There are few studies that relate eating and nutritional habits to the severity of the disease and demographic profile in patients with schizophrenia.
ObjectiveTo describe eating and nutritional habits and their relationship with the severity of the disease in patients with schizophrenia.
MethodCross-sectional descriptive study. Sample: 31 patients with schizophrenia (ICD-10) under outpatient treatment. Inclusion criteria: age 18–65 years, clinically stable and, written informed consent. Assessment: Demographic, clinical characteristics (CGI-SCH, length of illness, BMI, abdominal perimeter), ad hoc questionnaire (eating, nutritional, and physical activity).
ResultsMean age 43.13(SD = 7.85) years, males 61.3%. Mean severity of illness was 3.94(SD = 1.06), mean duration of the illness 18.42(SD = 8.27) years. 74.2% used to eatweekly fat meat and 64.5% less than 3−4 servings of fish, 77.4% less than 3 servings of fruit per day, and 51.6% drink less than 1 L of water. 83.9% used to drink coffee daily, 2.81(SD = 2.02) cups per day. Patients showed lower levels of Vitamin A, D, E, K1, C, folic acid, and magnesium. 93.5% did not fulfill the WHO recommendations on physical activity. Only retinol (r = −0.602, P = .039) and vitamin K1 (r = −0.693, P = .012) in women were related to the severity of illness.
ConclusionsOutpatients with schizophrenia do not follow WHO recommendations on healthy diets, neither physical activity. Both clinical severity of the illness and marital status and cohabitation were associated with poor eating habits and nutrients deficit. These data should be taken into account by the nursing staff when implementing specific care in routine clinical practice.
Hay pocos estudios que relacionen los hábitos alimenticios y nutricionales con la gravedad de la enfermedad y el perfil demográfico en pacientes con esquizofrenia.
ObjetivoDescribir los hábitos alimenticios y nutricionales y su relación con la gravedad de la enfermedad en pacientes con esquizofrenia.
MétodoEstudio descriptivo transversal. Muestra: 31 pacientes con esquizofrenia (CIE-10) en tratamiento ambulatorio. Criterios de inclusión: edad 18–65 años, clínicamente estable y consentimiento informado por escrito. Evaluación: características demográficas, clínicas (ICG-G, años de evolución de la enfermedad, IMC, perímetro abdominal), cuestionario ad hoc (alimentación, hábito nutricional y actividad física).
ResultadosEdad media 43.13 (D.E = 7.85) años, varones 61.3%. La gravedad media de la enfermedad fue de 3,94 (D.E = 1,06), con una media de 18,42 (D.E = 8,27) años evolución de la enfermedad. El 74.2% comía carne grasa semanalmente y el 64.5% menos de 3−4 porciones de pescado, el 77.4% menos de 3 porciones de fruta por día y el 51.6% bebía menos de 1 litro de agua. El 83.9% tomaba café diariamente, 2.81 (D.E = 2.02) cafés por día. Los pacientes presentaban niveles más bajos de vitamina A, D, E, K1, C, ácido fólico y magnesio. El 93,5% no cumplía con las recomendaciones de la OMS sobre actividad física. Solo el retinol (r = −0.602, P = .039) y la vitamina K1 (r = −0.693, P = .012) en las mujeres se relacionaron con la gravedad de la enfermedad.
ConclusionesLos pacientes con esquizofrenia a seguimiento ambulatorio no siguen las recomendaciones de la OMS sobre dietas saludables ni actividad física. Tanto la gravedad clínica de la enfermedad como el estado civil y la convivencia se asociaron con malos hábitos alimenticios y déficit de nutrientes. Estos datos deben ser tenidos en cuenta por el personal de enfermería a la hora de implementar cuidados específicos en la práctica clínica habitual.
Schizophrenia is a chronic mental disorder, which includes psychopathological manifestations in thinking, perception, emotions, movement, and behaviour, and impairs functioning and quality of life.1,2 In recent years, a growing number of studies have indicated that people with severe mental disorders, such as schizophrenia, have poorer physical health than their peers.3,4 This may be due to multiple factors, including the disease process itself, poor diet, a sedentary lifestyle, and certain antipsychotic medications that could add to the risk of developing cardiovascular and metabolic disorders.5,6
Several studies claim that the mortality rate is higher than in the general population,7,8 with a 20−30 year lower life expectancy.9,10 All these studies point to cardiovascular and endocrine-metabolic diseases as the major causes of death and physical disability among people with a mental illness.5,7–10 The RICAVA study11 describes how one third of the sample was obese or overweight, and half of the sample had hypercholesterolaemia, 38% hypertriglyceridaemia, and one third diabetes mellitus and hypertension. Therefore, patients with schizophrenia are a population group susceptible to health promotion and prevention interventions.12
The Food and Agriculture Organisation of the United Nations defines eating habits as “a set of customs that condition the way in which individuals or groups select, prepare and consume food, influenced by the availability of food, level of education and access to food”. They also specify nutritional status as a “condition of the body as a result of the relationship between individual nutritional needs and the intake, absorption and utilisation of nutrients contained in the food”.3 They go on to define nutrients as “chemical substances contained in food that are necessary for the normal functioning of the body. The six main types of nutrients are proteins, carbohydrates, fats, minerals, vitamins and water”.13 Macronutrients and micronutrients are differentiated within these. Various studies14–16 have described the diet of patients diagnosed with schizophrenia14–16 as poorly or not at all balanced. In terms of their eating habits, these patients have been described as consuming more foods rich in fats and sugars such as cured meats and pastries, but not fish, fruit, or sunflower oil.12 Regarding macro- and micronutrients, these patients have been observed to consume fewer saturated fatty acids, polyunsaturated fatty acids, and monounsaturated fatty acids, but more trans-fatty acids and carbohydrates.17
As there is a lack of knowledge about eating and nutritional habits and their relationship with disease severity in people diagnosed with schizophrenia, which is fundamental information for health promotion interventions and cardiovascular and endocrine-metabolic disease prevention. The present study seeks to describe these parameters and hypothesises that these patients will have poor eating, nutritional, and physical activity habits.
Material and methodsThis study was approved by the Regional Clinical Research Ethics Committee of the Principality of Asturias and by the Research Commission of the Central University Hospital of Asturias (Ref. n.° 48/12). The study was explained to the patients, and they signed the informed consent form before any procedure was performed.
This is a secondary analysis of a subsample of patients who participated in the study “Physical comorbidity in severe mental disorder: design, intervention and evaluation of a programme for the improvement of the patient's general state of health”, backed by the Ministry of Economy and Competitiveness, Instituto de Salud Carlos III and FEDER funds (PI12/00882), and who agreed to record their eating habits for one week.
Study populationThe study was conducted with a total sample of 31 patients, from the 84 that comprised the total sample, diagnosed with schizophrenia according to the International Classification of Mental and Behavioural Disorders (ICD-10) (World Health Organization [WHO], 1992.18
The inclusion criteria were: 1) age 18–65 years; 2) patients who had been clinically stable for the previous 6 months (no hospitalisation or acute exacerbation); and 3) having provided written informed consent to participate in the study. The exclusion criteria were: 1) refusal to participate in the study; 2) severe physical illness and/or significant disability/incapacity on inclusion and in parallel with the study. Data were collected between January and March 2017.
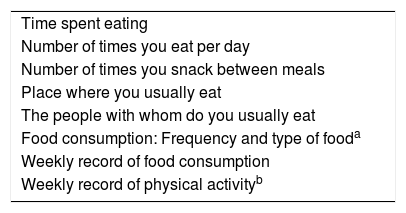
EvaluationAll the subjects were interviewed comprehensively by the same nurse who had been trained to conduct the study. In addition, each patient was trained to complete the ad hoc questionnaire on eating and nutritional habits and physical activity. Demographic and clinical characteristics were obtained (Clinical Global Impression (CGI-S), years of disease progression, degree of disability, toxic substance abuse, BMI, and abdominal girth). An ad hoc questionnaire was completed to assess eating and nutritional habits and physical activity, such as: time spent eating, number of times the subjects eat per day, number of times they snack between meals, place where they usually eat, people with whom they usually eat, food consumption (frequency and type of food, according to the recommendations of the Spanish Society of Community Nutrition19,20). This information was recorded weekly for one month at home. In addition, time spent on physical activity (in minutes) and the number of times they practised strength exercises were recorded according to the criteria of the World Health Organisation (WHO), “Global strategy on diet, physical activity and health”21 (Table 1). Once the weekly food consumption records were obtained for each participant, the macro- and micronutrients ingested daily over one week were analysed using the computer programme Alimentador.22 This is an online programme that allows nutritional calculations to be made for each food intake. The programme was developed by Spanish nutrition specialists and is endorsed by the Spanish Society of Dietetics and Health Sciences (SEDCA) and the Healthy Eating Foundation.
Ad hoc questionnaire: eating, nutritional and physical activity habits.
| Time spent eating |
| Number of times you eat per day |
| Number of times you snack between meals |
| Place where you usually eat |
| The people with whom do you usually eat |
| Food consumption: Frequency and type of fooda |
| Weekly record of food consumption |
| Weekly record of physical activityb |
According to the recommendations of the Spanish Society of Community Nutrition, for more details see Table 3.
We used SPSS for Windows version 20.0 for the statistical analysis. First, a descriptive analysis of socio-demographic and clinical characteristics was performed, including eating and nutritional habits and physical exercise (mean and standard deviation for quantitative variables and frequencies and percentages for qualitative variables). The χ2 test, Student's t-test and Pearson's correlation were used to analyse the association between variables, depending on the type of variables examined. The confidence level was established at 95%, and the level of statistical significance at .05.
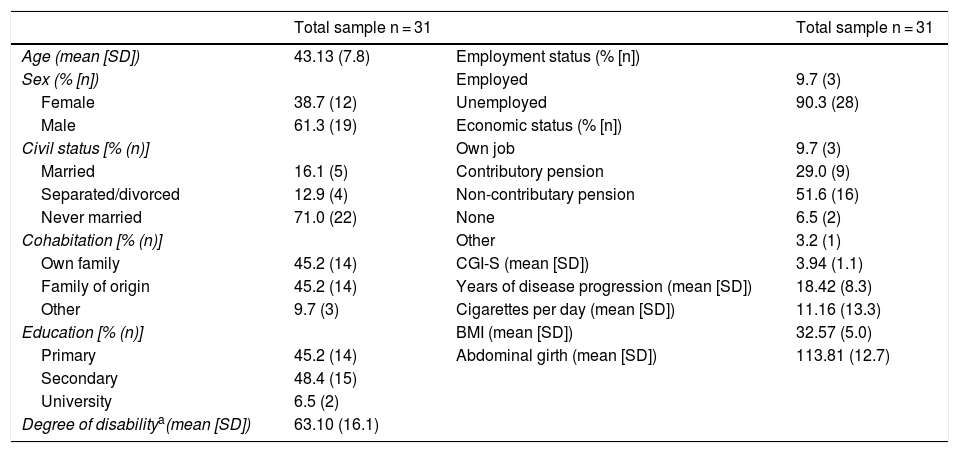
ResultsThe mean age of the sample was 43.13 years (SD 7.8), 61.3% were male. The mean disease severity score, using the CGI-S, was 3.94 (SD 1.1), i.e., moderately ill, with a mean of 18.42 (SD 8.3) years of disease progression. The mean BMI was 32.57 (SD 5.0), i.e., type II obesity, and the mean abdominal girth was 113.81 (SD 12.7) cm. Table 2 shows the sociodemographic and clinical characteristics.
Socio-demographic and clinical characteristics of the patients with a diagnosis of schizophrenia.
| Total sample n = 31 | Total sample n = 31 | ||
|---|---|---|---|
| Age (mean [SD]) | 43.13 (7.8) | Employment status (% [n]) | |
| Sex (% [n]) | Employed | 9.7 (3) | |
| Female | 38.7 (12) | Unemployed | 90.3 (28) |
| Male | 61.3 (19) | Economic status (% [n]) | |
| Civil status [% (n)] | Own job | 9.7 (3) | |
| Married | 16.1 (5) | Contributory pension | 29.0 (9) |
| Separated/divorced | 12.9 (4) | Non-contributary pension | 51.6 (16) |
| Never married | 71.0 (22) | None | 6.5 (2) |
| Cohabitation [% (n)] | Other | 3.2 (1) | |
| Own family | 45.2 (14) | CGI-S (mean [SD]) | 3.94 (1.1) |
| Family of origin | 45.2 (14) | Years of disease progression (mean [SD]) | 18.42 (8.3) |
| Other | 9.7 (3) | Cigarettes per day (mean [SD]) | 11.16 (13.3) |
| Education [% (n)] | BMI (mean [SD]) | 32.57 (5.0) | |
| Primary | 45.2 (14) | Abdominal girth (mean [SD]) | 113.81 (12.7) |
| Secondary | 48.4 (15) | ||
| University | 6.5 (2) | ||
| Degree of disabilitya(mean [SD]) | 63.10 (16.1) |
SD: Standard Deviation.
Regarding the characteristics of eating habits, the patients spent a mean 15.65 (SD 9.5) minutes eating, 3.71 (SD 0.9) meals per day. Of the sample, 51.6% did not snack between meals, 93.5% ate at home, and 80.6% usually ate with others.
In relation to physical activity, 93.5% of the sample did not comply with the World Health Organisation (WHO) recommendations on physical activity. The highest level of physical activity was light with a mean 331.45 (SD 540.3) minutes per week. However, no statistical association was found with sociodemographic or clinical profile, eating habits or nutrients.
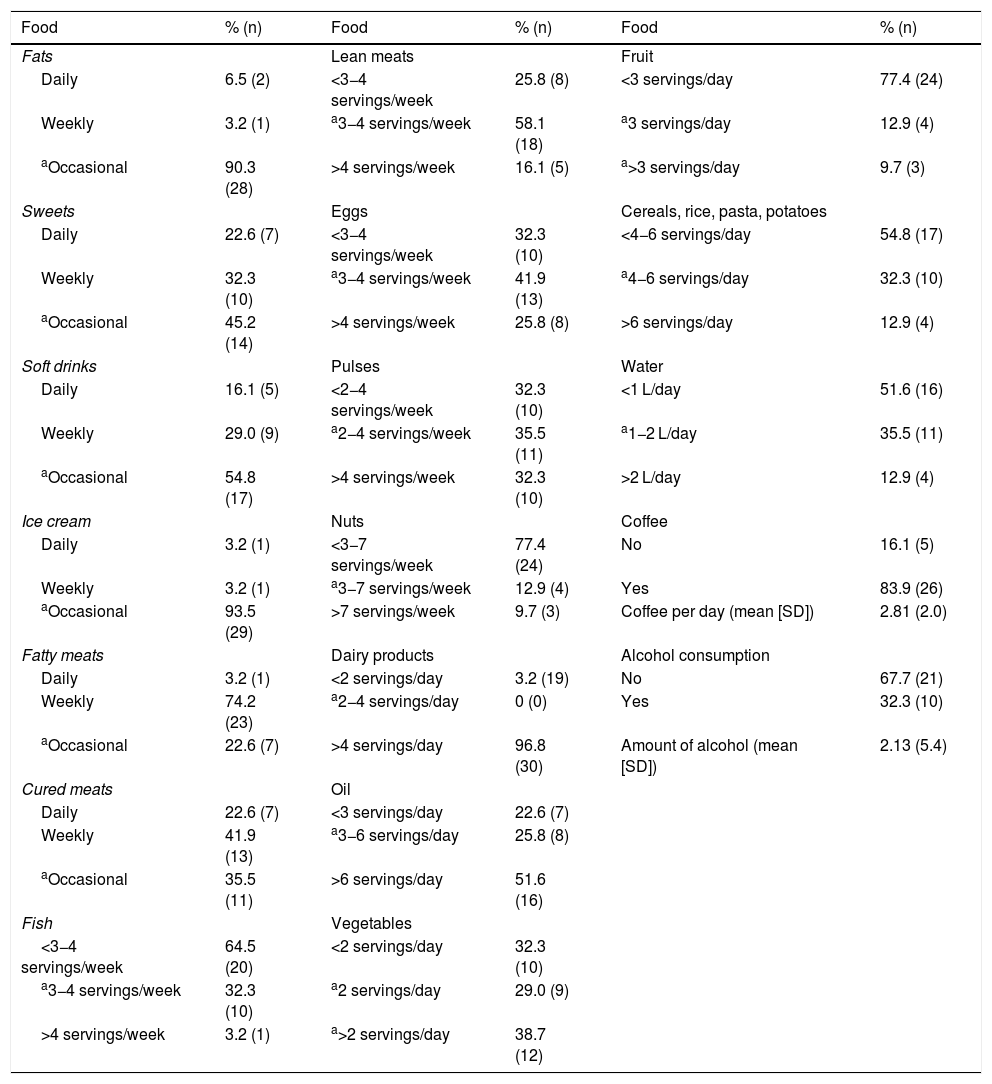
Frequency of food consumptionFrom the data shown in Table 3, we note that overall, the patients had poor eating habits in terms of frequency of food consumption. That is, 74.2% consumed fatty meat weekly, 64.5% less than 3−4 portions of fish per week, 77.4% less than 3 portions of fruit per day, and 51.6% of the sample drank less than one litre of water per day. A total of 83.9% consumed coffee daily with a mean 2.81 (SD 2.0) coffees per day. No statistically significant differences were found in eating habits according to age or gender. However, 40% of those who were married consumed fat daily compared to 0% of those who were single or separated/divorced (X2 = 11.424, P = .022). Those who lived with their own family or family of origin took a higher proportion of more than 4 daily servings of dairy products (X2 = 9.644, P = .008) compared to those who lived alone or with others. In addition, only those living alone or with others met the recommended consumption of oil (3−6 servings per day), (X2 = 9.846, P = .043). The patients who lived with their own family or family of origin consumed more coffee than those living alone or with others (X2 = 6.535, P = .038). However, we found no differences in eating habits according to disease severity, length of disease progression, BMI, or abdominal girth.
Frequency of food consumption in patients with a diagnosis of schizophrenia.
| Food | % (n) | Food | % (n) | Food | % (n) |
|---|---|---|---|---|---|
| Fats | Lean meats | Fruit | |||
| Daily | 6.5 (2) | <3−4 servings/week | 25.8 (8) | <3 servings/day | 77.4 (24) |
| Weekly | 3.2 (1) | a3−4 servings/week | 58.1 (18) | a3 servings/day | 12.9 (4) |
| aOccasional | 90.3 (28) | >4 servings/week | 16.1 (5) | a>3 servings/day | 9.7 (3) |
| Sweets | Eggs | Cereals, rice, pasta, potatoes | |||
| Daily | 22.6 (7) | <3−4 servings/week | 32.3 (10) | <4−6 servings/day | 54.8 (17) |
| Weekly | 32.3 (10) | a3−4 servings/week | 41.9 (13) | a4−6 servings/day | 32.3 (10) |
| aOccasional | 45.2 (14) | >4 servings/week | 25.8 (8) | >6 servings/day | 12.9 (4) |
| Soft drinks | Pulses | Water | |||
| Daily | 16.1 (5) | <2−4 servings/week | 32.3 (10) | <1 L/day | 51.6 (16) |
| Weekly | 29.0 (9) | a2−4 servings/week | 35.5 (11) | a1−2 L/day | 35.5 (11) |
| aOccasional | 54.8 (17) | >4 servings/week | 32.3 (10) | >2 L/day | 12.9 (4) |
| Ice cream | Nuts | Coffee | |||
| Daily | 3.2 (1) | <3−7 servings/week | 77.4 (24) | No | 16.1 (5) |
| Weekly | 3.2 (1) | a3−7 servings/week | 12.9 (4) | Yes | 83.9 (26) |
| aOccasional | 93.5 (29) | >7 servings/week | 9.7 (3) | Coffee per day (mean [SD]) | 2.81 (2.0) |
| Fatty meats | Dairy products | Alcohol consumption | |||
| Daily | 3.2 (1) | <2 servings/day | 3.2 (19) | No | 67.7 (21) |
| Weekly | 74.2 (23) | a2−4 servings/day | 0 (0) | Yes | 32.3 (10) |
| aOccasional | 22.6 (7) | >4 servings/day | 96.8 (30) | Amount of alcohol (mean [SD]) | 2.13 (5.4) |
| Cured meats | Oil | ||||
| Daily | 22.6 (7) | <3 servings/day | 22.6 (7) | ||
| Weekly | 41.9 (13) | a3−6 servings/day | 25.8 (8) | ||
| aOccasional | 35.5 (11) | >6 servings/day | 51.6 (16) | ||
| Fish | Vegetables | ||||
| <3−4 servings/week | 64.5 (20) | <2 servings/day | 32.3 (10) | ||
| a3−4 servings/week | 32.3 (10) | a2 servings/day | 29.0 (9) | ||
| >4 servings/week | 3.2 (1) | a>2 servings/day | 38.7 (12) |
SD: Standard Deviation.
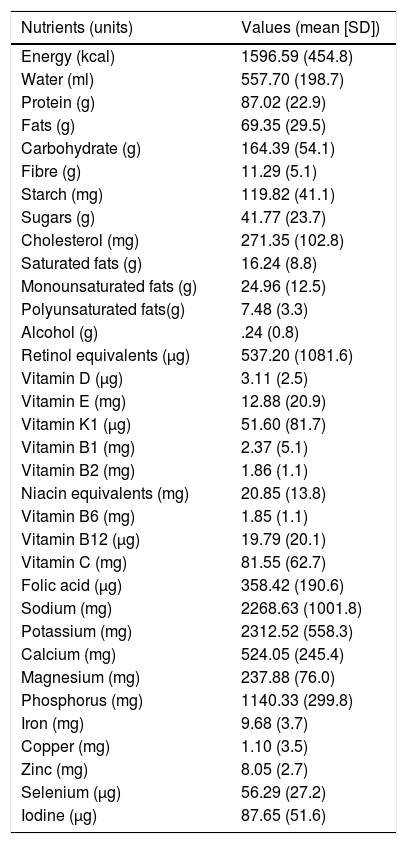
The patients reported a deficiency in mean water intake of 557.70 mL (SD 198.7), fibre 11.29 g (SD 5.2), and magnesium 237.88 mg (SD 76.0) as shown in Table 4. Vitamin deficiencies were also identified. Specifically, a deficiency of vitamin A of 537.29 g (SD 1081.6), of vitamin D of 3.11 g (SD 2.5), of vitamin E of 12.88 mg (SD 20.9), of vitamin K1 of 51.60 g (SD 81.7), of vitamin C of 81.55 mg (SD 62.7), and of folic acid of 358.42 g (SD 190.6). Regarding the nutrients analysed according to clinical parameters, significant differences were only found according to disease severity and body mass index (BMI). The greater the severity of the disease in the women, the lower the consumption of retinol (vitamin A) (r = −.602, P = .039) and vitamin K1 (r = −.693, P = .012), and in the men, the greater the severity of the disease, the lower the consumption of alcohol (r = −.528, P = .020). With respect to BMI, we only observed significant results in the men, the higher the BMI, the lower the consumption of saturated lipids (r = −.628, P = .004), vitamin D (r = −.516, P = .024) and vitamin B1, or thiamine (r = −.616, P = .005).
Mean nutrient intake/day in patients with schizophrenia.
| Nutrients (units) | Values (mean [SD]) |
|---|---|
| Energy (kcal) | 1596.59 (454.8) |
| Water (ml) | 557.70 (198.7) |
| Protein (g) | 87.02 (22.9) |
| Fats (g) | 69.35 (29.5) |
| Carbohydrate (g) | 164.39 (54.1) |
| Fibre (g) | 11.29 (5.1) |
| Starch (mg) | 119.82 (41.1) |
| Sugars (g) | 41.77 (23.7) |
| Cholesterol (mg) | 271.35 (102.8) |
| Saturated fats (g) | 16.24 (8.8) |
| Monounsaturated fats (g) | 24.96 (12.5) |
| Polyunsaturated fats(g) | 7.48 (3.3) |
| Alcohol (g) | .24 (0.8) |
| Retinol equivalents (μg) | 537.20 (1081.6) |
| Vitamin D (μg) | 3.11 (2.5) |
| Vitamin E (mg) | 12.88 (20.9) |
| Vitamin K1 (μg) | 51.60 (81.7) |
| Vitamin B1 (mg) | 2.37 (5.1) |
| Vitamin B2 (mg) | 1.86 (1.1) |
| Niacin equivalents (mg) | 20.85 (13.8) |
| Vitamin B6 (mg) | 1.85 (1.1) |
| Vitamin B12 (μg) | 19.79 (20.1) |
| Vitamin C (mg) | 81.55 (62.7) |
| Folic acid (μg) | 358.42 (190.6) |
| Sodium (mg) | 2268.63 (1001.8) |
| Potassium (mg) | 2312.52 (558.3) |
| Calcium (mg) | 524.05 (245.4) |
| Magnesium (mg) | 237.88 (76.0) |
| Phosphorus (mg) | 1140.33 (299.8) |
| Iron (mg) | 9.68 (3.7) |
| Copper (mg) | 1.10 (3.5) |
| Zinc (mg) | 8.05 (2.7) |
| Selenium (μg) | 56.29 (27.2) |
| Iodine (μg) | 87.65 (51.6) |
SD: Standard Deviation.
In the present study, patients diagnosed with schizophrenia in outpatient treatment were found to have unhealthy lifestyles, i.e., poor eating, nutritional and physical activity habits, as hypothesised. We also found a deficiency in the intake of several nutrients, mainly vitamins.
In terms of the sociodemographic profile of the sample, the majority were men, single, living with their own family or family of origin, with secondary education, unemployed and with more than 15 years of disease progression; this profile coincides with the studies found in the same geographical area.11,23 The BMI of the patients corresponded to type II obesity, similar to that found in other studies,11,14,23 which confers a high risk of developing comorbid diseases such as type 2 diabetes mellitus, dyslipidaemia, and hypertension.24
In terms of eating habits, the data obtained are like those described in the literature14; approximately half the sample spent less than 15 min eating and ate between 4 and 5 meals a day. More than half the sample snacked daily or occasionally, and almost all the sample ate at home. Almost all of them engaged in light physical activity without meeting the WHO physical activity recommendations, which is consistent with the CLAMORS study.23
There are few studies on food and nutrient intake in the schizophrenia population. However, as in other studies,14,16 there is excess consumption of fatty meat, cured meats, dairy products and oil compared to a reduced consumption of fish, fruit, cereals, pasta, rice, and water. Furthermore, as in other studies,15,25–27 they had nutritional deficiencies in fibre, vitamins (A, D, E, K, C, folic acid) and magnesium. However, daily coffee consumption was higher than in the studies consulted.14 These unhealthy habits are associated with the clinical severity of the mental illness, but only in the women. In the women, low levels of retinol and vitamin K1 were associated with greater severity. Although a synergistic interaction between vitamins D and K has now been hypothesised in their role in the development of osteoporosis and atherosclerosis, no information has been found on their role in schizophrenia or even in any mental disorder.28 However, Tsuruga et al.27 report a link between a “cereal” dietary pattern in the diet and the risk of schizophrenia. In addition, a relationship was found with demographic profile, especially with marital status and cohabitation, such that married subjects consumed more fat than recommended and those living with their own or their family of origin consumed more dairy and more coffee. To our knowledge, no studies have examined these issues in non-institutionalised schizophrenia patients.
The limitations and biases of the study need to be considered. First, the “Hawthorne effect” whereby subjects alter their habits and responses because they are in a research study. Second, the sample size is relatively small, although the comprehensive collection of information on eating, nutritional and physical activity habits is worth highlighting. Third, it is a cross-sectional study that does not allow for temporal follow-up of participants. Finally, in the absence of a control group from the general population, we cannot conclude whether their eating habits are better or worse, but can only describe whether they comply with the recommendations for food consumption, nutrition, and physical activity.
In conclusion, patients with a diagnosis of schizophrenia under outpatient maintenance treatment do not follow the WHO recommendations for eating, nutrition, and physical activity habits. Nursing staff should consider these data when implementing specific care in routine clinical practice, according to the quality indicators for depression, bipolar disorder, and schizophrenia.29 Furthermore, this study may suggest that there is a need for intervention in the family unit to work on dietary education, as eating and nutritional habits in this study are especially related to marital status and cohabitation.
FundingThis work is part of a research project entitled: “Physical comorbidity in severe mental disorder: design, intervention and evaluation of a programme for the improvement of the patient's general state of health”, with the support of the Ministry of Economy and Competitiveness, Instituto de Salud Carlos III and FEDER funds (PI12/00882).
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Zurrón Madera P, Casaprima Suárez S, García Álvarez L, García-Portilla González MP, Junquera Fernández R, Lluch Canut MT. Hábitos alimenticios y nutricionales en pacientes con esquizofrenia. Rev Psiquiatr Salud Ment (Barc). 2022;15:54–60.