Several studies have shown that patients with persistent or severe mental illness are at increased risk for obesity, both from the illness itself and from its treatment. Nevertheless, obesity in these patients could be related to other sociodemographic, psychosocial, and genetic factors.
AimTo explore whether obesity and other physical comorbidities, are more prevalent in long-term psychiatric outpatients as compare to standard population.
DesignCross-sectional study in a rural Community Mental Health Setting, comparing physical and demographic data from psychiatric outpatients with data from the general population of the region, controlling for age, gender, body mass index (BMI) and physical comorbidity.
ResultsPsychiatric patients were older, with higher BMIs and more chronic diseases. They are more frequently diagnosed with hypertension and hyperlipidemia. However, obesity is related to age, gender and comorbidity, but not to the presence or absence of psychiatric illnesses.
ConclusionsPsychiatric patients are more obese than the general population, but it might be related to physical and demographic correlates: age, chronic illness and lifestyle. These factors can be also responsible for their increased risk of hypertension and hyperlipidemia. All those factors could be more relevant than the presence of mental illness itself or its treatment.
Diversos estudios han demostrado que los pacientes con una enfermedad mental persistente o grave presentan un mayor riesgo de obesidad, tanto como consecuencia de la enfermedad en sí como a causa de su tratamiento. No obstante, la obesidad de estos pacientes podría estar relacionada con otros factores sociodemográficos, psicosociales y genéticos.
ObjetivoExplorar si la obesidad y otras comorbilidades físicas tienen una mayor prevalencia en pacientes ambulatorios psiquiátricos de larga evolución, en comparación con la población general.
DiseñoEstudio transversal en un contexto de Salud Mental Comunitaria rural, comparando los datos físicos y demográficos de pacientes ambulatorios psiquiátricos con los de la población general de la región e introduciendo un control respecto a edad, sexo, índice de masa corporal (IMC) y comorbilidad física.
ResultadosLos pacientes psiquiátricos eran de mayor edad y tenían valores superiores de IMC y más enfermedades crónicas. Se les diagnostica con mayor frecuencia hipertensión e hiperlipemia. Sin embargo, la obesidad está relacionada con la edad, el sexo y la comorbilidad, pero no con la presencia o ausencia de enfermedades psiquiátricas.
ConclusionesLos pacientes psiquiátricos son más obesos que los individuos de la población general, pero esto podría estar relacionado con factores físicos y demográficos: edad, enfermedad crónica y estilo de vida. Dichos factores también pueden ser la causa del aumento del riesgo de hipertensión e hiperlipemia. Todos estos factores podrían ser más relevantes que la presencia de la enfermedad mental en sí o su tratamiento.
Obesity and psychiatric disorders are increasing in prevalence and are associated with a variety of health complications. Multiple studies have shown that people with severe mental illness represent a vulnerable population—at risk for various medical conditions1–4 and among whom mortality rates are very high5–7 or life expectancy is much lower than that seen in the general population.8,9 As health problems, overweight and obesity are common in the general population and causes for growing concern in clinic populations—especially those patients with severe mental illness. Several recent studies indicate that patients with persistent or severe psychiatric disorders are more likely than the general population to be obese.10,11 There are also various articles on research into the risk of depression and other psychiatric disorders, with obese individuals as the index population12–15; these report a weak correlation between obesity and the risk of depression. At any rate, the general conclusion from these studies is that further research on this issue is needed.
The connection between obesity and physical and psychiatric disorders is widely debated. There is general agreement about an association, but the key issue is whether psychiatric patients are more obese and have more physical comorbidities—there being a causal relationship with their psychiatric problems—or whether certain physical disorders and obesity, in and of themselves, predispose to psychiatric disorders. This article is oriented towards analysing another dimension or hypothesis, actually: that obesity and other physical problems are indeed associated with psychiatric disorders but that this association is not causal but rather related to other demographic and population characteristics of these patients.
Materials and methodsContextThe Canary Islands are a Spanish archipelago made up of 7 islands located just off the northwest coast of Africa; they constitute an autonomous region of Spain that has full responsibility for healthcare. The archipelago has more than 2 million inhabitants, 85% of whom live on the main islands of Tenerife and Gran Canaria while the remaining 15% of its citizens are scattered among the other 5 islands. The population of the island of La Gomera is about 20,000, and it has a 35-bed hospital, 5 primary care centres, and 15 general practice physicians who render services to 100% of the population. All primary care medical records are digitized, and there are community programs for diabetes, hypertension, hypercholesterolemia, obesity, smoking, as well as routine screening for breast cancer and osteoporosis, which operate on a regular basis. There is a small private sector within the healthcare realm, with 1–2 doctors in private practice.
The Mental Health Centre team on the island of La Gomera consists of 1 consulting psychiatrist (who works in person on Mondays and via tele-psychiatry the rest of the week), 2 clinical psychologists (1 full-time and 1 part-time), 1 nurse, 1 social assistant, and 2 nurses aides. The source of mental health consults is referrals from the primary care doctors in general practice. Professionals from mental health and primary care collaborate closely within a partially integrated system (electronic medical records, lab tests, scheduling, and data entry), having ongoing personal interactions regarding patients, joint consults, coordinated treatment plans for complicated cases, and their shared allegiance to a biopsychosocial/systems paradigm.
Study populationAll adult, outpatient, psychiatric patients who had suffered at least 2 episodes of a psychiatric disorder and had been followed on a regular basis for more than 3 years at the Mental Health Centre on the island of La Gomera were invited to participate in the study between January and December of 2008. Having received a detailed explanation of the study, each patient signed an informed consent form that had been approved by the local Ethics Committee.
Information on the controls was obtained from the Canary Islands Health Survey [Encuesta de Salud de las Islas Canarias16 (ESIC)] conducted in 2004. The health survey is organized and monitored entirely by regional health department officials and is available upon request.12 A total of 5633 individuals were recruited, constituting a representative random sample of the diversity of the Canary Islands population, through a multistage stratified cluster design. In the first stage, the 180 census sections for the Canary Islands territory were set up as clusters. The stratification criteria for selecting the clusters were the number of inhabitants and the socio-economic conditions in each census section. In the second stage, for the homes selected in each census section, an individual over 16 years of age (if present) was randomly chosen. All individuals gave their informed consent prior to completing the survey. From the survey, 4223 individuals at least 18 years of age were selected for this study. However, the information from only 3327 individuals could be used; the rest did not respond or had a psychiatric disorder.
Evaluation parametersBMIThe research team used ordinary primary care scales and height measurements to determine height and weight for each outpatient psychiatric patient in the sample. The body mass index (BMI) was calculated using the following formula: weight in kg/(height in metres).2 According to WHO classification guidelines for overweight and obesity, participants were classified as low or normal weight (BMI<25), overweight (25≤BMI<30), or obese (BMI≥30). For the controls taken from the Canary Islands Health Survey, BMI was estimated using the height and weight information provided on the survey itself.
Demographic variables and comorbidityTo diagnose lifelong physical health problems, each patient was interviewed by his/her psychiatrist to determine whether there were any medical conditions, and primary care medical records were analysed to uncover possible comorbidity.
Information was obtained on comorbidity in the 12 months prior to the Canary Islands Health Survey relative to physician-diagnosed chronic diseases, such as osteomuscular disease, cardiovascular disease, cancer in general, hypertension, diabetes, migraines, gastrointestinal disease, hyperlipidemia, allergies, varices/varicose veins, chronic lung disease/asthma, and obesity.
Two demographic variables—sex and age—were used as covariables for the analysis, with stratification into 2 groups, depending on the statistical results, and a cut-off value of 65 years of age. Smoker status was also included in the analysis.
Analysis of the dataAll phenotype information, gleaned from the interviews and surveys, was coded by assigning a number to each participant and eliminating all personally identifiable information. To perform the statistical analyses, the information was first entered into a data file created with the program Statistical Procedures for the Social Sciences (SPSS), version 17 for Windows.
Analysis of simple contingency tables was used to compare the groups in terms of the lifelong incidence of different physical health problems. Each comorbidity, showing a significant association, was entered into a multivariable logistic regression model. Cofactors such as age, sex, and obesity that showed significant association were used in the final regression model. P values were adjusted using the Bonferroni correction for multiple tests. A multivariable logistic regression model was also used to explore the association between psychiatric illness and overweight. Relevant covariables having an association were used to introduce an adjustment for them into the final regression model (age, sex, smoker status, and number of chronic diseases).
ResultsA total of 201 psychiatric outpatients from La Gomera were included in the study, along with 3327 mentally healthy controls from the general population. None of the patients refused to participate in the study, once they had received adequate information and the assurance that individual results would be completely confidential. Depressive disorders (40.8%) and anxiety disorders (33.3%) were the diagnoses most prevalent among the psychiatric outpatients, followed by schizophrenia spectrum disorders (20.4%), personality disorders (3%), and other diagnoses (2.5%). The mean number of psychotropic drugs taken by the patients was 1.85±0.9 (range, 0–5). Only 32.7% of the patients were receiving monotherapy treatment, while 50.2% were taking 2 drugs, 11.4% were taking 3 drugs, and 4.5% were taking 4 drugs or more. The most common medication was the benzodiazepine tranquillisers, taken by 65.7% of the patients, followed by SNRI antidepressants taken by 35.8%; atypical antipsychotics, 23.4%; SSRI antidepressants, 22.9%; mood stabilizers, 11.4%; conventional antipsychotics, 10.4%; anticholinergics, 3.5%; and tricyclic antidepressants, 2%. All patients were receiving cognitive behaviour therapy from their psychiatrist in conjunction with the pharmacotherapy.
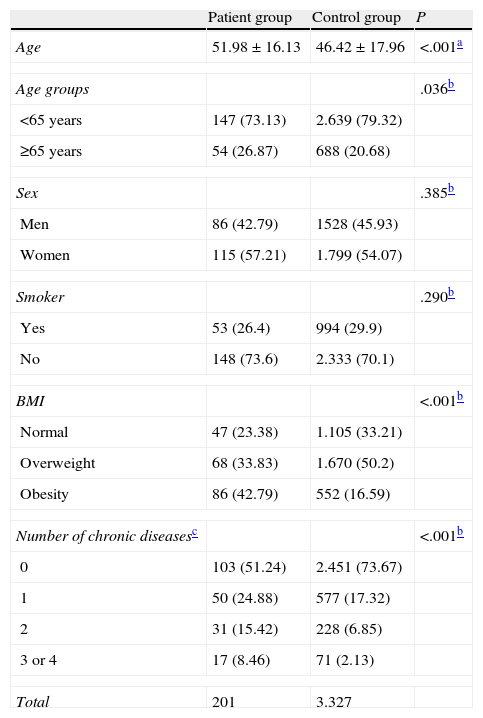
Table 1 shows distribution of the demographic variables, distribution of the BMI, and the number of chronic diseases. There were no statistically significant differences between the groups in terms of the distribution by sex and smoker status. At the time of the interview, the mean age was 51.98 years for the patients and 46.42 years for the controls (P<.001). Because this difference was significant, a control for age was introduced into all comparisons for medical conditions.
Characteristics of the reference population and the sample.
| Patient group | Control group | P | |
| Age | 51.98±16.13 | 46.42±17.96 | <.001a |
| Age groups | .036b | ||
| <65 years | 147 (73.13) | 2.639 (79.32) | |
| ≥65 years | 54 (26.87) | 688 (20.68) | |
| Sex | .385b | ||
| Men | 86 (42.79) | 1528 (45.93) | |
| Women | 115 (57.21) | 1.799 (54.07) | |
| Smoker | .290b | ||
| Yes | 53 (26.4) | 994 (29.9) | |
| No | 148 (73.6) | 2.333 (70.1) | |
| BMI | <.001b | ||
| Normal | 47 (23.38) | 1.105 (33.21) | |
| Overweight | 68 (33.83) | 1.670 (50.2) | |
| Obesity | 86 (42.79) | 552 (16.59) | |
| Number of chronic diseasesc | <.001b | ||
| 0 | 103 (51.24) | 2.451 (73.67) | |
| 1 | 50 (24.88) | 577 (17.32) | |
| 2 | 31 (15.42) | 228 (6.85) | |
| 3 or 4 | 17 (8.46) | 71 (2.13) | |
| Total | 201 | 3.327 | |
The data express n (%) or mean±standard deviation.
In terms of weight, 23% of patients and 33% of controls were normal; 34% of patients and 50% of controls were overweight; and 43% of patients and 17% of controls had body weight in the obesity range. These differences were statistically significant (P<.001).
One-fourth of the psychiatric outpatients and 9% of individuals in the control group had 2 or more chronic diseases. There was a significant difference between the 2 groups (P<.001) in terms of distribution of the number of chronic diseases.
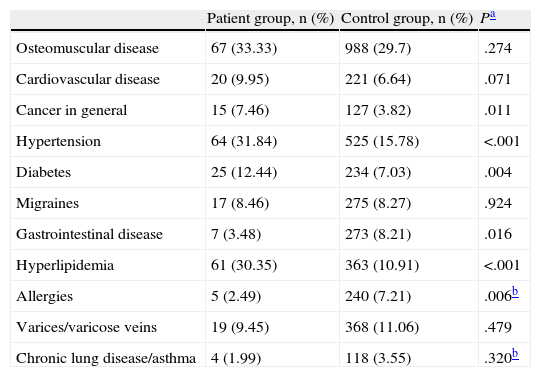
The lifelong incidence of common medical conditions for the patient and control groups is shown in Table 2. The patient group had the highest lifelong incidence for osteomuscular disease, cardiovascular disease, migraines, cancer, hypertension, diabetes, and hyperlipidemia, though only for the last 4 conditions listed was the incidence significantly higher in the patient group than in the control group.
Lifelong incidence of medical conditions in the outpatient sample.
| Patient group, n (%) | Control group, n (%) | Pa | |
| Osteomuscular disease | 67 (33.33) | 988 (29.7) | .274 |
| Cardiovascular disease | 20 (9.95) | 221 (6.64) | .071 |
| Cancer in general | 15 (7.46) | 127 (3.82) | .011 |
| Hypertension | 64 (31.84) | 525 (15.78) | <.001 |
| Diabetes | 25 (12.44) | 234 (7.03) | .004 |
| Migraines | 17 (8.46) | 275 (8.27) | .924 |
| Gastrointestinal disease | 7 (3.48) | 273 (8.21) | .016 |
| Hyperlipidemia | 61 (30.35) | 363 (10.91) | <.001 |
| Allergies | 5 (2.49) | 240 (7.21) | .006b |
| Varices/varicose veins | 19 (9.45) | 368 (11.06) | .479 |
| Chronic lung disease/asthma | 4 (1.99) | 118 (3.55) | .320b |
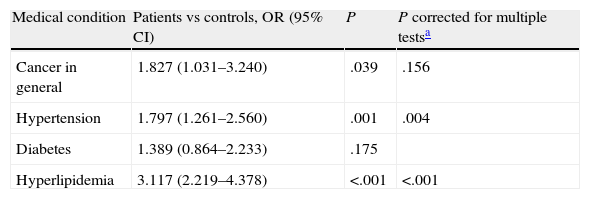
Table 3 shows the odds ratio values, 95% confidence intervals, and statistical significance for the multivariable logistic regression (4 regressions are done in Table 3) for each medical condition where a significant difference was seen between patients and controls (Table 2). The presence or absence of the condition was the evaluation variable or result, and the cofactors were the individual's group (patient or control), BMI (low or normal weight, overweight, and obesity), sex, smoker status, and age group (under 65 years or at least 65 years). The odds ratio values for hypertension and hyperlipidemia were the only ones that remained significant after the Bonferroni correction was applied. After an adjustment for other covariables was introduced, psychiatric outpatients had a 79% higher probability of having hypertension and were more than 3 times more likely to have hyperlipidemia than individuals who have no psychiatric illness.
Multiple binary logistic regression, with the presence or absence of each medical condition as evaluation variable, and with patient v. control, BMI, sex, age, and smoker status as cofactors.
| Medical condition | Patients vs controls, OR (95% CI) | P | P corrected for multiple testsa |
| Cancer in general | 1.827 (1.031–3.240) | .039 | .156 |
| Hypertension | 1.797 (1.261–2.560) | .001 | .004 |
| Diabetes | 1.389 (0.864–2.233) | .175 | |
| Hyperlipidemia | 3.117 (2.219–4.378) | <.001 | <.001 |
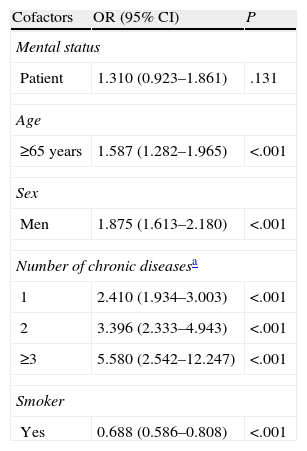
With (1) the presence of obesity as the evaluation variable, (2) an adjustment for the presence of mental illness, and (3) the number of significant chronic diseases, sex, smoker status, and age (<65 or ≥65 years) as cofactors, the multivariable logistic regression model (Table 4) showed no statistically significant association between obesity—measured dichotomously using the BMI (presence of an obesity problem)—and mental health, while all the other cofactors were associated with obesity.
Multiple binary logistic regression, with the presence or absence of an obesity problem as evaluation variable, and with patient v. control, number of chronic diseases, sex, age, and smoker status as cofactors.
| Cofactors | OR (95% CI) | P |
| Mental status | ||
| Patient | 1.310 (0.923–1.861) | .131 |
| Age | ||
| ≥65 years | 1.587 (1.282–1.965) | <.001 |
| Sex | ||
| Men | 1.875 (1.613–2.180) | <.001 |
| Number of chronic diseasesa | ||
| 1 | 2.410 (1.934–3.003) | <.001 |
| 2 | 3.396 (2.333–4.943) | <.001 |
| ≥3 | 5.580 (2.542–12.247) | <.001 |
| Smoker | ||
| Yes | 0.688 (0.586–0.808) | <.001 |
Reference category: mental status=control; age ≥65 years; sex=female; number of chronic diseases=absence; smoker status=non-smoker.
In conclusion, there is no causal association between obesity and psychiatric disorders, and only the higher incidence of hypertension and hyperlipidemia shows a statistically significant association with patients who have psychiatric disorders.
DiscussionThe results of previous research on the physical health of individuals with mental illness indicate that there is high morbidity and mortality from certain physical illnesses in individuals with long-standing mental illness. Risk factors related to lifestyle (smoking, inappropriate consumption of alcohol and drugs, lack of exercise, obesity, and improper diet), psychotropic medication, and inadequate care of physical health have been described as contributing to the poor physical health of individuals with mental illness.1,2
Researching the physical health of psychiatric outpatients is inherently complicated, as the many studies published show and as is appreciated in this study. The validity of most diagnostic categories in psychiatry has not been demonstrated, for they are not discrete entities that have natural boundaries separating them from other disorders.17 Among the main criteria for validating a psychiatric diagnosis is its stability over time.18 Nowadays, however, there can be major fluctuations in the stability of the diagnostic, as well as changes in the way it manifests clinically.19 Changes in the psychiatric diagnosis over time may reflect the progression of an illness, the appearance of new information, or low reliability of the measurements taken.20 The inconsistency of mental disorders over time is a problem with our current psychiatric diagnosis procedures. Current diagnostic systems, such as the DSM-IV21 and the ICD-10,22 also foment the diagnosis of comorbid disorders.
Polypharmacy—the concomitant use of multiple psychoactive medications in an individual patient—is an increasingly common and debatable practice in clinical psychiatry23,24 that must be taken into account, as well. There is also some confusion as to the classification of psychiatric drugs, for there are no standard criteria by which any given drug is assigned to a group of substances, and medications are grouped arbitrarily into several classes that do not always reflect the degree to which they resemble each other pharmacologically. How a drug is classified may depend on its basic pharmaceutical structure, its mechanism of action, its pharmacological effects, and the subjective intention of the person administering it. In addition, there are also many medications that have been approved for different indications.
Besides these basic difficulties, this study had several limitations relative to the control group. Although based on a well-designed health survey, the information supplied by the surveys themselves was limited to a few disorders and was not validated. The fact that it was based on the disorders listed on the survey may mean that estimates of incidence are biased, especially in the case of individuals who have a lower level of education and are in unfavourable socio-economic circumstances. There is also the possibility that individuals were erroneously classified on the basis of BMI because overweight individuals are more likely to state a figure less than their actual weight.25,26
Despite the limitations described, the results of this study are significant. In our study, outpatients with long-standing psychiatric disorders had a higher incidence of overweight and obesity and suffered more chronic diseases than individuals in the control group. In any event, it seems that this occurs with certain health conditions, in particular: apparently, osteomuscular disease, cardiovascular disease, migraines, and chronic lung disease are not associated with chronic psychiatric disorders, while hypertension, hyperlipidemia, cancer, and probably also diabetes appear to be related to psychiatric comorbidity. After introducing a control for patients/controls, BMI, sex, and age, only hypertension and hyperlipidemia showed a clear association with the psychiatric patients. It appears that other comorbidities are not directly related to the diagnosis of a mental disorder.
Previous studies indicate that patients with persistent or severe mental illness are at increased risk for obesity because of the illness itself as well as its treatment.27 The minor affective disorders—not easily identified—such as hypomanic symptoms or abnormal temperament14,15 have also been considered obesity risk factors. However, our results do not go in the same direction. Table 4 sheds some light on the interpretation of our results. Although it appears that the patients have a higher BMI and more chronic diseases, when a control for obesity is introduced into the sample as a whole, then obesity is seen to be related to age, sex, and the number of chronic physical conditions—not to the presence of a psychiatric illness. When all these data are correlated, the hypertension and hyperlipidemia diagnoses, which appear to be more common in the psychiatric patients (Table 3), could also be related not only to the psychiatric illness itself or its treatment but also to the demographic characteristics and lifestyle of these patients.
Hypertension and hyperlipidemia are associated with the modifiable risk factors of lifestyle and unhealthy diet—elements that are typically altered in psychiatric patients, who tend to have a more sedentary lifestyle and whose eating habits are affected by a lack of emotional well-being. Diabetes is probably related to poor eating habits, and the higher incidence of cancer may be related to the emotional impact of the diagnosis, for which psychiatric care has been requested. This study was unable to differentiate between the role of the illness itself and the role of the psychotropic drugs used because of the high degree of comorbidity and existing polypharmacy as well as the fact that there are no clear patterns of association between the hypertension and hyperlipidemia and the drugs that were most frequently used.
There are many factors that could make a psychiatric patient more susceptible to obesity and vice versa. These factors have not yet been studied in detail, but there are multiple influences in both directions rather than a single pattern of association.28
Given a scenario of proper access to primary healthcare—with population-wide prevention programs and a specific framework of reference for chronic psychiatric illness that has special emphasis on physical health—the higher incidence of hypertension and hyperlipidemia in psychiatric outpatients appears to be related more to their demographic characteristics than to any direct effect of the mental illness or its treatment.
For these reasons, special consideration must be given to diagnosing and properly treating cardiovascular risk factors in patients with long-standing, mild psychiatric disorders.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: De las Cuevas C, et al. ¿Están relacionadas la obesidad y otras comorbilidades físicas con la enfermedad mental? Rev Psiquiatr Salud Ment (Barc.). 2011;4:119–25.