Suicide is a major public health problem worldwide, and an approach is necessary due to its high potential for prevention. This paper examines the main characteristics of people admitted to hospitals in the Community of Madrid (Spain) with suicidal behaviour, and the factors associated with their hospital mortality.
Material and methodsA study was conducted on patients with E950-E959 codes of suicide and self-inflicted injuries of the International Classification of Diseases, Ninth Revision, Clinical Modification, contained in any diagnostic field of the minimum basic data set at hospital discharge between 2003 and 2013. Sociodemographic, clinical and health care variables were assessed by uni- and multivariate logistic regression analysis in the evaluation of factors associated with hospital mortality.
ResultsHospital suicidal behaviour predominates in women (58.7%) and in middle-age. Hospital mortality is 2.2% (1.6% in women and 3.2% in men), increasing with age. Mental disorders are detected 3–4 times more in secondary diagnoses. The main primary diagnosis (>74%) is poisoning with substances, with lower mortality (∼1%) than injury by hanging and jumping from high places (≥12%), which have the highest numbers. Other factors associated with increased mortality include different medical comorbidities and severity of the injury, while length of stay and mental disorders are protective factors. Type of hospital, poisoning, and Charlson index are associated differently with mortality in men and women.
ConclusionsHospitalised suicidal acts show a low mortality, mainly related to comorbidities and the severity of injuries.
El suicidio es un importante problema de salud pública mundial, de necesario abordaje por su alto potencial preventivo. Este trabajo estudia las principales características de las personas ingresadas en hospitales de la Comunidad de Madrid (España) con conducta suicida y los factores asociados a su mortalidad intrahospitalaria.
Material y métodosSe estudian los códigos E950-E959 de suicidio y lesiones autoinfligidas de la Clasificación Internacional de Enfermedades, Novena Revisión, Modificación Clínica, contenidos en los campos diagnósticos del conjunto mínimo básico de datos al alta hospitalaria entre 2003 y 2013. Se describen variables sociodemográficas, clínicas y asistenciales mediante análisis uni y multivariante de regresión logística en la valoración de factores asociados a la mortalidad intrahospitalaria.
ResultadosLa conducta suicida hospitalizada predomina en mujeres (58,7%) y en edades medias. La mortalidad intrahospitalaria es del 2,2% (1,6% en mujeres y 3,2% en hombres), aumentando con la edad. Los trastornos mentales se detectan 3–4 veces más en diagnósticos secundarios. El diagnóstico principal mayoritario (>74%) es el envenenamiento por sustancias, con una mortalidad inferior (∼1%) a la de las lesiones por ahorcamiento y precipitación (≥12%), que presentan las cifras más elevadas. Otros factores asociados con una mayor mortalidad son diversas comorbilidades médicas y la gravedad de la lesión, mientras que la estancia y los trastornos mentales son factores protectores en ambos sexos. El tipo de hospital, el envenenamiento con sustancias y el índice de Charlson se asocian a la mortalidad de forma diferencial en hombres y mujeres.
ConclusionesLos actos suicidas hospitalizados presentan una baja mortalidad, la cual está principalmente relacionada con las comorbilidades y la gravedad de las lesiones.
Suicide is a major world public health problem and causes an annual 800,000 deaths.1 A mental health action pan has been implemented, based on experience with recent previous World Health Organisation initiatives, as part of suicide prevention with the goal of reducing suicide rates by 10% by 2020.2 Likewise, there have been messages warning of the need for a global preventive approach, to minimise its tragic consequences and social and economic repercussions.3
The latest research has lead to better knowledge of suicidal behaviour, acknowledged as a complex phenomenon in which many biological, psychological, social, environmental and cultural aspects are involved and interact. Some of the factors associated with suicide risks are personal and universal, such as prior suicide attempts, mental disorders (anxiety disorders, behavioural disorders, substance abuse and dependence, bipolar disorder, schizophrenia), biological constraints, parental psychopathology, childhood adversities (physical or sexual abuse, and domestic violence), and financial or relationship losses.4 It involves other factors from a social and community perspective, such as living conditions, religion, integration and social support, conflictive relationships, etc., and limited social contact has been detected as a factor strongly related to suicidal behaviour in people over the age of 65 in industrialised countries.5
More than 3800 people die each year in our country due to suicide, which is the primary cause of death by external causes because road traffic accident deaths have diminished in recent years. The overall trend of death by suicide has been decreasing since the end of the nineties. The highest rates are found in elderly men, with a mortality of between 3 and 4 times higher than that of women.6 The situation in the Community of Madrid (CM) is parallel to that of the nation, with figures that are traditionally lower.7
An effect of suicidal behaviour that has been less investigated is the morbidity in individuals who do not die immediately after an attempt. It is well known that suicide attempts are much more common than deaths by suicide, between approximately 10–20 times more common, and are more frequent in women and at younger ages.8,9 Most of these people are attended by the health system, either primary care, or specialist mental health care; some patients due to their severity or risk of fatal repeat attempts require hospitalisation. There are many problems in the study of morbidity associated with suicidal behaviour, in terms of definition and quantification, as well as issues with the recording, classification and underdiagnosis of this condition in our information systems.10
Although it is possible to study suicidal behaviour through various information sources (mortality, primary care, hospital care, etc.), each sources only offers partial knowledge of the phenomenon, highlighting the difficulty of a comprehensive approach and the limitations of the information devices used.
This paper aims to tackle a specific, little-studied aspect of suicidal behaviour, which is to discover the main characteristics associated with the hospitalisation of patients initially surviving a suicide attempt and admitted to a CM hospital, and to analyse the factors associated with their in-hospital mortality. Due to its major impact on results we chose a descriptive and sex-differentiated strategy.
Material and methodsSource of information, scope and period of studyThe minimum basic dataset (MBDS) was used on admission to a CM hospital between 2003 and 2013 for people resident in the region. The MBDS comprises an information system for the collection of data and indicators of universal and mandatory hospital operation for the entire National Health System relating to periods of hospitalisation. The CM Ministry of Health is in charge of its management, which records, maintains and periodically assesses the data provided by all public and private inpatient healthcare centres and establishments, and those with outpatient surgery units.
Selection of the study populationHospital admissions were selected corresponding to codes E950-E959, included in the Supplementary classification of external causes of injury and poisoning (E codes) of the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM), under the heading suicide and self-inflicted injury in all the diagnostic fields of the CM MBDS, including the principal diagnosis (reason for admission) and 13 secondary diagnoses (those affecting their hospital stay or the treatment given for the current episode). In order to monitor any errors of inclusion and achieve greater homogeneity, we excluded 108 records that exceeded 96 days of hospital stay (percentile 99), because we considered extremely long hospital stays difficult to relate to the consequences of the suicidal episode. Similarly, we rejected 18 records of patients under the age of 7, considering the capacity of volition to be insufficiently developed at an early age.
Study variablesWe studied sociodemographic variables: sex; age, continuously and categorically; country of origin –Spain, Foreign and Unknown. We considered the following clinical variables: main and/or secondary diagnoses, categorised according to the chapters of ICD-9-CM –Infectious diseases, Neoplasms, Endocrine diseases, Diseases of the Blood, Mental disorders, Diseases of the Nervous System, Circulatory System, Respiratory System, Digestive System, Genitourinary System, Complications of Pregnancy, Childbirth and the Puerperium, Skin, Diseases of the Musculoskeletal System and Connective Tissue, Congenital Anomalies, Conditions in the Perinatal period, Ill-defined conditions, Injuries and poisoning; causes of injuries and poisoning –Poisoning by solid or liquid substances, Injuries by cutting or piercing instrument, Injuries by hanging, strangulation or asphyxiation, Injuries from jumping from high places, Other causes of injury; Charlson index,11 that summarises the patient's comorbidity, 4-category ordinal scale (from 0 to ≥3), and the Maximum Abbreviated Injury Scale (MAIS), that considers the injury with the highest score on the Abbreviated Injury Scale,12 initial classifying ordinal scale of the severity of the injuries in 7 categories (from 0 to 6), recoded in our paper into 6 (from 0 to ≥5) by merging the last 2 due to the low number of units in each. Finally some care variables were analysed: type of hospital –Public and Private; hospital stay and circumstances at discharge –Home, Transfer or referral, Voluntary discharge, Death, Other.
Statistical analysisWe used descriptive statistical techniques according to the qualitative or quantitative nature of the variables, describing their frequency distribution, measures of central tendency and dispersion, and relationship with mortality. To compare the proportions we used the χ2 or Fisher's exact test, and the Mann–Whitney U test to compare the means. Logistic regression models were adjusted by uni- and multivariate analyses to assess in-hospital mortality (dependent variable), using as independent variables: age, sex, country of origin, type of hospital, stay, causes of injury and poisoning, comorbidities in main diagnosis and/or secondary diagnoses, Charlson Index and MAIS. Stratification by sex was used in all the analyses, providing differentiated results in the form of odds ratios and their confidence intervals for men (ORm) and women (ORw) in the logistical regression. We used SPSS v. 21.0 and Epidat v. 4.1 for analysis of the data.
Ethical aspectsThis study was undertaken in compliance with current legal regulations and following the recommendations of the Declaration of Helsinki.
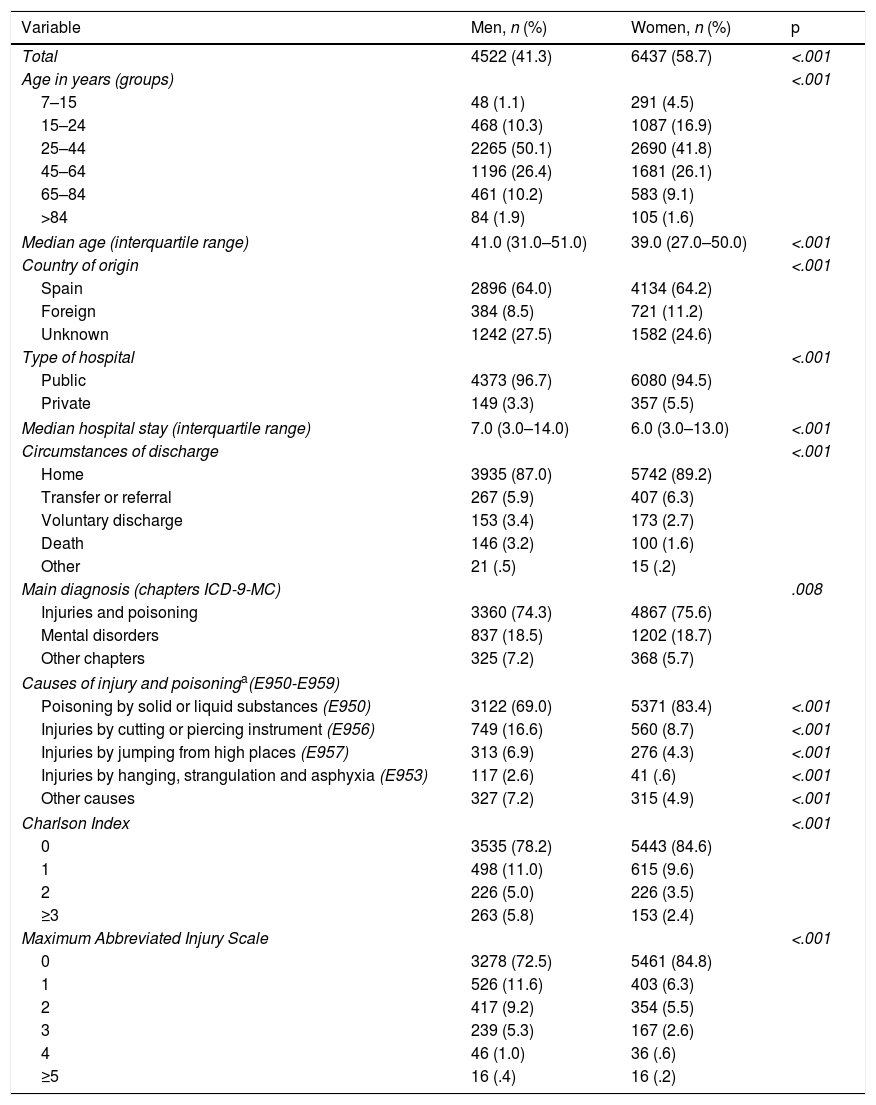
ResultsFinally, 10,959 records were studied. Around 60% of the hospital admissions were of women (Table 1). The mean age of the men was 2 years older (41.0 vs. 39.0 years; p<.001). There were more women under the age of 25 years (21.4% vs. 11.4%), whereas three quarters of the episodes occurred in men aged between 25 and 64. Sixty-four percent of both sexes were born in Spain. Most of the admissions were to public hospitals. The median stay was one day more for the men (7.0 vs. 6.0 days; p<.001). Discharge home was the most usual circumstance for both sexes. The mortality of the men was double that of the women (3.2 vs. 1.6%; p<.001).
Principal sociodemographic, clinical, and healthcare characteristics per sex in the selection Suicide and self-inflicted injuries (E950-E959) in the diagnostic fields of the minimum basic data set on hospital admission of the Community of Madrid, 2003–2013 (noverall=10,959).
| Variable | Men, n (%) | Women, n (%) | p |
|---|---|---|---|
| Total | 4522 (41.3) | 6437 (58.7) | <.001 |
| Age in years (groups) | <.001 | ||
| 7–15 | 48 (1.1) | 291 (4.5) | |
| 15–24 | 468 (10.3) | 1087 (16.9) | |
| 25–44 | 2265 (50.1) | 2690 (41.8) | |
| 45–64 | 1196 (26.4) | 1681 (26.1) | |
| 65–84 | 461 (10.2) | 583 (9.1) | |
| >84 | 84 (1.9) | 105 (1.6) | |
| Median age (interquartile range) | 41.0 (31.0–51.0) | 39.0 (27.0–50.0) | <.001 |
| Country of origin | <.001 | ||
| Spain | 2896 (64.0) | 4134 (64.2) | |
| Foreign | 384 (8.5) | 721 (11.2) | |
| Unknown | 1242 (27.5) | 1582 (24.6) | |
| Type of hospital | <.001 | ||
| Public | 4373 (96.7) | 6080 (94.5) | |
| Private | 149 (3.3) | 357 (5.5) | |
| Median hospital stay (interquartile range) | 7.0 (3.0–14.0) | 6.0 (3.0–13.0) | <.001 |
| Circumstances of discharge | <.001 | ||
| Home | 3935 (87.0) | 5742 (89.2) | |
| Transfer or referral | 267 (5.9) | 407 (6.3) | |
| Voluntary discharge | 153 (3.4) | 173 (2.7) | |
| Death | 146 (3.2) | 100 (1.6) | |
| Other | 21 (.5) | 15 (.2) | |
| Main diagnosis (chapters ICD-9-MC) | .008 | ||
| Injuries and poisoning | 3360 (74.3) | 4867 (75.6) | |
| Mental disorders | 837 (18.5) | 1202 (18.7) | |
| Other chapters | 325 (7.2) | 368 (5.7) | |
| Causes of injury and poisoninga(E950-E959) | |||
| Poisoning by solid or liquid substances (E950) | 3122 (69.0) | 5371 (83.4) | <.001 |
| Injuries by cutting or piercing instrument (E956) | 749 (16.6) | 560 (8.7) | <.001 |
| Injuries by jumping from high places (E957) | 313 (6.9) | 276 (4.3) | <.001 |
| Injuries by hanging, strangulation and asphyxia (E953) | 117 (2.6) | 41 (.6) | <.001 |
| Other causes | 327 (7.2) | 315 (4.9) | <.001 |
| Charlson Index | <.001 | ||
| 0 | 3535 (78.2) | 5443 (84.6) | |
| 1 | 498 (11.0) | 615 (9.6) | |
| 2 | 226 (5.0) | 226 (3.5) | |
| ≥3 | 263 (5.8) | 153 (2.4) | |
| Maximum Abbreviated Injury Scale | <.001 | ||
| 0 | 3278 (72.5) | 5461 (84.8) | |
| 1 | 526 (11.6) | 403 (6.3) | |
| 2 | 417 (9.2) | 354 (5.5) | |
| 3 | 239 (5.3) | 167 (2.6) | |
| 4 | 46 (1.0) | 36 (.6) | |
| ≥5 | 16 (.4) | 16 (.2) | |
Three quarters of the hospitalised suicide attempts involved injuries and poisoning in the main diagnosis, both for men and women, while mental disorder was diagnosed in around 18%, with similar figures in both sexes. The main cause of injury was poisoning by substances, more women (83.4% vs. 69.0%; p<.001), followed by injuries caused by a cutting or piercing instrument, more men (16.6% vs. 8.7%; p<.001). Most of the episodes presented with no comorbidities (Charlson Index) and no scorable injuries (MAIS), in both cases there were more in women (84.6% vs. 78.2% [p<.001] and 84.8% vs. 72.5% [p<.001], respectively) (Table 1).
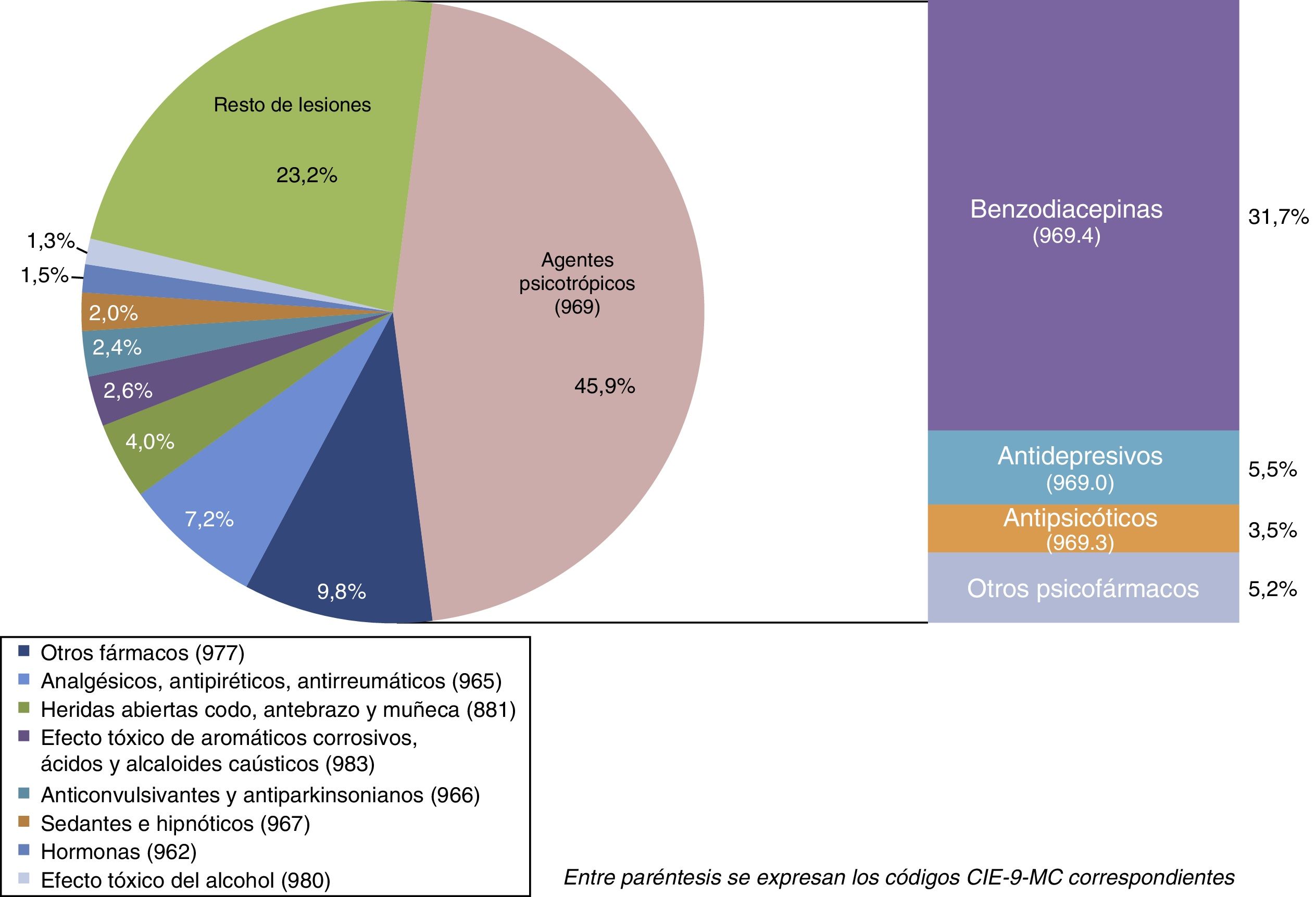
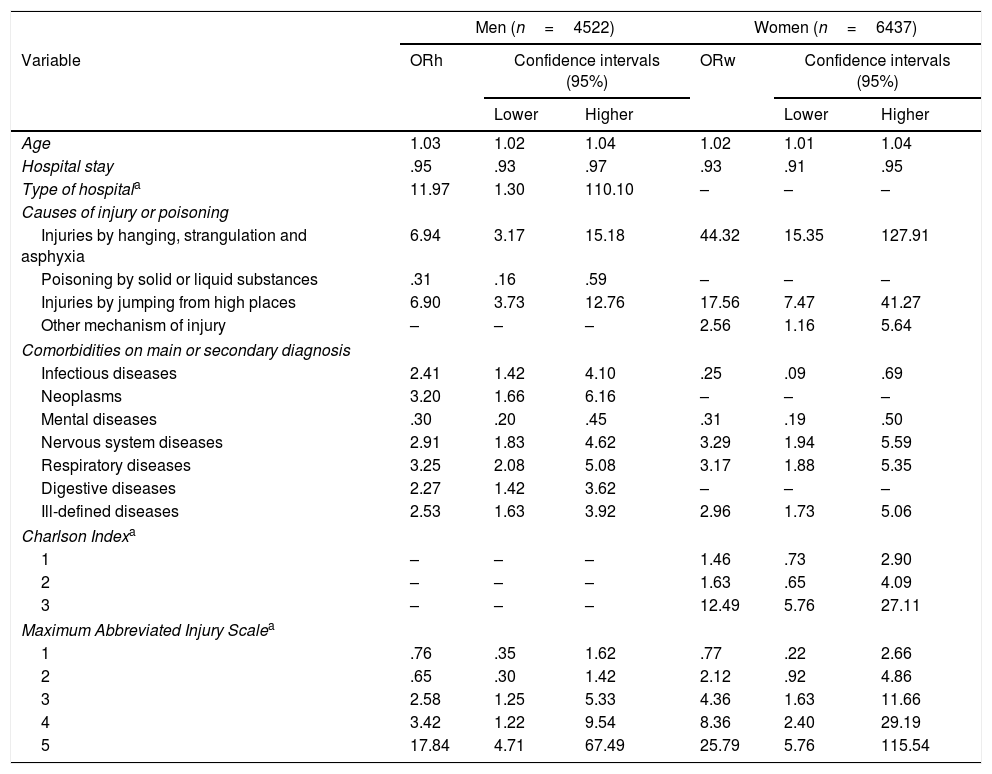
Forty-five point nine percent of the injuries and poisoning in the main diagnosis involved the intake of psychotropic agents, chiefly benzodiazepines (31.7% of the total) (Fig. 1).
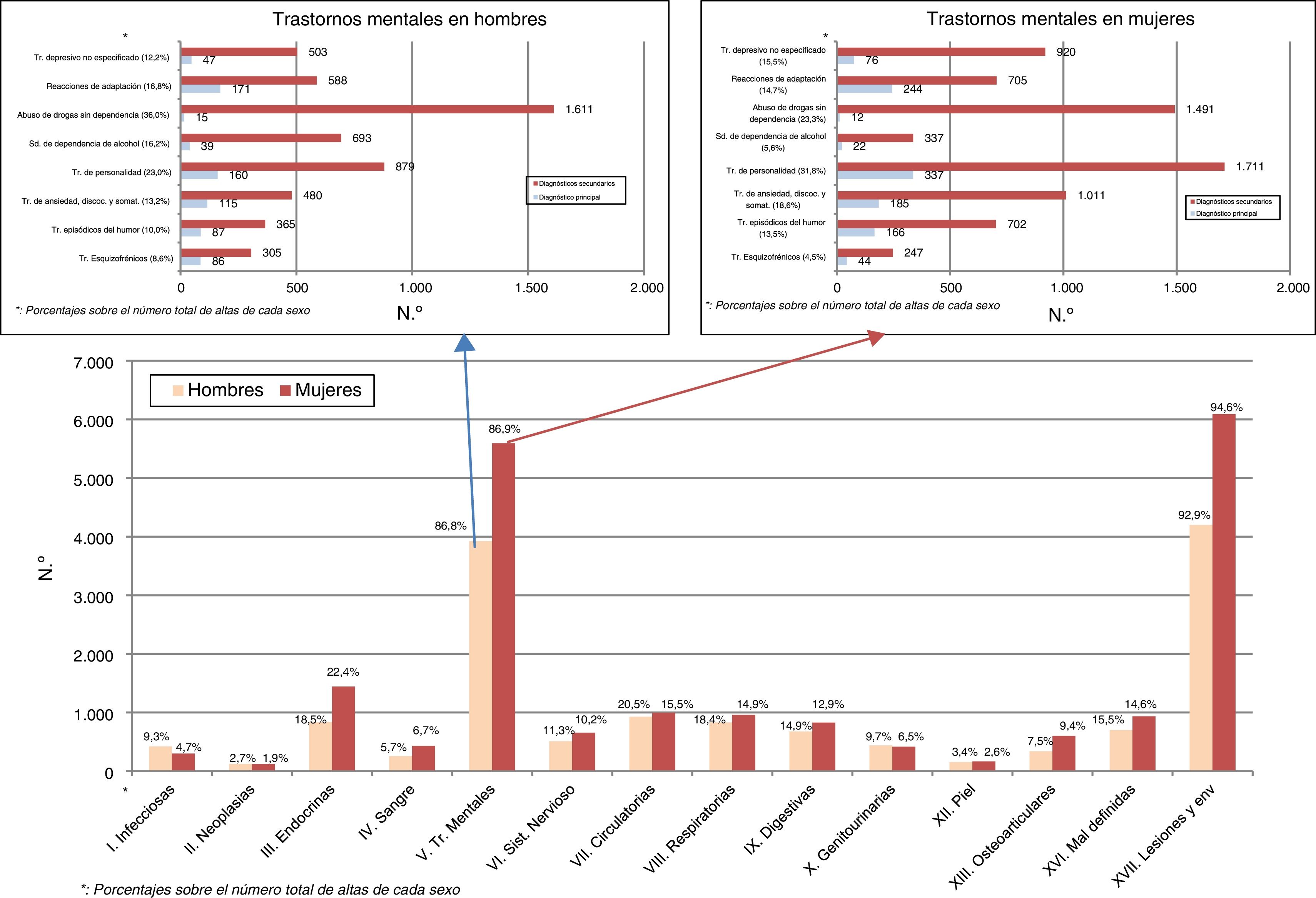
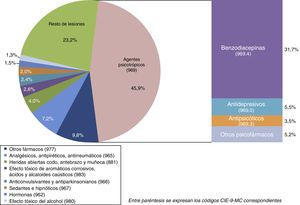
Injuries and poisoning in more than 90%, followed by mental disorders in more than 85%, were the major sources of morbidity in the main and secondary diagnoses compared to the other chapters of ICD-9-MC. Recording mental disorder in secondary diagnoses was very much higher than in the main diagnosis for the principal pathological groups, and in both sexes. Nondependent drug abuse in men (36.0%) and personality disorders in women (31.8%) were the most frequent headings (Fig. 2).
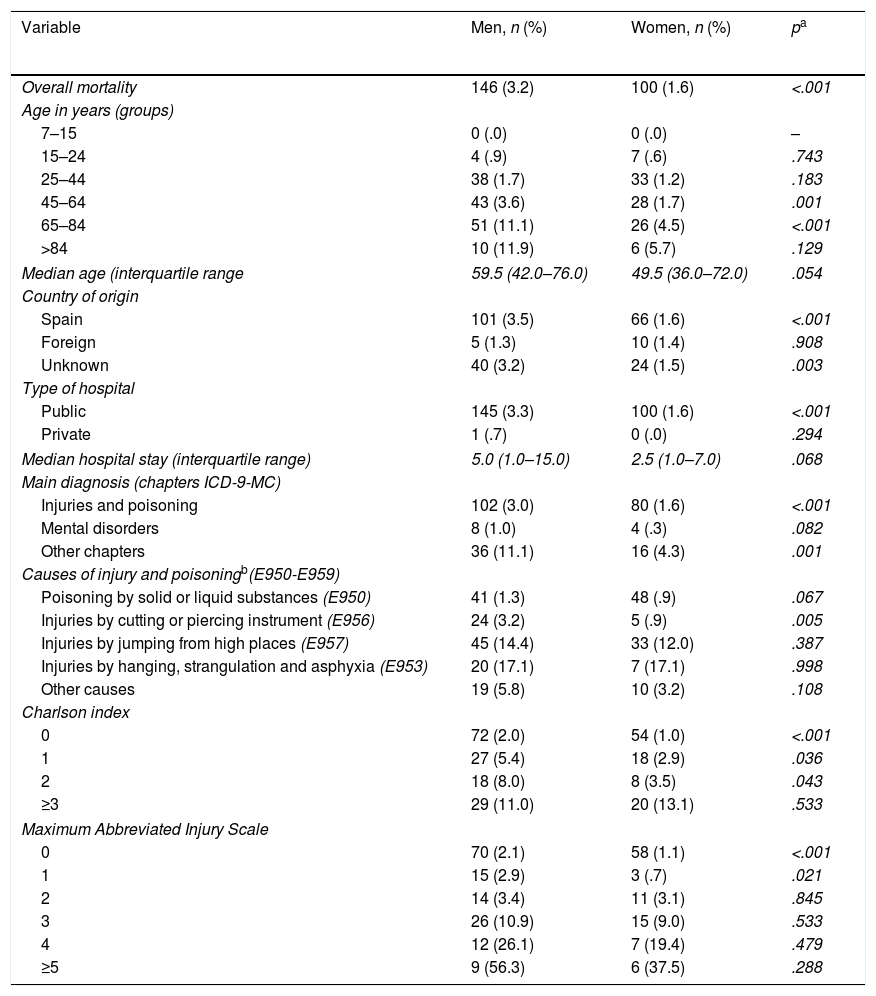
In-hospital mortality rose according to increased age in both sexes, especially from the age of 65, and was higher in men in all the categories. We found significant differences in the groups aged from 45–64 years (3.6% vs. 1.7%; p=.001) and 65–84 years (11.1% vs. 4.5%; p<.001) (Table 2). The median age of death was 10 years older in the men (59.5 vs. 49.5 years; p<.054). Men of Spanish origin and from unknown countries had the highest mortality rate, above that of women (3.5% vs. 1.6% [p<.001] and 3.2% vs. 1.5% [p=.003], respectively). Mortality in public hospitals was higher than in the private sector, and higher for men than women (3.3% vs. 1,6%; p<.001).
In-hospital mortality according to sociodemographic, clinical and healthcare variables, by sex in the selection Suicide and self-inflicted injuries (E950-E959) in the diagnostic fields of the minimum basic data set on hospital admission of the Community of Madrid, 2003–2013 (noverall=10,959; ndeath=246).
| Variable | Men, n (%) | Women, n (%) | pa |
|---|---|---|---|
| Overall mortality | 146 (3.2) | 100 (1.6) | <.001 |
| Age in years (groups) | |||
| 7–15 | 0 (.0) | 0 (.0) | – |
| 15–24 | 4 (.9) | 7 (.6) | .743 |
| 25–44 | 38 (1.7) | 33 (1.2) | .183 |
| 45–64 | 43 (3.6) | 28 (1.7) | .001 |
| 65–84 | 51 (11.1) | 26 (4.5) | <.001 |
| >84 | 10 (11.9) | 6 (5.7) | .129 |
| Median age (interquartile range | 59.5 (42.0–76.0) | 49.5 (36.0–72.0) | .054 |
| Country of origin | |||
| Spain | 101 (3.5) | 66 (1.6) | <.001 |
| Foreign | 5 (1.3) | 10 (1.4) | .908 |
| Unknown | 40 (3.2) | 24 (1.5) | .003 |
| Type of hospital | |||
| Public | 145 (3.3) | 100 (1.6) | <.001 |
| Private | 1 (.7) | 0 (.0) | .294 |
| Median hospital stay (interquartile range) | 5.0 (1.0–15.0) | 2.5 (1.0–7.0) | .068 |
| Main diagnosis (chapters ICD-9-MC) | |||
| Injuries and poisoning | 102 (3.0) | 80 (1.6) | <.001 |
| Mental disorders | 8 (1.0) | 4 (.3) | .082 |
| Other chapters | 36 (11.1) | 16 (4.3) | .001 |
| Causes of injury and poisoningb(E950-E959) | |||
| Poisoning by solid or liquid substances (E950) | 41 (1.3) | 48 (.9) | .067 |
| Injuries by cutting or piercing instrument (E956) | 24 (3.2) | 5 (.9) | .005 |
| Injuries by jumping from high places (E957) | 45 (14.4) | 33 (12.0) | .387 |
| Injuries by hanging, strangulation and asphyxia (E953) | 20 (17.1) | 7 (17.1) | .998 |
| Other causes | 19 (5.8) | 10 (3.2) | .108 |
| Charlson index | |||
| 0 | 72 (2.0) | 54 (1.0) | <.001 |
| 1 | 27 (5.4) | 18 (2.9) | .036 |
| 2 | 18 (8.0) | 8 (3.5) | .043 |
| ≥3 | 29 (11.0) | 20 (13.1) | .533 |
| Maximum Abbreviated Injury Scale | |||
| 0 | 70 (2.1) | 58 (1.1) | <.001 |
| 1 | 15 (2.9) | 3 (.7) | .021 |
| 2 | 14 (3.4) | 11 (3.1) | .845 |
| 3 | 26 (10.9) | 15 (9.0) | .533 |
| 4 | 12 (26.1) | 7 (19.4) | .479 |
| ≥5 | 9 (56.3) | 6 (37.5) | .288 |
The presence of “Other chapters” other than “Injuries and poisoning” and “Mental disorders” of ICD-9-MC in the main diagnosis showed the highest rates of mortality (11.1% for men vs. 4.3% for women; p=.001), whereas mental disorders showed the lowest values (1.0% for men vs..3% for women; p=.082). Precipitation and strangling as causes of injury presented figures above 12%, with significantly higher mortality in men from injuries from cutting instruments (3.2% vs. .9%; p=.005). The lowest mortality was from poisoning from substances. The mortality rose with an increased Charlson Index and MAIS score. There was significantly higher mortality in men in the 3 first categories of the former, and the 2 first categories of the latter (Table 2).
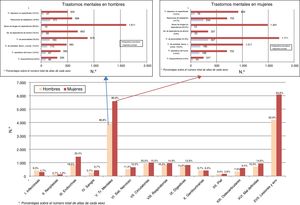
Consistently for both sexes, the variables: age (ORm: 1.03, ORw: 1.02), Injuries by hanging (ORh: 6.94, ORm: 44.32), precipitation injuries (ORm: 6.90, ORw: 17.56), nervous system diseases (ORm: 2.91, ORw3.29), respiratory diseases (ORm: 3.25, ORw: 3.17) and ill-defined diseases (ORm: 2.53, ORw: 2.96), and MAIS from category 3 were associated with a greater risk of mortality, whereas hospital stay (ORm: .95, ORw: .93) and mental disorders (ORm: .30, ORw: .31) acted as protective factors in the multivariate analysis. The public hospital variables (ORm: 11.97), neoplasms (ORm: 3.20) and digestive diseases (ORm: 2.27) were associated with a greater probability of death only in the men, and other mechanisms of injury (ORw: 2.56) and Charlson Index (category 3) (ORw: 12.49) were associated differentially in women. Poisoning with substances only had a protective effect in men (ORm: .31), whereas infectious diseases increased the risk in men (ORm: 2.41), but reduced it in women (ORw: .25) (Table 3).
Logistical regression analysis (backward stepwise). Dependent variable: mortality; independent variables retained in the final model.
| Men (n=4522) | Women (n=6437) | |||||
|---|---|---|---|---|---|---|
| Variable | ORh | Confidence intervals (95%) | ORw | Confidence intervals (95%) | ||
| Lower | Higher | Lower | Higher | |||
| Age | 1.03 | 1.02 | 1.04 | 1.02 | 1.01 | 1.04 |
| Hospital stay | .95 | .93 | .97 | .93 | .91 | .95 |
| Type of hospitala | 11.97 | 1.30 | 110.10 | – | – | – |
| Causes of injury or poisoning | ||||||
| Injuries by hanging, strangulation and asphyxia | 6.94 | 3.17 | 15.18 | 44.32 | 15.35 | 127.91 |
| Poisoning by solid or liquid substances | .31 | .16 | .59 | – | – | – |
| Injuries by jumping from high places | 6.90 | 3.73 | 12.76 | 17.56 | 7.47 | 41.27 |
| Other mechanism of injury | – | – | – | 2.56 | 1.16 | 5.64 |
| Comorbidities on main or secondary diagnosis | ||||||
| Infectious diseases | 2.41 | 1.42 | 4.10 | .25 | .09 | .69 |
| Neoplasms | 3.20 | 1.66 | 6.16 | – | – | – |
| Mental diseases | .30 | .20 | .45 | .31 | .19 | .50 |
| Nervous system diseases | 2.91 | 1.83 | 4.62 | 3.29 | 1.94 | 5.59 |
| Respiratory diseases | 3.25 | 2.08 | 5.08 | 3.17 | 1.88 | 5.35 |
| Digestive diseases | 2.27 | 1.42 | 3.62 | – | – | – |
| Ill-defined diseases | 2.53 | 1.63 | 3.92 | 2.96 | 1.73 | 5.06 |
| Charlson Indexa | ||||||
| 1 | – | – | – | 1.46 | .73 | 2.90 |
| 2 | – | – | – | 1.63 | .65 | 4.09 |
| 3 | – | – | – | 12.49 | 5.76 | 27.11 |
| Maximum Abbreviated Injury Scalea | ||||||
| 1 | .76 | .35 | 1.62 | .77 | .22 | 2.66 |
| 2 | .65 | .30 | 1.42 | 2.12 | .92 | 4.86 |
| 3 | 2.58 | 1.25 | 5.33 | 4.36 | 1.63 | 11.66 |
| 4 | 3.42 | 1.22 | 9.54 | 8.36 | 2.40 | 29.19 |
| 5 | 17.84 | 4.71 | 67.49 | 25.79 | 5.76 | 115.54 |
Our results indicate that suicidal behaviour attended in CM hospitals is more common in women and in middle-age. Their mortality is principally associated with increased age, severity of injury, and the patient's comorbidity. We found differences in descriptive variables, and in those related to mortality between both sexes.
Various factors affect admission to hospital after attempted suicide. Advanced age, living alone, methods of self-injury that do not involve drug overdose, a previous history of suicidal behaviour and psychiatric diagnoses of schizophrenia, mood or personality disorder have been detected as independent factors associated with admission to hospital.13 Other research studies have highlighted other explanatory factors, such as a delay until discovery of more than one hour; previous attempts; suicidal ideation; high suicidal planning; and lack of verbalisation of adequate criticism of the attempt.14 Other authors have identified the information provided by the patients themselves, more than a consideration of diagnostic, demographic or psychosocial aspects as a crucial element in the decision to hospitalise by psychiatrists.15
Although hospitalisation currently remains the main therapeutic strategy in the management of suicidal behaviour, it is appropriate to assess its potential iatrogenic effects. Facilitation of stigma, low perceived self-efficacy, breakdown in therapeutic alliance, and possible strengthening of non-fatal self-harm are factors that should be considered.16 Similarly, a controversial aspect is the admission of some types of personality disorders, since this might cause a greater risk of recurrence of parasuicidal behaviour; this aspect is not confirmed by all authors.17
In this regard, differential management has been suggested according to clinical profile, which would enable the use of more or less intensive and specialist resources adapted to the specific situation. Thus, patients admitted to intensive care would have profiles and needs that are very different from those who are routinely not hospitalised with repeated parasuicidal behaviours.18
Of all the factors involved in suicide, the presence of a mental disorder is the most frequent finding, and varies according to the specific diagnosis. Under the age of 35, schizophrenia and borderline personality disorder cause the most incidents, whereas alcoholism in middle age, and reactions to stress and adjustment disorders in the elderly are the main predictors of suicide risk.19 In terms of completed suicide, schizophrenia and severe mood disorders are most associated with mortality.20
Depressive disorders are the main predictive factor of death due to this cause,21 and there are major differences in terms of age, associated with higher mortality, both by suicide and by somatic diseases, when they occur at an advanced age.22 Because of their relationship, depressive symptoms must be investigated if there is a simultaneous chronic disease. The beliefs of the patient him or herself about depression are an essential element in establishing appropriate detection strategies for these patients.23 Other disorders associated with depression, such as substance consumption, result in a greater number and severity of suicidal acts.24
In line with our results, we found that physical disease in itself, irrespective of mental disorders and unfavourable socioeconomic factors, is a risk factor for suicide.25 Some aspects relating to physical disease, such as self-perceived physical health, and amount of chronic diseases and pain-generating diseases have been associated with a higher desire for death in the elderly population, which underlines the importance of appropriate preventive assessment of the suicide risk in every area of healthcare.26
Some of the characteristics of suicidal behaviour that we observed in our study are similar to those of other research studies, with a predominance of women and young and middle- aged people in nonfatal self-inflicted injuries.9 In this study, many of the differences found between men and women were associated with the different psychopathological expressivity of each sex. Thus, internalising disorders (mood and anxiety), more common in women, are associated with high suicide attempts, whereas externalising disorders (substance abuse and behavioural disorders), more prevalent in men, are associated with higher fatality. This finding is also reflected in the different mortality found between the sexes in our paper. Without doubt, this factor impacts other variables, such as the age of presentation, chosen method and, consequently, the degrees of harm and comorbidity detected.27
Substance intake is the main method used in attempted suicide in developed countries, particularly psychotropic drugs, which we also found in our study. The benzodiazepines were the majority within this group of drugs in our study, followed by antidepressants. An explanatory factor is the easy access and availability of these types of substances in our environment due to their extensive and trivialised use beyond the appropriate clinical indications and criteria. Therefore, a key current preventive strategy would be to limit direct access to these drugs where there is a suicide risk.28
We can consider that in-hospital mortality is related to, firstly, the mechanism of injury depending on the method used, the most aggressive methods are those associated with higher mortality since they cause more severe injuries and vice versa, and this is related to the results found when applying the injury severity scale. Secondly, comorbidity, which is already present or a consequence of the injuries sustained, is a major risk factor, associated with diseases of different organs and systems, although with differences between both sexes under the headings of neoplasms, infectious and digestive diseases, and Charlson Index. This would require more detailed analysis. In this regard, some researchers have detected risks of death that are doubled for self-inflicted injuries compared to unintentional injuries in intensive care units, adjusting by age and level of severity of the injury, which supports a differential and intrinsic effect of these type of injuries.29
Other factors relating to a greater probability of death are increased age, probably related to greater physical vulnerability, and admission to a public hospital, only observed in men, possibly associated with greater clinical severity. Conversely, a longer hospital stay and poisoning by substances, both indicative of greater survival, behave logically as protective factors. The protective effect detected for mental disorder is more difficult to explain, and might be paradoxical. In this regard, we highlighted the presence in clinical and administrative databases of an information sub-record on a history of chronic illness in the most severe patients who died, which leads to spurious protective behaviour with regard to in-hospital mortality in the statistical models.30
Our results indicate that suicidal behaviour presents a main diagnosis of mental disorder in less than 20% of patients admitted, which represents a prioritisation of diagnostic coding for the methods and organic injuries that occur. However, also bearing in mind the presence of mental disorder in secondary diagnoses, 87% have some type of disorder. In the obvious relationship between suicide and mental illness,31 current research studies have detected methodological differences on psychological autopsy, the method routinely used to clarify underlying factors.32 Beyond psychiatric disease itself, we feel that worry and shame, barely consulted or recognised in terms of care, might be factors involved in a great many suicidal behaviours with no history of mental disorder.
This study only shows a small part of suicide-related mortality—in-hospital mortality—and does not consider mortality prior or subsequent to discharge from hospital. We confirmed an elevated risk during this latter period if the patient has a mental disorder, particularly during the first weeks of a mood disorder, in the knowledge that a quarter of suicide victims have been admitted the year before with a mental disorder.33
Another limitation of our study, in addition to the impossibility of establishing causal relationships because it was cross-sectional, is the difficulty in distinguishing between underlying physical diseases and those causing the suicide attempt itself. For example, anoxic brain damage, the most frequently detected injury in nervous system diseases, is probably a consequence of the suicidal act itself, whereas neoplasms are difficult to attribute to the episode and might, in any case, relate to its genesis.
Added to this difficulty are some characteristics particular to the MBDS, with a database extracted from the discharge report, with possible variability between hospitals in terms of the exhaustive nature of information, compliance, coding, quality and specificity of the available clinical variables, which leads to the possibility of common errors in the management of clinical and administrative databases.34 Despite these limitations, MBDS remains a useful tool for developing clinical and epidemiological studies.
A strength of our study is the use for the first time of an injury severity scale, originally designed to assess road traffic accidents that achieves good adjustment and logical association between severity and mortality, which makes it a useful tool for the future until more specific instruments are developed.
This paper explores a specific aspect of suicidal behaviour such as that related to hospitalisation, showing differences in presentation and fatality by sex, with low overall mortality, principally associated with the severity of injuries and presence of comorbidities. These results might be relevant in the exploration of more specific aspects and population sub-groups at greater risk.
It is necessary to continue advancing our understanding of suicide from a global approach that considers all its elements and dimensions, with the ultimate goal of a reduction in its levels, and appropriate prevention. In this regard, we raised the possibility of creating a national preventive strategy to achieve effective and measurable results beyond a mere declaration of intentions.35
Transparency declarationThe lead author, Juan Manuel Sendra-Gutiérrez, affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that there are no discrepancies from the study as planned.
Ethical responsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing has been carried out under this research.
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Privacy rights and informed consentThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sendra-Gutiérrez JM, Esteban-Vasallo M, Domínguez-Berjón MF. Características de la conducta suicida y factores asociados a su mortalidad en el ámbito hospitalario. Rev Psiquiatr Salud Ment (Barc.). 2018;11:234–243.