Gingival enlargement is a chronic inflammatory lesion caused by bacterial plaque. It appears as a tumefaction at the level of the inter-dental papilla and/or marginal gingival tissue; it can be localized or generalized. It exhibits slow and painless progression and can be exacerbated by hormonal causes or use of drugs. The present article studies the case of a patient afflicted with gingival enlargement and gingival lesions induced by bacterial plaque. The case was resolved with use of non surgical periodontal therapy. For seven days, antibiotic therapy and manual therapy were conducted. Re-evaluation one month later revealed resolution of the enlargement, decrease of inflammation, suppuration, periodontal pocket percentage and degree of dental mobility; periodontal maintenance was executed at that point. After three months, decrease of periodontal pockets percentage and degree of dental mobility were observed; at that point maintenance periodontal therapy was conducted.
El agrandamiento gingival es una lesión crónica inflamatoria, cuyo factor causal es la placa bacteriana. Se presenta como una tumefacción a nivel de la papila interdental y/o la encía marginal, puede estar de manera localizada o generalizada, siendo de progresión lenta e indolora, pudiendo ser exacerbado por efectos hormonales o por el uso de fármacos. Este artículo reporta el caso de una paciente con agrandamiento gingival y lesiones gingivales inducidas por placa bacteriana resuelto mediante terapia periodontal no quirúrgica. Se realizó la terapia manual y antibióticoterapia sistémica por siete días. Al mes de reevaluación se evidencio la resolución del agrandamiento; reducción de la inflamación, supuración, porcentaje de bolsas y grado de movilidad dental, se realiza mantenimiento periodontal. A los tres meses se observa reducción en el porcentaje de bolsas periodontales y grado de movilidad dental; se realizó terapia periodontal de mantenimiento.
Increase of gingival volume is a common characteristic of gingival disease.1 Present terminology describes the condition as «gingival enlargement» or «excessive gingival growth».2,3 Chronic gingival inflammation can result in gingival enlargement.4 Chronic gingival enlargement is caused by prolonged exposition to dental plaque. Factors favoring plaque accumulation and retention include poor oral hygiene habits along with irritation caused by anatomical abnormalities and applying orthodontic forces, as well as inappropriate restorations.1,2
Inflammatory gingival enlargement begins as a mild tumefaction in the interdental papilla and marginal gingival tissue. This tumefaction can increase in size up to the point of covering part of the crowns. Enlargement can be localized or generalized and progresses in a slow and painless manner, unless acute infection or trauma complications arise.2 In some cases, chronic inflammatory enlargement appears as a sessile or pediculated mass, similar to a tumor. These enlargements can appear at interproximal level, and in marginal or inserted gingival.2 A spontaneous volume reduction can take place, followed by continuous exacerbation and enlargement. Chronic inflammatory gingival enlargements show exudative and proliferative elements which are characteristic of chronic inflammation showing vascular thickening, new capillary formation and related degenerative changes. Lesions are relatively firm, resistant and of a pinkish hue, they have a major fibrotic component with abundance of fibroblasts and collagen fibers.2 This excessive growth of the gingival tissue can be greater in patients with genetic factors or patients consuming drugs such as anticonvulsants, cyclosporine and calcium channel blockers; it can also be due to general systemic factors.4–6 In some of these cases, gingival enlargement can be reduced to a minimum by means of suitable personal oral hygiene and professional maintenance. Nevertheless, root debridement in patients with gingival overgrowth frequently does not restore normal contour to the periodontium.4–8 Excessive residual growth can not only hinder the patient's ability to suitably clean the teeth, it can cause as well esthetic and functional problems.4,5
The present article reports the case of a patient afflicted with gingival enlargement and gingival lesions induced by bacterial plaque. The case was resolved by means of non surgical periodontal therapy.
CLINICAL CASE PRESENTATIONA 71 year old female patient attended the Periodontics Masters Clinic at the San Martin de Porres University complaining of «pain in the gums, bleeding on brushing and two lesions which hindered chewing». During history, the patient revealed she was afflicted with Osteoporosis and Osteoarthritis, presently under treatment. Her last visit to a dental office had been three months before due to tooth extraction procedure caused by dental caries.
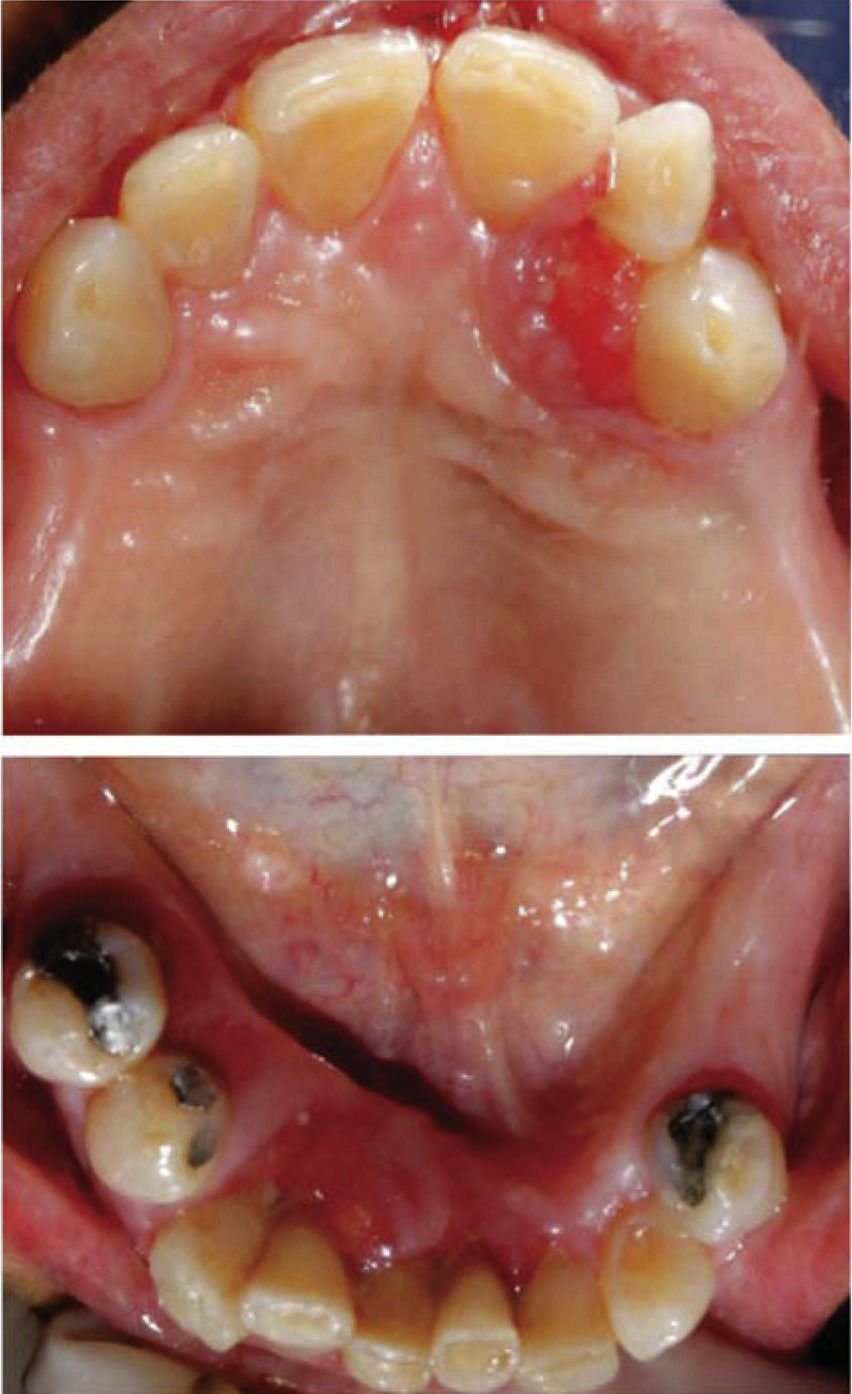
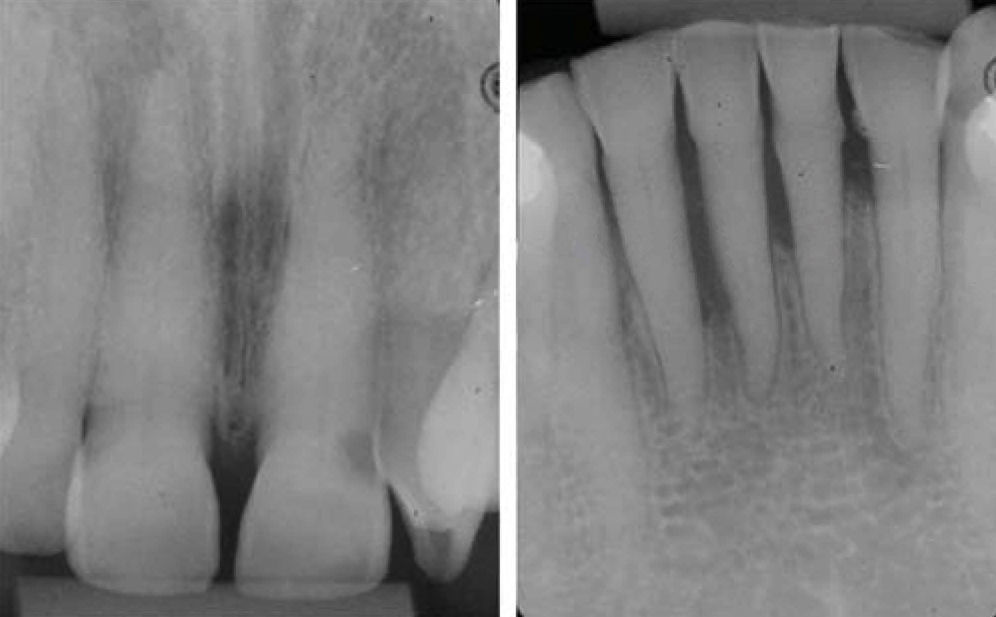
Initial intraoral examination revealed gingival inflammation surrounding most teeth, as well as a soft tissue lesion located at the marginal and inserted vestibular gingiva surrounding tooth number 2.1 with presence of suppuration (Figures 1 to 3). The lesion appeared as a sessile, erythematous mass with spontaneous bleeding, measuring approximately 1 × 1cm, with a 6mm periodontal pocket. Serial periapical X-rays were taken which revealed horizontal bone loss at upper and lower incisors (Figure 4).
Periodontal assessment established presence of periodontal pockets of up to 12mm depth in 35.56% of assessed sites. Grade 2 mobility was observed in teeth with bone resorption in the whole upper or lower anterior sector, as well as suppuration in tooth 2.1, and bleeding upon probing. According to O¿ Leary index, the patient exhibited an 80% (Poor) oral hygiene index. After assessing all obtained information a diagnosis of severe generalized chronic periodontitis was established, as well as acquired mucogingival deformities and lesions surrounding the teeth; «gingival enlargement». Thus, the following treatment plan was devised: oral hygiene instruction, root planing and scaling by sextants with systemic antibiotic therapy combined with a chemical agent. Re-evaluation and first maintenance session were conducted 30 days later. Moreover, surgical removal of the lesion was initially planned.
TREATMENTPhase 1 of periodontal therapy was initiated with oral hygiene instruction and motivation to the patient at each appointment, O’ Leary's index was used to record and reflect improvement. Use of a soft dental brush was recommended as well as adherence to Bass; brushing technique. Moreover, as supplementary instruments for hygiene, use of dental floss and inter-proximal brushes were recommended; their use was instructed at all treatment sessions, In a second session root flattening and scaling by sextants was established, as well as polishing all teeth. This procedure was conducted in a total of four sessions, with one day time interval between them. Root flattening and scaling was achieved with manual instruments using specific Jacquet scalers and Gracey curettes. Simultaneously, use of amoxicillin 875 mg/clavulanic acid 125mg by mouth every eight hours for a week was prescribed along with 0.12% chlorhexidine rinses every 12hours, 15ml for 1 minute during 14 days.
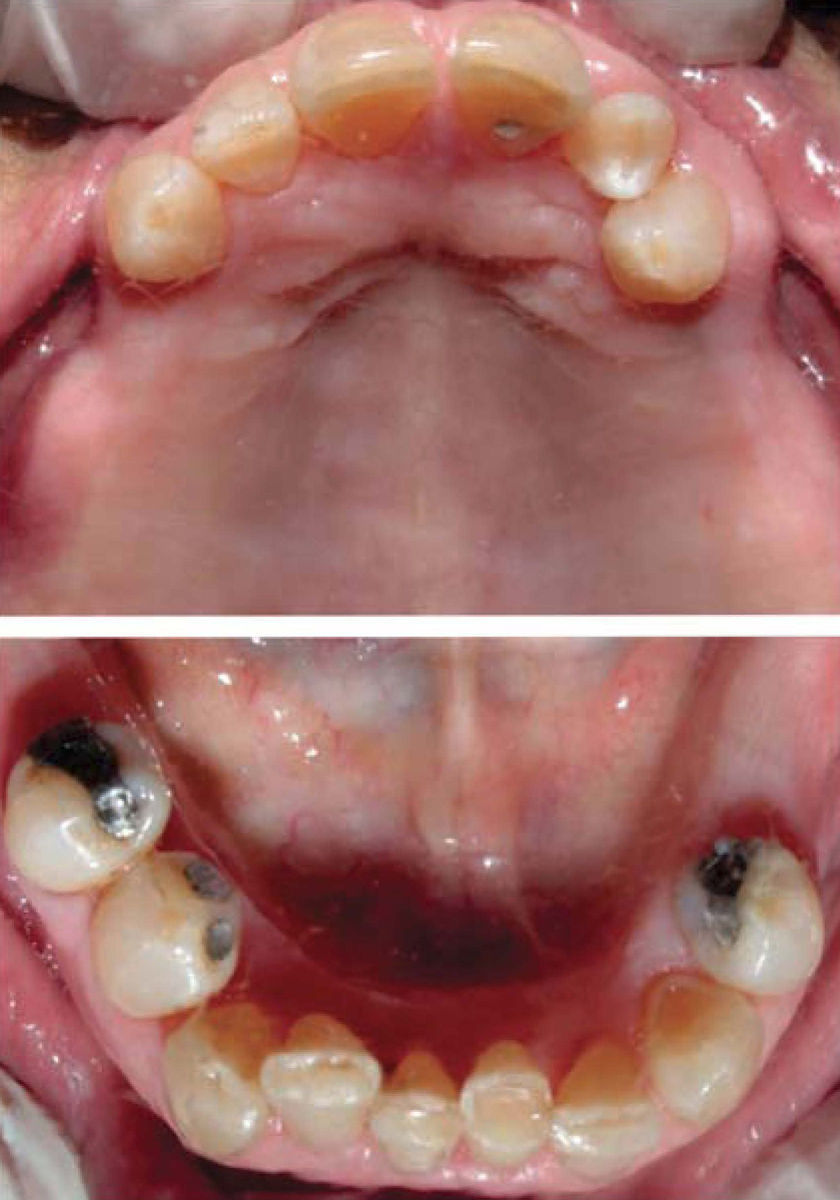
Re-evaluation after one monthO’Leary's index was once more applied as well as a periodontal study. In this assessment a 12.2% percentage of periodontal pockets was found, with depths of up to 7 mm; there was presence of grade 2 mobility in tooth number 4.1, absence of suppuration and 51.6% O’ Leary oral hygiene index (Poor) (Figures 5 and 6). Moreover gingival enlargement remission was observed, with the gingiva exhibiting a coral pink hue, firm consistency, even margins and healthy aspect. New root flattening and scraping was undertaken in areas with presence of dental plaque and active periodontal pockets. At a later point, the patient was referred for relevant. dental operative and prosthodontic treatments.
The following was observed at this re-evaluation: 5.5% percentage of periodontal pockets, with depth of up to 5mm, presence of grade 1 mobility in lower anterior teeth, absence of suppuration, oral hygiene index of 40% (O’Leary: Poor) (Figure 7). Periodontal maintenance therapy was once more conducted with manual instrumentation. The following re-evaluation appointment was programmed for three months later.
DISCUSSIONGingival disease associated to dental plaque, endogenous hormonal fluctuations, drugs, systemic diseases and malnutrition shares many essential characteristics. Universal characteristics of these gingival diseases include: clinical signs of inflammation, disease reversibility by means of etiology elimination, presence of bacterial plaque to initiate and exacerbate the severity of the lesion as well as a possible role as an insertion loss precursor.1 Clinical signs of gingival inflammation include enlarged gingival contours due to edema or fibrosis, transition to a reddish or bluish-red hue, bleeding upon probing and increase of gingival exudates.1
Gingival enlargement is a frequent finding in clinical practice, treatment is dependent on etiology as well as accurate diagnosis. The most common form of gingival enlargement is due to induced inflammation (inflammatory hyperplasia), which tends to be located at the level of interdental papillae. This clinical enlargement can be exacerbated by hormonal causes such as puberty or pregnancy, as well as by the use of certain drugs. Plaque-induced inflammatory hyperplasia must be resolved with removal of plaque and calculi, as well as improvement of patient's oral hygiene.7 In the gingiva; esthetically deforming excessive growth is a significant adverse result, it is mainly associated to use of anticonvulsive, immunosuppressant and calcium channel blocker drugs.1
Common clinical characteristics of gingival enlargement due to drug use include a variation among patients (this is to say, genetic predisposition) with a tendency to appear more frequently in the anterior region, greater prevalence in younger age groups, onset during the first 3 months of use, initiation at the papillae level, as well as finding a periodontium with or without bone loss.1
Nevertheless, in the present case, the following was observed: gingival inflammation, bleeding upon probing, presence of periodontal pockets, suppuration, dental mobility and gingival enlargement at papillary level and on attached gingiva. Dental plaque can be considered as etiologic factor of this lesion due to absence of other factors that might be related.
In patients afflicted with gingival enlargement, tissue topographic modification by means of surgical remodeling can be performed so as to create an oral environment suitable to maintenance. Recurrence is common in patients with drug-use induced gingival enlargement. For these patients, inter-consultation with the physician is necessary to determine the feasibility of using alternative pharmacological therapy which would not enlarge the gingival tissue; otherwise it might prove necessary to repeat the surgical procdure.4
In periodontal patients, mechanical, nonsurgical pocket treatment decreases inflammation and probing depth and increases clinical insertion levels.8,9 Nevertheless, residual plaque and calculi can still be found in spite of meticulous non surgical instrumentation. Therefore, surgical treatment might be advisable in cases of persisting inflammation.10
Heitz-Mayfield et al assessed effectiveness of surgical versus non surgical treatment for chronic periodontitis treatment by means of systematic review. For deep pocket treatment (> 6 mm) they reported that 12 months after treatment, surgical therapy resulted in 0.6mm additional decrease of depth upon probing, and 0.2mm gain of additional clinical attachment when compared to non surgical therapy. In periodontal pockets measuring 4-6mm root scaling and flattening resulted in 0.4mm additional gain in clinical insertion and 0.4mm less in depth upon probing when compared to surgical therapy. Based upon this it was concluded that root scaling and flattening alone as well as flattening and scaling combined with a flap procedure are efficient means for treatment of chronic periodontitis in terms of insertion gain and gingival inflammation decrease. Moreover, it was observed that in deep pockets (> 6 mm) debridement to flap resulted in a greater decrease of depth upon probing as well as gain of clinical insertion level.10 In the case presented in this article, only non surgical periodontal therapy was required in order to observe significant decrease of pocket number and depth as well as decrease of inflammation signs. The patient exhibited positive response, experiencing with time improvement in periodontal health circumstances; she exhibited remission of gingival enlargement as well as no relapse up to the moment of the last control.
Moreover, in periodontal therapy, there are reports in literature on the additional use of systemic antimicrobial agents.11,12 Justification for combination of these agents with non surgical debridement is the suppression of periodontal pathogens persistent in the biofilm of deep periodontal pockets, root bifurcations and concavities.10 Nevertheless, in certain instances, periodontal surgery might be necessary; in these cases there is controversy with respect to when it is more effective to prescribe the systemic antimicrobial agent; either in combination with basic periodontal therapy of with the surgical phase.11
Cionca et al found that systemic metronidazole combined with amoxicillin significantly improved clinical results six months after non surgical periodontal debridement of the whole mouth, thus significantly decreasing the need for additional therapy.10
Nevertheless, indirect evidence suggests that antibiotic intake must be completed in a short period of time (preferably lesser than a week),13 therefore, in the present case, one-week systemic antibiotic therapy was recommended during non surgical therapy, favoring thus achieved results.
Result re-evaluation after initial treatment is essential in order to suitably select additional therapy and establish in the long term the best possible prognosis. Traditionally, re-evaluation takes place a few months after initial periodontal treatment. Even though data support the fact that healing can continue during nine months after initial treatment, the greater part of the healing process is completed three months after treatment.8
Several retrospective studies have assessed the effectiveness of initial periodontal treatment (IPT) followed by maintenance periodontal therapy (MPT) In general MPT seems to be efficient in the prevention of recurrent periodontitis, if MPT is absent, risk of tooth loss increases. It has been shown that in patient with teeth gravely affected by periodontal disease, control of microbial concentrations and use of systemic antibiotic as supplement to non surgical MPT might decrease the need of tooth extractions. This shows that MPT is of paramount importance in the success of periodontal treatment.14
According to all the aforementioned, re -evaluation of the present case after three months showed great improvement in the following: decrease of percentage and depth of periodontal pockets, decrease of mobility degree, absence of suppuration, absence of enlargement relapse and lesser percentage of oral hygiene index (Table I). This evolution in the patient highlights the importance of observing maintenance periodontal therapy as well as the need to follow periodic and permanent follow-up of this type of patients so as to preserve long-term periodontal health.
Evaluation indicators and periodontal health state follow-up.
| Evaluation | Oral hygiene (O’Leary) (%) | Presence of pockets (%) | Probing depth (mm) | Bleeding upon probing | Suppuration | Mobility (Miller) |
|---|---|---|---|---|---|---|
| Initial | 80.0 | 35.56 | 6-12 | +++ | + | Grade 2 |
| 1 month | 51.6 | 12.2 | 4-7 | ++ | - | Grade 2 |
| 3 months | 40.0 | 5.5 | 4-5 | + | - | Grade 1 |