To find out the opinions, beliefs and concerns of the Spanish population on serious mental diseases: schizophrenia and bipolar disorder.
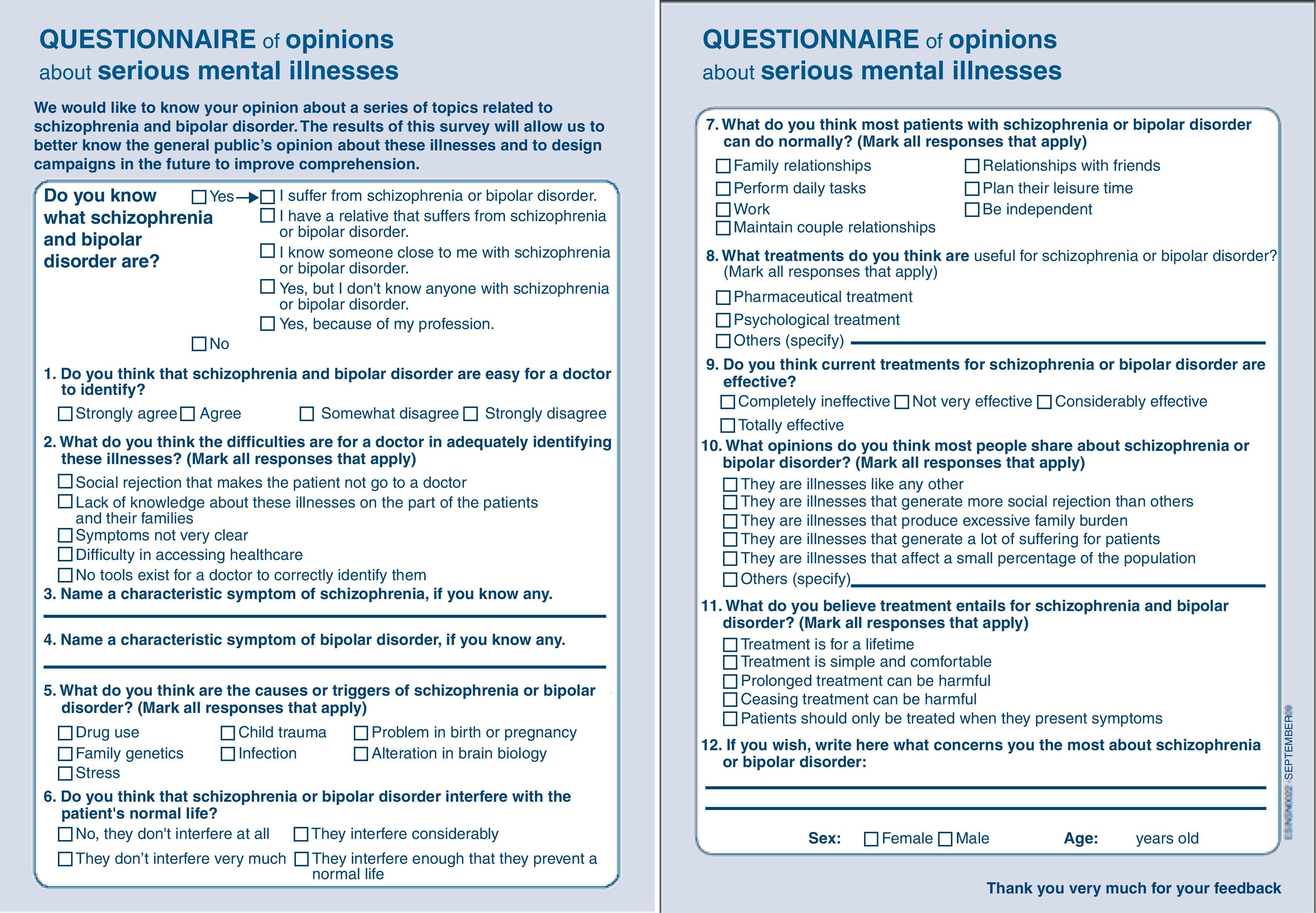
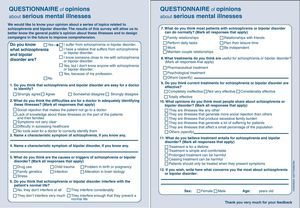
Materials and methodsAn ad-hoc questionnaire was constructed for the survey. A panel of seven experts extracted the contents. The Societies that involved were: ASAENES, ABBA, FEAFES-ANDALUCÍA, AMAFE, and AFAEM-5 advocacy societies were also involved. The questionnaire contained 12 questions about: knowledge of the diseases, diagnostic difficulties, symptoms, triggering factors, interference, treatments and effectiveness, beliefs and concerns. The questionnaire was administered during the IV Campaign of Social Awareness about Serious Mental Illness (Madrid and Seville, September–October 2009).
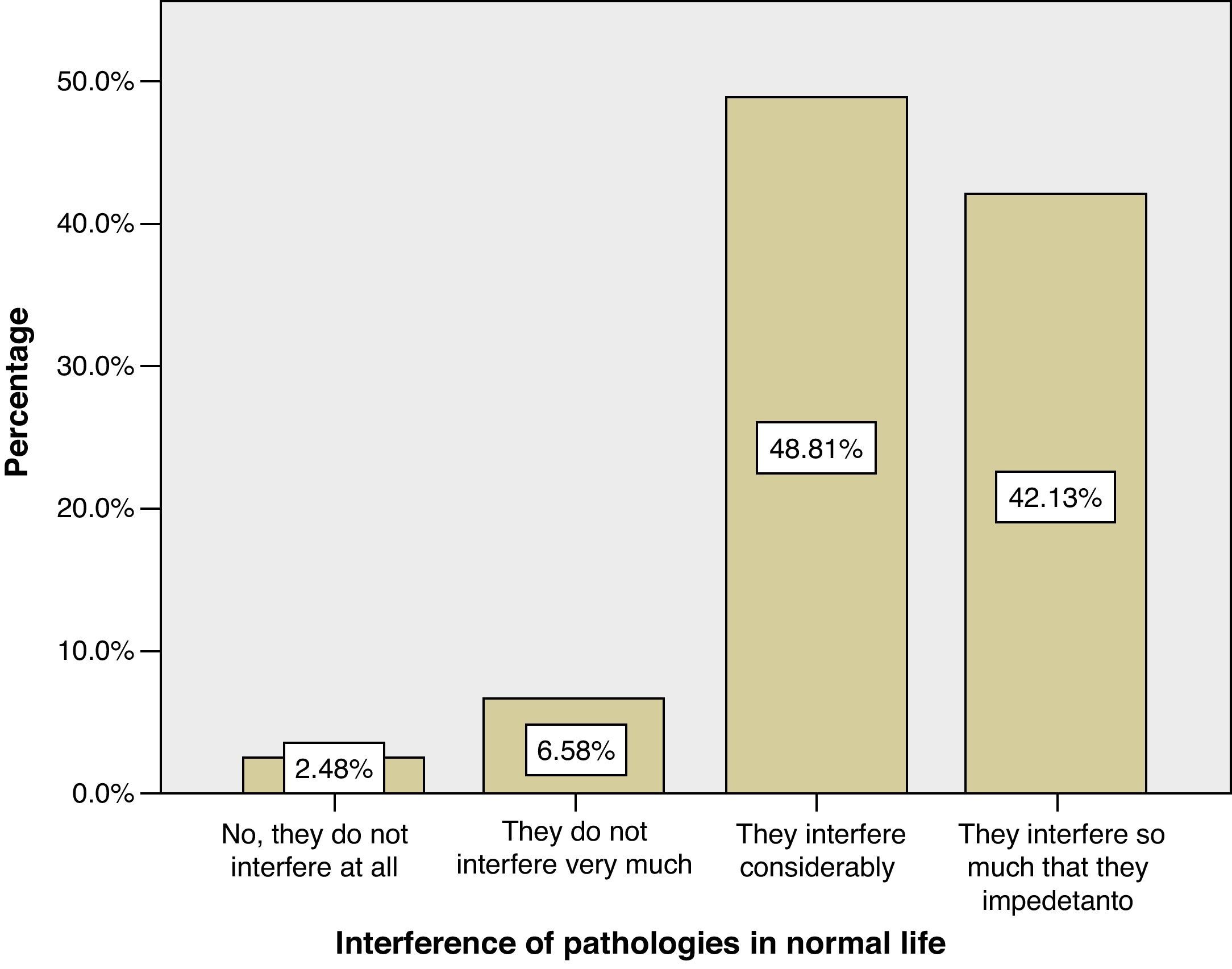
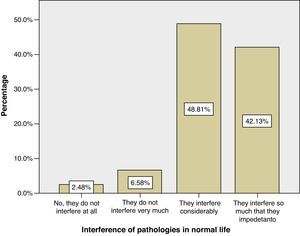
ResultsA total of 5473 questionnaires were collected, 55.8% in Seville. The majority (66.2%) of the sample were women, and the mean age was 35 years (SD=14.5). Both illnesses were known by 82% of the population, but 51% did not have any symptom of schizophrenia. Other notable opinions were: they are difficult to diagnose (59%); they were not diagnosed due to social rejection (27%), interfered quite a lot with daily life (49%) or prevented a normal life (42%), and the effective treatments are psychological (72%). Beliefs were: social rejection, family burden, and patient suffering. Concerns included: dangerousness, social rejection, lack of information, and scarcity of resources.
ConclusionsThere is a lack of knowledge of the symptoms. The majority do not know about specific symptoms and highlight the negative ones. Combined pharmacological–psychological treatment is believed to be most effective. Social stigma and family and personal burden are concerns.
Conocer las opiniones, creencias y preocupaciones de la población general sobre dos enfermedades mentales graves: esquizofrenia y trastorno bipolar.
Material y métodosSe construyó un cuestionario ad-hoc para encuesta. Un panel de siete expertos extrajo los contenidos. También participaron: ASAENES, ABBA, FEAFES-ANDALUCIA, AMAFE, FEMASAM y AFAEM-5. El cuestionario contenía 12 preguntas sobre: conocimiento de las patologías, dificultades diagnósticas, síntomas, desencadenantes, interferencia, tratamientos y efectividad, creencias y preocupaciones. Administrado: IV Campaña de Concienciación Social sobre la Enfermedad Mental Grave (Madrid y Sevilla, septiembre - octubre 2009).
ResultadosSe recogieron 5.473 encuestas, 55,8% en Sevilla. El 66,2% de la muestra eran mujeres y la edad media 35 años (DE=14,5). El 82% conocía ambas enfermedades, pero el 51% no conocía ningún síntoma de la esquizofrenia. Otras opiniones destacables: son difíciles de diagnosticar (59%), no se diagnostican por rechazo social (27%), interfieren bastante en la vida cotidiana (49%) o impiden la vida normal (42%), los tratamientos eficaces son psicológicos (82%) y farmacológicos (72%). Las creencias refieren: rechazo social, sobrecarga familiar y sufrimiento del paciente. Las preocupaciones refieren: peligrosidad, rechazo social, falta de información y escasez de recursos.
ConclusionesExiste desconocimiento sobre la sintomatología. La mayoría desconoce síntomas específicos y resalta los negativos. Se atribuye mayor eficacia al tratamiento conjunto psicológico-farmacológico. Preocupan la estigmatización y la sobrecarga familiar y personal.
It is estimated that 38.2% of the European Union population suffers from some form of mental illness each year.1 In agreement with data from the epidemiological project ESEMeD, coordinated by the World Health Organisation, 19.5% of the people surveyed in Spain had a mental disorder at some moment in their lives and 8.4%, in the last 12 months. The most frequent mental disorder was the major depressive episode, with a yearly prevalence of 3.9%.2
Serious mental illnesses encompass various psychiatric diagnoses (including, among others, schizophrenia and bipolar disorder) with some persistence over time. They present serious difficulties in personal and social functioning, reducing the quality of life of the person affected.3 Assistance for those with serious mental disorders requires the integration of different levels of care and different types of intervention with the objective of reaching autonomy, quality of life, personal well-being and social participation on the road to personal recovery. This way, care for a mental illness is not reduced to just controlling the symptoms. It should also confront the different consequential needs. Care for these patients demands the integration of psychopharmacological and psychosocial interventions in a mental health network formed by interdisciplinary teams.4
One of the barriers to patients’ integral recovery is the stigma attached to mental illness that exists in society.5–7 Serious mental illnesses and the people who suffer from them are perceived by the general public with prejudice, while they are really unknown as far as their symptomatology, their evolution and their different treatment options. According to a Eurobarometer study, in the 15 member countries of the European Union in 2003, people with mental health problems were perceived more frequently as not having “the same opportunities in finding work, improving their training or their job position” as the rest of the population has. Of the people surveyed, 87% believed that people with mental illness had fewer possibilities than any other person. This was a much higher index than for people with physical disability (77%), elderly people (71%) and people of an ethnic minority (62%).8 The stigmatisation of people with mental health problems, as a concept, involves 3 principal problems: ignorance (due to little or incorrect knowledge about mental illness), prejudice (fear, anxiety and rejection of patients) and discrimination (in several family, personal and work life aspects).9–11 The role of media in this sense is especially relevant. The Spanish Confederation of Groups for the Mentally Ill and their Families edited a Style Guide on Mental Health and the Media to promote a series of basic principles, which include: increasing social knowledge, fostering a positive vision, facilitating normalising information, dismantling false beliefs, removing mental illness from the journalistic chronicling of events, etc.12
The objective of this study was to survey the Spanish society's opinions and beliefs about serious mental illnesses, especially schizophrenia and bipolar disorder. In addition, the differences in responses were evaluated depending on how the participants knew the illnesses.
Materials and methodsThe first step in elaborating the questionnaire was to select an expert panel to propose pertinent content and to supervise the composition and editing of the questions. The expert panel consisted of 7 members: 3 psychiatric doctors, 1 representative of patients’ associations, 1 expert in research methodology and data analysis, 1 expert in social psychology and 1 expert in clinical medicine.
The first phase of content collection was carried out in a focus group–made up of the expert panel–that discussed the fundamental aspects that should be known by the general population regarding serious mental illnesses. In particular, the following were determined: aetiology, symptomatology, available treatments and beliefs associated with the illnesses. The session was video recorded for later documentation and analysis.
In addition to the content proposed by the expert panel, contributions from the following were also discussed: Seville Association of Families, Friends and People with Serious Mental Disorders (ASAENES in Spanish), Andalusia Bipolar Association (ABBA), Andalusia Federation of Families of People with Mental Illness (FEAFES-ANDALUCÍA), Madrid Association of Friends and Family of People with Schizophrenia (AMAFE), Madrid Federation of Pro Mental Health Associations (FEMASAM) and Family Association of Mental Illnesses “Area 5” (AFAEM-5). The questionnaire proposed was to be short, capable of being completed by attendees of awareness sessions, self-administered and easily answered by a person at any educational level.
The final questionnaire contained 12 questions that related to the reason for knowing the pathologies (1), the difficulties in diagnosing schizophrenia and bipolar disorder (1), characteristic symptoms (2), illness triggers (1), interference of illnesses with daily life (1), current treatments and their effectiveness (1), beliefs associated with treatments (2) and with the pathologies (2) and concerns about these pathologies (1). In addition, sex and age were recorded. The answer format included multiple-choice questions, 3 open-ended questions and 2 questions with an open-ended option.
Before administering the questionnaire to the overall sample, it was piloted in a sample of 8 patients to test comprehension of the language used and of the concepts included, as well as to assure that the questions were not offensive. The expert panel participating in the discussion group endorsed the suggested modifications (Appendix).
The categorical variables were described using absolute and relative frequencies and the continuous variables using the mean and standard deviation. The comparison between response frequencies was performed using the chi-squared statistic, and the relation between responses and categories using Pearson's chi-squared test of independence. Responses to the open-ended questions were evaluated using a semantic reduction process.13,14 The response categories were later compared using statistics for nominal variables. The responses were compared as to the geographical location of those surveyed and as to the reason for knowing the illness to check for bias. All analyses were performed using SPSS software for Windows version 18.
PopulationThe objective population was the general population without restrictions. Two sampling points were established during the fourth Campaign for Social Awareness of Serious Mental Illness, held in Madrid from 21 to 25 September 2009 and in Seville from 5 to 10 October 2009. We used an opportunity sample of convenience, inviting campaign attendees and passers-by in the mall where it was held to participate in the survey. No initial restriction on the number of participants was established. Information collection was carried out in 2 cities of different sizes and geographic areas to assess whether bias existed in information collection that could prohibit generalisation of the results.
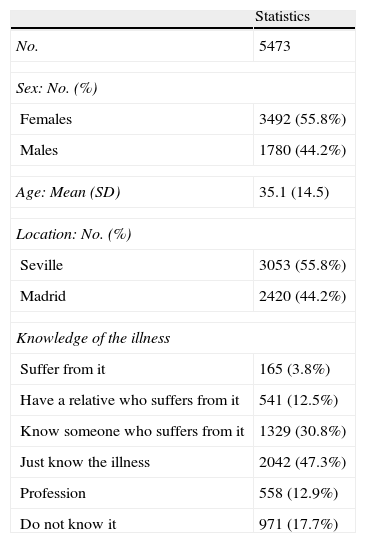
ResultsIn total, 5473 surveys were received, 55.8% from Seville and 44.2% from Madrid. Female participants composed 66.2% of the sample. The mean age was 35 years (SD=14.5), the youngest age recorded being 12 years and the oldest 99 years (Table 1).
Sample description.
| Statistics | |
| No. | 5473 |
| Sex: No. (%) | |
| Females | 3492 (55.8%) |
| Males | 1780 (44.2%) |
| Age: Mean (SD) | 35.1 (14.5) |
| Location: No. (%) | |
| Seville | 3053 (55.8%) |
| Madrid | 2420 (44.2%) |
| Knowledge of the illness | |
| Suffer from it | 165 (3.8%) |
| Have a relative who suffers from it | 541 (12.5%) |
| Know someone who suffers from it | 1329 (30.8%) |
| Just know the illness | 2042 (47.3%) |
| Profession | 558 (12.9%) |
| Do not know it | 971 (17.7%) |
The sample participation from Seville (55.8%) turned out to be significantly greater than that from Madrid (χ2=73.2; df=1; P<.001). In addition, a greater number of women (69%) participated in the Madrid sample, compared to the 64% who participated in Seville (χ2=17.8; df=1; P<.001). The Seville sample was younger than that of Madrid (t=23.9; df=3872; P<.001), with the mean age in Seville being 30.8 years (SD=11.6) compared to the mean age of 40.5 years (SD=16.1) in Madrid.
Description of the overall sampleOf those surveyed, 82% (n=4487) indicated that they knew about schizophrenia and bipolar disorder. Among them, almost half (47%) reported not knowing anyone with schizophrenia or bipolar disorder, 31% knew about the illness because of someone close with schizophrenia or bipolar disorder, 13% because of their profession, 13% because of a relative suffering from an illness and only 4% because they had suffered schizophrenia or bipolar disorder themselves.
Of those surveyed, 58% (n=3174) considered these pathologies to be difficult for a doctor to diagnose. From the list of difficulties, most participants (69%) believed that this was due to ignorance on behalf of the patients themselves and their families. In addition, 46% of those surveyed believed that it was due to social rejection that causes the patient not to go to a doctor. A fourth of participants (26%) thought that the symptoms were not clear enough for a diagnosis, 16% thought that there were no tools to help a physician correctly identify these illnesses and 15% that the diagnostic difficulty was in the difficulty itself of accessing the health system.
Of those surveyed, 45.5% (n=2463) were unable to put forward any symptoms of schizophrenia and, additionally, 5.5% admitted not knowing any, making a total of 51%. The symptom most mentioned was the presence of hallucinations (12.5% of participants), with special mention of auditory hallucinations. The second most mentioned symptom was aggressive and violent behaviour (9.7%), followed by personality changes (6.2%), mood changes (4%), attacks or crises (2%), paranoia or feelings of persecution (4.6%), delirium (3%) and nervousness or stress (3.3%). To a lesser extent, participants also mentioned mania and obsessions (1.2%), loss of control (0.9%), irritability (0.8%), cognitive or thought disturbance (0.7%), amnesia of experienced situations (0.5%), apathy (0.4%) and depression (0.8%).
In the case of bipolar disorder, 60.5% (n=3311) of those surveyed were not able to indicate any symptoms. The symptoms most mentioned were frequent mood changes in the form of highs and lows (12.8% of participants), abrupt changes in personality (7.2%), mood swings (8.7%), split personality (4.5%) or some of the individual phases of mood swings: euphoria (0.6%), depression (1.3%) or apathy (0.3%).
More than two-thirds of those surveyed (68%, n=3271) believed that one of the triggering causes of schizophrenia or bipolar disorder was a change in brain biology. Almost half (45%) also believed that genetics was another trigger. In addition, almost half (45%) believed that the reason could be drug use. To a lesser extent, stress (28%), child trauma (27%), a problem in birth or pregnancy (10%) and infection (4%) were also mentioned. Of those surveyed, 33% selected only 1 response option, compared to 49% who selected 2 or 3 responses.
The great majority of those surveyed (91%) were of the opinion that serious mental illnesses interfere considerably (42%) or interfere enough that they inhibit normal life (49%). Only 9% thought that they interfered somewhat and 3% thought that they did not interfere at all (Fig. 1).
In response to the question about daily life activities that can be performed normally despite illness (provided with a list of activities), 64% of those surveyed thought that family relations were not affected, 55% thought that daily tasks were not affected and 40% that relationships with friends could be managed normally. On the contrary, only 28% of those surveyed thought that patients could handle relationships or planning their free time (33%). Some participants also believed patient independence (34%) and working without interference (36%) to be possible.
Concerning useful treatments for managing illnesses, 81% of those surveyed selected psychological treatment, compared to the 72% who selected treatment with drugs. Almost half selected a combination of the two strategies (45%).
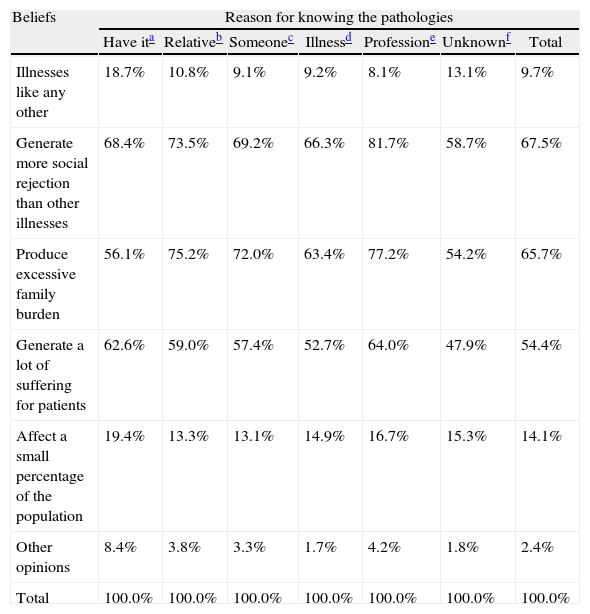
From the list offered of beliefs normally associated with these illnesses, more than two-thirds of those surveyed (68%) thought that schizophrenia and bipolar disorder were illnesses that generate more social rejection than others and 66% declared them to be illnesses that generate family burden. In addition, more than half of those surveyed (55%) believed that they generate considerable suffering for the patients. Only 10% believed that they were illnesses like any other. Furthermore, 3% expressed additional written opinions. The aspects mentioned were dangerousness (0.2%) and aggression (0.1%), excessive family burden (0.3%), fear of illness (0.2%) and patients’ unawareness of themselves (0.2%).
Regarding beliefs associated with treatments, more than three-quarters (78%) believed that treatment for these illnesses should last a lifetime, 61% thought that ceasing treatment could be harmful for the patient and 15% thought that these illnesses should only be treated when symptoms are present, leading to the perception that continuous treatment is necessary. Barely 7% of those surveyed believed treatment to be simple and comfortable, and 10% thought that prolonged treatment could be harmful.
Regarding participants’ concerns about these illnesses, 45.4% answered the question. Drawing from the content of the free responses, the most frequent was the dangerousness of the illnesses (5%), be it violent behaviour, aggression or harm in which it might involve other people. Also mentioned were ignorance of these illnesses (on the part of both society and families) and the lack of information (4%), an issue that is usually associated with not knowing how to help someone affected and also with social rejection of those affected (4.2%). A more serious level of rejection mentioned frequently was the stigmatisation of illness (0.5%) and the socio-labour marginalisation of patients (1.9%). Under the concept of resource availability, the scarcity of centres, the lack of specialised care, the difficulty in accessing treatment and the need for more healthcare were especially mentioned. Closely linked to this idea was the demand for better institutional support (1%), the complaint of inadequate treatment for patients (3.3%), including inadequate follow-up, the demand for specialised psychological treatment and non-pharmacological therapies, the need for more research (1%) and the provision of family support (1.1%).
From the patients’ point of view, some concerns were raised, such as the characteristic symptoms of these illnesses (1.1%), the patients’ suffering (2.2%), the loss of control from which many patients suffer (0.7%) and isolation (0.4%). In addition, the demand for patient support (0.4%), social support (0.2%), greater illness acceptance by society (0.2%) and patient acceptance (0.4%) were expressed. Also mentioned were denial of the illness by the patient and his/her family (0.8%), family rejection of patients (0.1%) and family problems with the caregiver (2 responses). In addition, participants mentioned the excessive family burden that taking care of the patients or living with them entails (2.6%), concerns of possibly suffering from the illness, concerns about the patients’ future without their family (0.5%), dependence, disability or lack of autonomy in leading a normal life (0.5%), the perception that there is an increase in prevalence (0.5%), the mere existence of the illness itself (0.5%), the need for better legal coverage (0.1%) or even committal in some cases (0.2%).
Comparison of reason for knowing the illnessesThe degree of interference of schizophrenia and bipolar disorder with a patient's normal life significantly differed according to the reason given for knowing the illness (χ2=123.2; df=18; P<.001). Using the response categories of perceived interference of an illness in an ordinal scale (1=No, they do not interfere at all; 4=They interfere enough to greatly inhibit normal life), the highest level of interference was perceived by professionals (mean=3.35) and family members (3.32), compared to those who suffer from an illness (3.01).
Regarding daily life activities that participants thought patients could perform normally, selections differed significantly according to the reason for knowing the pathologies (χ2=803.4; df=42; P<.001). The group that differed the most from the rest was the group that knew the illnesses through their profession. In this group, the frequency of selecting activities that can be performed normally was higher than the overall profile and the selections of other groups, especially (concerning the other groups) daily tasks (76.4%). The group of people who know the pathologies, because they suffer from them, stood out in their selection of relations with family (70%), relations with friends (50%) and planning leisure time (41.3%), but they selected daily tasks with less frequency overall (50.7%). Those who have a family member with an illness also selected more activities overall, reflecting that they believe that there is little limitation. This profile is similar to that of those who know someone who suffers from one of these illnesses.
The different beliefs associated with the illnesses were established significantly differently depending on the reason for knowing the pathologies (χ2=435.6; df=36; P<.001) (Table 2). The group of participants with an illness selected, more frequently than the overall percentage, the fact that these illnesses are like any other (18.7%, overall=9.7%) and they selected, less frequently than the overall percentage that they produce excessive family burden (56.1%, overall=65.7%), as occurred among others ignorant of the illnesses (13.1% and 54.2% respectively). In addition, the group of patients selected, higher than the overall percentage that these illnesses generate more social rejection than others (68.4%, overall=67.5%) and they generate considerable suffering for those with them (62.6%, overall=54.4%). In addition, the group of patients selected, with relatively more frequency that these diseases affect a small percentage of the population (19.4%, overall=14.1%). The professionals were those who most selected that illnesses produce an excessive family burden (77.2%), which coincides with what family members thought (75.2%). Professionals and families noted, above the overall percentage that these illnesses generate more social rejection than others (81.7% and 73.5% respectively) and that they generate considerable suffering for patients (64% and 59%). Professionals and families differ in their perception of such illnesses being like any other, with reduced selection on behalf of professionals (8.1%) and increased selection on behalf of families (10.8%); this pattern is inverted regarding the opinion that these illnesses are not prevalent.
Beliefs about serious mental illnesses by reason for knowledge of them (% column).
| Beliefs | Reason for knowing the pathologies | ||||||
| Have ita | Relativeb | Someonec | Illnessd | Professione | Unknownf | Total | |
| Illnesses like any other | 18.7% | 10.8% | 9.1% | 9.2% | 8.1% | 13.1% | 9.7% |
| Generate more social rejection than other illnesses | 68.4% | 73.5% | 69.2% | 66.3% | 81.7% | 58.7% | 67.5% |
| Produce excessive family burden | 56.1% | 75.2% | 72.0% | 63.4% | 77.2% | 54.2% | 65.7% |
| Generate a lot of suffering for patients | 62.6% | 59.0% | 57.4% | 52.7% | 64.0% | 47.9% | 54.4% |
| Affect a small percentage of the population | 19.4% | 13.3% | 13.1% | 14.9% | 16.7% | 15.3% | 14.1% |
| Other opinions | 8.4% | 3.8% | 3.3% | 1.7% | 4.2% | 1.8% | 2.4% |
| Total | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% |
In general, the questionnaire in the survey was well-accepted, easily answered and requiring little time. Forming the questions in a positive sense and trying to avoid a stigmatising vision of the illnesses did not seem to obscure the responses, of which the vast majority were quality responses. The questionnaire turned out to be easy to answer and generated extremely few blank responses, which were not due to ignorance.
As a limitation of the study, it should be mentioned that it was not possible to confirm whether those that claimed to suffer from an illness really suffered from it, given that the method of gathering information did not allow performing a diagnosis for case classification. It should not be forgotten that the opportunity sampling method used did not let us ensure that the sample was representative of the population. In addition, it should be considered that, as 2 cities were selected to carry out the survey, the greatest bias attributable lies in the under-representation of rural areas.
More than three-quarters of those surveyed claimed to know both illnesses (schizophrenia and bipolar disorder). However, 51% did not know any symptoms of schizophrenia and 61% did not know any symptoms of bipolar disorder. This leads us to think that such knowledge was not real, and that in reality the response to this question should be interpreted in a colloquial sense of having heard of the illnesses.
The symptoms most frequently associated with schizophrenia were hallucinations, aggression and violent behaviour. The symptoms of bipolar disorder mentioned most were abrupt changes in personality, mood changes, split personality and individual phases of mood changes: euphoria, depression or apathy. This leads us to think that the general population perceives both illnesses in a differentiated way.
Violence is one of the principal stereotypes related to mental illness in general, and to schizophrenia in particular.15 The association between mental illness and violence is present in studies of perception and stigma in populations in Europe, Latin America, Asia and Africa.16–19 In many cases this association is reinforced by the continuous appearance of violent acts committed by a patient with a mental illness in the media.12,15 This perception leads to the perpetuation of stigmatising and discriminatory practices against people with serious mental disorders. Unfortunately, the media do not report that violent acts attributable to mental pathology are very unusual in relation to the violence of society in general.
More than half of those surveyed believed that these illnesses are not easy to diagnose and 40% believed that even patients and families are ignorant of them. In addition, one-fourth believed that doctors are not sought out due to fear of social rejection and that patients thus hide their suffering. These 3 fundamental ideas are revealed constantly in the responses to the remaining questions, leading to a pejorative vision of the illnesses and those that suffer from them.
Alteration in brain biology, genetics and drug use were appropriately recognised as triggers for these illnesses.
It is assessed that these illnesses interfere considerably in daily life or even impede normal life. However, it was also thought that they permit normal achievement of family relations, daily tasks and relations with friends. The functional abilities mentioned by those surveyed coincide with those used habitually for evaluation of functionality in scales like WHO-DAS II20 for any type of patient or the Personal and Social Performance (PSP) scale21 for schizophrenia: self-care, personal and social relations, habitual social activities and abnormal or aggressive behaviours. They also coincide with the indicators of excessive burden found in previous studies22 and all of them have been considered in evaluating the benefit of psychoeducational interventions in patients’ families.23
Both psychological and pharmacological treatments are perceived as useful, and most thought that these were effective or totally effective. The majority believed that treatment should last a lifetime and that ceasing treatment could be harmful. However, a subgroup of people surveyed thought that patients should only be treated if they present symptoms that a very prolonged treatment could be harmful and that treatment was simple and comfortable.
The most deeply rooted beliefs were that these illnesses generate a lot of social rejection, excessive family burden and patient suffering. The concerns mentioned with greatest frequency were dangerousness, social rejection, lack of information, scarcity of resources and excessive family burden.
It is interesting to note that those who suffered from an illness perceived much less interference of the illness in daily life (even though this group also scored higher than the mean on the scale). Professionals and families were groups that perceived a greater level of interference. This result could be explained by the tendency of patients to minimise their clinical situation and to adjust to their personal situation. This result might also be due to a certain reduction in the patients’ introspective capacities.
ConclusionsThere is an ignorance of symptomatology of schizophrenia and bipolar disorder. Practically half of those surveyed did not know specific symptoms, and those who knew some of the symptoms emphasised that those are harmful to others. The difficulty in their diagnoses is due to this ignorance and social rejection. The limitation in quality of life is not experienced equally in all areas of daily life. Preferentially, psychological treatment in conjunction with pharmacological treatment was perceived as the most effective. Treatment should be continuous, chronic and present even in the absence of symptoms. The most frequent concerns were stigmatisation and excessive burden, both for the family and the patient. Also mentioned were the need to have better information, to consider them as common illnesses and to make autonomy possible for those who suffer from them.
Ethical responsibilitiesHuman and animal protection. The authors declare that no experiments were performed on humans or animals for this study.
Data confidentiality. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
FundingThe study was funded by the AstraZeneca Foundation.
Conflict of interestsMiguel Ángel Ruiz has participated in research projects subsidised by the Autonomous University of Madrid Foundation with the following laboratories: Abbott, AstraZeneca, Knoll, Medtronic, Pfizer, Roche and Eli Lilly. José Manuel Montes has received research grants from, has participated in clinical trials for or has collected fees for presenting at conferences of the following laboratories: AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb-Otsuka, Lundbeck, Pfizer, Rovi and Servier. Consuelo de Dios has received research grants from, participated in clinical trials for or has collected fees for presenting at conferences of the following laboratories: Almirall, AstraZeneca, Bristol-Myers Squibb-Otsuka, Eli Lilly, GlaxoSmithKline, Janssen-Cilag, Lundbeck, Pfizer, Sanofi-Aventis, Servier and Wyeth. Javier Correas Lauffer has received research grants from, participated in clinical trials for and has collected fees for both his advisory work and presenting at conferences of the following laboratories: Almirall, AstraZeneca, Bristol-Myers Squibb-Otsuka, Boehringer Ingelheim, Eli Lilly, Janssen-Cilag, Lilly, Lundbeck and Servier. Cristina Álvarez and Jorge Mauriño are full-time employees of AstraZeneca Pharmaceuticals, Spain, S.A.
Please cite this article as: Ruiz MÁ, et al. Opiniones y creencias sobre las enfermedades mentales graves (esquizofrenia y trastorno bipolar) en la sociedad española. Rev Psiquiatr Salud Ment (Barc). 2012;5:98–106.