was used to rehabilitate the area of the missing upper lateral incisors and to place a restoration on tooth #21. Surgery was performed to place a bone graft on teeth 12 and 22. Once growth has ceased dental implants will be placed. A lower fixed and an upper circumferential retainer was used.
Paciente femenino de 11 años de edad, con secuela de labio y paladar hendido bilateral completo de lado izquierdo e incompleto de lado derecho, ausencia de incisivos laterales superiores e hipoplasia del esmalte en el diente 21. Los objetivos del tratamiento fueron lograr una oclusión funcional, mejorar la estética dental y facial, elevar su calidad de vida; favoreciendo de esta forma su autoestima. Se realizó un tratamiento ortodóncico con aparatología Roth ranura .022, se hicieron extracciones de primeros premolares inferiores así como de los dientes temporales que se encontraban presentes. Se utilizaron elásticos verticales cortos para asentar mordida y a los 16 años de edad se remitió al Departamento de Prótesis donde se le realizó una prótesis transicional removible para rehabilitar el área de incisivos laterales ausentes y se restauró el diente número 21. El Departamento de Cirugía se encargó de colocar un injerto óseo autólogo en la zona de los dientes de 12 y 22 para la posterior colocación de implantes dentales una vez que haya cesado su crecimiento. Se utilizó retención fija inferior y retenedor tipo circunferencial superior estético.
Lip and palatal fissures constitute one of the congenital malformations that most frequently affect facial structures of the human being. Due to their location, they constitute an important biological and psychological problem that has repercussions on the family and in the social environment.1
Naso-labial-alveolar-palatal fissure is the name of the congenital craniofacial malformations produced by embryologic defects during the formation of the face. Its degree of severity focuses on certain areas of the facial complex, especially the upper lip, the premaxilla, hard palate and the floor of the nasal fossa.2
These fissures occur when the elements of the upper lip and the left and right palatal segments, do not merge within the first nine weeks of intrauterine life, being the sixth week the one with the higher risk.1
Fissures may have a genetic cause or develop through the action of teratogenic agents or illnesses contracted by the mother during pregnancy. Environmental factors also contribute to the development and expression of this malformation.3
One of the most commonly used classifications is that of the WHO which uses a decimal system to describe the categories of the fissures and the classification of Kernahan and Stark in which a diagram is used in form of a «Y» in order to depict the anatomical organs to diagnose.4
The incidence of CLP in Mexico, according to Armendares and Lisker, is rated at 1.39 cases per 1,000 births live births.5 According to the Single Information System for Epidemiological Surveillance (SUIVE), in Baja California there were an average of 18.7 new cases per year during the period from 2003 to 2006.6
Due to the complexity of the malformation, a multidisciplinary rehabilitation approach is required which involves several health areas. To mention a few there is Pediatrics, Otorhinolaryngology, Psychology, Phoniatry, and Plastic Surgery as well as those of the dental area such as Maxillofacial Surgery, Periodontics, Prosthodontics, Maxillofacial Prosthetics and Orthodontics which coordinates along with Maxillofacial Surgery the surgical times for graft placement.
In 1961 it was reported for the first time in the English literature the closure of a nasoalveolar fistula described by Boyne and Sands, who showed that the development of the maxilla could be further enhanced if bone grafts were performed in the appropriate stages. They described four ideal stages for graft placement and nasoalveolar fistula closure.7
- 1.
Primary bone graft
It is performed during the first months of life, and consists in placing the graft in the cleft site. Nowadays, if used, it should be combined with maxillary orthopedics.
- 2.
Early secondary bone graft
This procedure is performed before the eruption of the permanent teeth between the ages of five to eight years. The main advantage is that it produces a bony guide for the eruption of the lateral incisor and canine if they are present.
- 3.
Secondary bone graft
This bone graft is performed in the mixed dentition, between the age of eight and 12 years in conjunction with orthodontics to bring the maxillary segments closer before surgery. Ideally, grafting should be performed when the canine root is located ½ to ¾ from its complete development.
- 4.
Late secondary graft
It is performed when the permanent dentition is already present in order to give continuity to the alveolar ridge and favor rehabilitation.
According to their composition grafts are classified into:
Allograft: compounds of tissues taken from an individual of the same species but genetically different.
Xenograft: compounds of tissue taken from a donor of another species.
Alloplastic: synthetic and/or natural, such as hydroxyapatite.
Autograft: it is composed of tissue taken from the same individual.
An autograft may be obtained from extraoral areas such as the iliac crest, tibia, rib and calvarium; as well as from intraoral sites such as the maxillary tuberosity, zygomatic bone, mandibular ramus and mandibular symphysis;8 which is a donor area with easy access.
Chin characteristics make it an ideal material for increasing the transverse dimension of the alveolar crest, especially in the maxilla and posterior areas of the mandible, and even more so if implants are going to be placed.9
Within the biological advantages of chin bone grafts, the following may be highlighted:
- 1.
Medullary bone provides osteoinductive properties, while the cortical serves as a biological membrane to provide osteoconductive properties.9
- 2.
Cortico-membranous bone is re-vascularizes faster than thicker spongy grafts 9.
- 3.
They allow greater capacity for bone regeneration.9
- 4.
They have a slower resorption capacity, compared to other autogenous bone grafts, thus promoting long-term bone regeneration.9
Female patient, 12 years of age, who attended the Orthodontics Post-graduate Program of the UABC, Mexicali -The reason for consultation was; «I have non-aligned teeth». Routine studies were requested. Upon clinical examination an asymmetric, oval-faced, dolichofacial patient is noted; convex profile, retrusive chin, slightly increased lower third, a sequel scar of a bilateral lip cleft, thick lips and a hypoplasic and flattened alar cartilage and short collumnela (Figure 1).
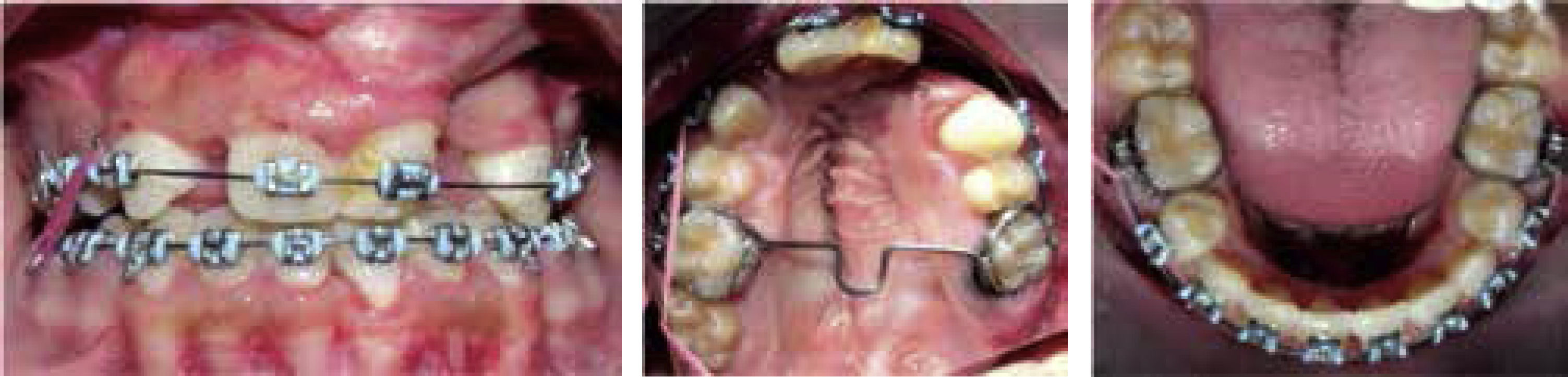
Intraoral clinical examination revealed an anterior and posterior crossbite as well as collapse of maxilla on the left side and a mixed dentition. A scar that runs from the alveolar ridge of the left side that involves the hard and soft palate is observed. A tooth in the fissure line may be observed as well as upper and lower crowding, an enamel defect of the upper left central incisor, bilateral molar class I, an indeterminate canine class and arch incoordination (Figure 2).
In the panoramic radiograph, a mixed dentition, congenital absence of the upper second premolars and the upper right lateral incisor as well as the germs of the upper and lower second molars may be observed (Figure 3).
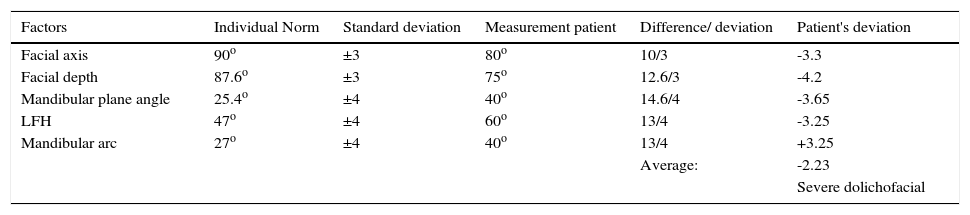
DIAGNOSISJarabak-Roth cephalometric analysis revealed a skeletal class I diagnosis with a clockwise growth direction, upper and lower incisor retroclination and according to Ricketts’ VERT, she is a severe dolichofacial patient with bilateral molar class II in centric relation. According to Pont's Analysis, the patient presented an 8.9mm maxillary compression in the transverse width from premolar to premolar (Figure 4).
Problem list
- I.
Skeletal
- •
Class II.
- •
Bilateral cleft lip and palate sequelae.
- •
- II.
Dental
- •
Bilateral molar Class II and indeterminate canine at attempted Centric relationship.
- •
Sequelae of cleft lip and palate.
- •
Maxillary transverse collapse.
- •
Maxillary anterior and posterior crossbite.
- •
Upper and lower incisor retroclination.
- •
Upper and lower crowding.
- •
Absence of the upper right lateral incisor and upper second premolars.
- •
Enamel hypoplasia of the upper left central incisor.
- •
0mm overbite and overjet.
- •
Arch incoordination.
- •
- III.
Aesthetic
- •
Convex proile
- •
Lower third slightly increased
- •
Objectives
- I.
Skeletal
- •
To maintain Class II
- •
- II.
Dental
- •
To achieve functional class I molar and canine relationship.
- •
Maxillary Expansion.
- •
Uncross bite
- •
Eliminate crowding
- •
Coordinate arches
- •
Refer to the prosthetics department for rehabilitation of missing teeth in the fissure line and restore the upper left central incisor with the enamel defect.
- •
- III.
Aesthetic
- •
Maintain proile
- •
Do not increase the lower third
- •
| Factors | Individual Norm | Standard deviation | Measurement patient | Difference/ deviation | Patient's deviation |
|---|---|---|---|---|---|
| Facial axis | 90o | ±3 | 80o | 10/3 | -3.3 |
| Facial depth | 87.6o | ±3 | 75o | 12.6/3 | -4.2 |
| Mandibular plane angle | 25.4o | ±4 | 40o | 14.6/4 | -3.65 |
| LFH | 47o | ±4 | 60o | 13/4 | -3.25 |
| Mandibular arc | 27o | ±4 | 40o | 13/4 | +3.25 |
| Average: | -2.23 | ||||
| Severe dolichofacial |
Taking into consideration that the patient presented sequelae of cleft lip and palate, interconsultation with other medical specialties was carried out such as Psychology, Otorhinolaryngology, Phoniatry, Plastic Surgery, as well as with other dental areas: Periodontics to assess periodontal health, Maxillofacial Surgery to coordinate graft stages and prosthetics for dental rehabilitation.
Orthodontic treatment was performed with lower first premolar extractions due to the crowding and to the upper second premolar absence. A Quad Helix was used to achieve the expansion. Additionally, a transpalatal arch and a lingual arch as anchorage were placed as well as 0.022” slot Roth appliances.
The patient began treatment with upper fixed appliances. The alignment and leveling phase was initiated with 0.014” Nitinol archwires (Figure 5).
After six months, the extraction of the tooth that was in the fissure line was performed and 0.020” Nitinol archwires were placed. It is evident that a better upper arch form was achieved with the initial archwires, contributing to the correction of the anterior and posterior crossbite and thus avoiding the use of expansion with Quad Helix (Figure 6). At 12 months, 0.017” x 0.025” Stainless Steel archwires were placed and elastics for the correction of the canine class II at the right side (Figure 7).
0.019” x 0.025” SS archwires were placed subsequently with an open coil between the upper central incisor and upper left canine for correction of the midline that was slightly offset and for the correction of the canine class.
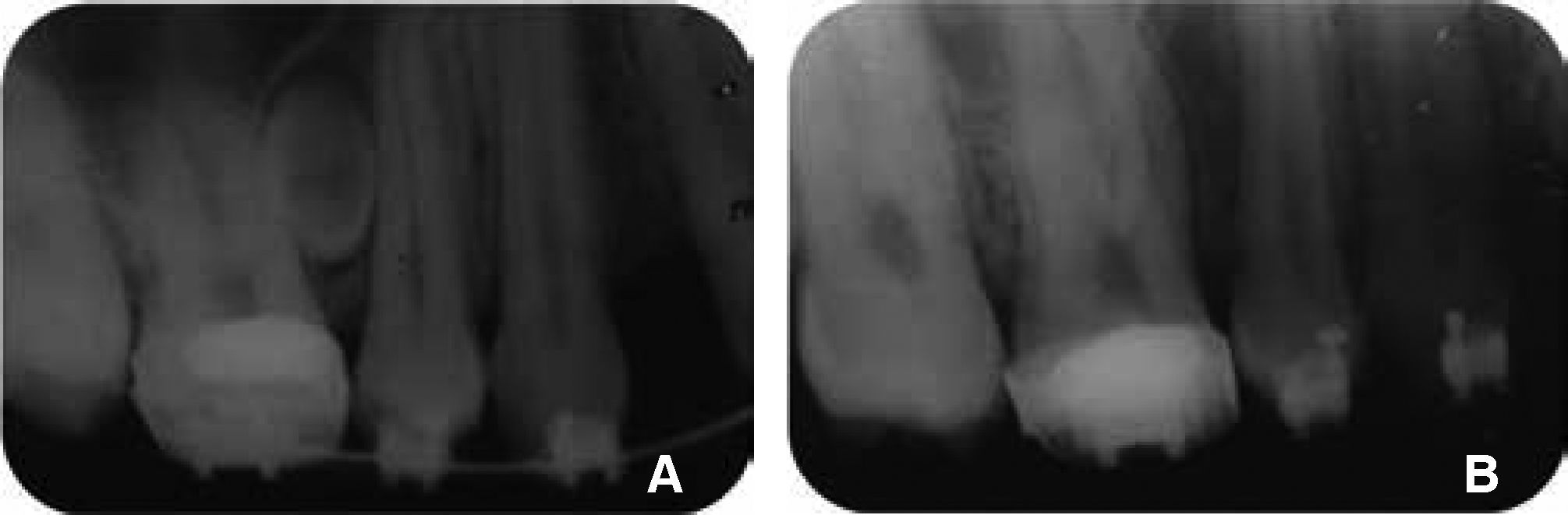
As a complementary study, a tomography was requested to corroborate that the teeth will be placed within their bony bases, and at the analysis, an amorphous tooth was found located between the roots of the first molar and upper right first premolar, which was removed (Figures 8 and 9).
First premolar brackets were repositioned and a transitional prosthesis was placed, adding the missing lateral incisors (Figure 10). In the course of the same month, the patient underwent a rhinoplasty and a cheiloplasty in the United States. Once close to finalizing orthodontic treatment, the late secondary bone graft was placed in the department of Maxillofacial Surgery, with the goal of encouraging prosthetic rehabilitation of the toothless area (Figure 11). This was followed up by an interdental papilla plasty of the dental organs #11 and 21. A diagnostic wax up for the prosthetic rehabilitation of the lateral incisors was performed (Figure 12).
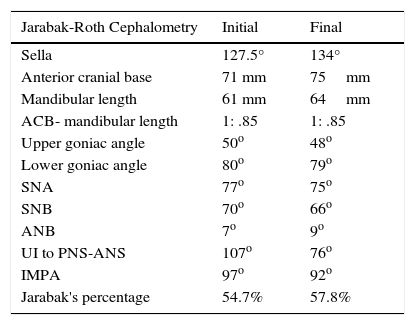
| Jarabak-Roth Cephalometry | Initial | Final |
|---|---|---|
| Sella | 127.5° | 134° |
| Anterior cranial base | 71 mm | 75mm |
| Mandibular length | 61 mm | 64mm |
| ACB- mandibular length | 1: .85 | 1: .85 |
| Upper goniac angle | 50o | 48o |
| Lower goniac angle | 80o | 79o |
| SNA | 77o | 75o |
| SNB | 70o | 66o |
| ANB | 7o | 9o |
| UI to PNS-ANS | 107o | 76o |
| IMPA | 97o | 92o |
| Jarabak's percentage | 54.7% | 57.8% |
An improvement in the patient's profile was observed (Figure 14), the transverse and anteroposterior collapse of the maxilla was corrected, a bilateral canine class I was obtained, arch coordination and a stable and functional occlusion (Figures 15 and 16).
Cephalometrically, a decrease in the UI/palatal plane angle was obtained, from 107o to 76o and in the IMPA there was a decrease of 5o (Figures 17 and 18).
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Second-year student of the Orthodontics Postgraduate Program.