Breast cancer is the main cause of cancer-related death in women and almost all related deaths occur due to metastasis. The most frequent places of metastasis are lymph nodes, bone, lung, liver, and central nervous system. Bladder metastasis are very rare, being described in only 7% of autopsy studies. Besides being uncommon, most cases of secondary bladder involvement occur as a result of disseminated disease, being the solitary bladder metastasis sporadically reported.
This article presents the case of a woman with a history of invasive lobular breast carcinoma who, 18 months after diagnosis, presents herself with complaints of urinary urgency and urinary incontinence. The requested complementary exams revealed a voluminous bladder mass and the anatomopathological study was compatible with a metastatic lesion.
El cáncer de mama es la principal causa de muerte relacionada con el cáncer en las mujeres y casi todas las muertes relacionadas se producen por metástasis. Los lugares más frecuentes de metástasis son los ganglios linfáticos, los huesos, los pulmones, el hígado y el sistema nervioso central. Las metástasis vesicales son muy raras, describiéndose sólo en el 7% de los estudios de autopsia. Además de ser poco común, la mayoría de los casos de afectación vesical secundaria ocurren como resultado de una enfermedad diseminada, siendo la metástasis vesical solitaria reportada esporádicamente.
Este artículo presenta el caso de una mujer con antecedentes de carcinoma lobulillar invasivo de mama que, 18 meses después del diagnóstico, presenta síntomas de urgencia urinaria e incontinencia urinaria. Los exámenes complementarios solicitados revelaron una masa vesical voluminosa y el estudio anatomopatológico fue compatible con lesión metastásica.
Breast carcinoma is one of the most frequent malignant tumors in females.1 The most common histological type is non-special type invasive carcinoma/NST (50%–75%), formerly called invasive ductal carcinoma, followed by invasive lobular carcinoma/ILC in 5%–15% of cases.2 Patients are at risk for the development of distant metastasis, even after long periods of remission.3 Local or distant recurrence of ILC is estimated to occur in 30% of cases during follow-up after initial treatment. Different metastatic patterns have been described between the 2 histological types.3 Dissemination to exceptional locations such as the peritoneum, meninges, and gastrointestinal tract seems to be more frequent in the latter.4 The occurrence of bladder metastasis in breast carcinoma is a very rare situation, with few cases described in the literature.5 This article reports a case of bladder metastasis from invasive lobular carcinoma 18 months after the initial diagnosis.
CaseA 74-year-old woman, with irrelevant personal and family history, under surveillance in a Senology Unit for locally advanced invasive cancer of the left breast. At diagnosis, she had retroareolar nodular swelling, nipple invagination, and suspicious axillary and supraclavicular lymph nodes—clinical stage cT3 N3c. A microbiopsy of the breast lesion revealed invasive lobular carcinoma (grade 2, luminal A, negative Cerb-B2 with 10% Ki67), and that of the axillary lymph nodes confirmed metastasis. An aspiration puncture of the supraclavicular node was also performed, with cytology suspected of carcinoma metastasis. Staging exams suggested secondary bone involvement in the right clavicle and 5th lumbar vertebra, not showing other sites of metastasis.
Despite being M1, the patient had oligometastatic bone disease but with a high local tumor burden. Afraid that the local disease would progress quickly, it was decided to start neoadjuvant chemotherapy to try to achieve a faster local response. Despite chemotherapy (4 cycles of docetaxel and cyclophosphamide), the locoregional disease continued to progress. The same did not happen with metastatic disease, evidenced by the disappearance of bone lesions described in the positron emission tomography (PET) scan performed after chemotherapy. It was therefore decided to do a radical salvage mastectomy with the aim of local control of the disease that was unresponsive to chemotherapy and progressing. Post-surgical histopathological examination revealed a grade 2 invasive lobular carcinoma, unresponsive to neoadjuvant treatment (residual cancer burden/RCB III)—stage ypT3N3a (20 positive nodes out of 25 isolated), with lymphatic and perineural invasion, without vascular invasion. She started adjuvant hormone therapy with tamoxifen and received radiotherapy on the left chest wall and also on the ipsilateral axillary–supraclavicular lymph nodes (total dose 52 Gy), given that the supraclavicular fossa had not been approached surgically.
In one of the follow-up consultations and 18 months after the initial diagnosis, the patient reported polyakiuria, urinary urgency, and urinary incontinence, so she was referred to a Urology consultation. On physical examination, bimanual palpation was questionable regarding bladder mobility. Bladder ultrasound and contrast-enhanced thoracoabdominopelvic computed tomography (CT) were requested. Complementary diagnostic tests revealed ectasia of the excretory tree on the left with thickening of the ureter, particularly in the pelvic location, and an extensive filling defect of the ipsilateral lateral bladder wall (marked by red arrows; Fig. 1). No other findings were reported in the remaining organs and systems.
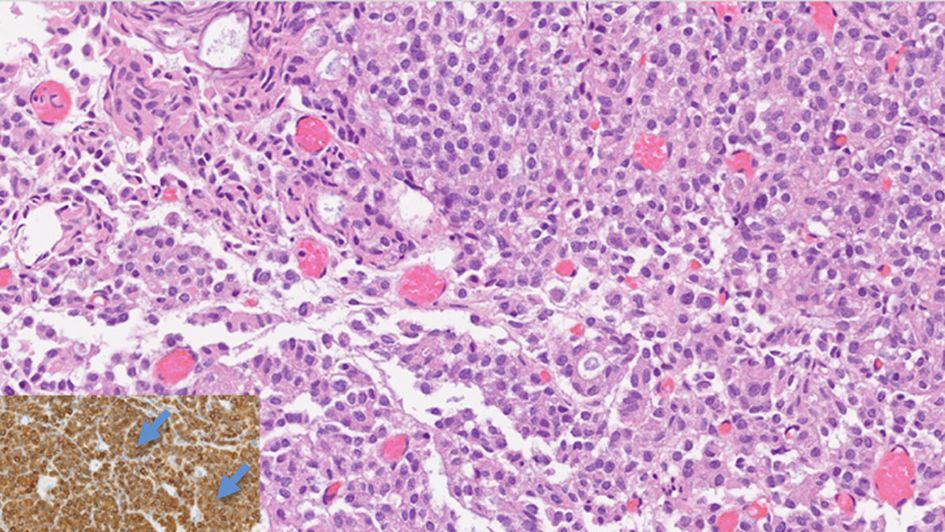
According to the previous describing findings, cystoscopy with bladder incisional biopsy was performed. The sample, consisting almost exclusively of malignant epithelial neoplasia, showed expression for CKAE1/AE3, CK7, GATA3, mammoglobin, and estrogen receptor (focal and weak) and was negative for CK20, progesterone receptor, Cerb-B2, synaptophysin, and chromogranin (Fig. 2). Therefore, the morphological and immunohistochemical aspects of the lesion described, corresponding to bladder parietal thickening, were compatible with metastasis of invasive lobular carcinoma.
Bladder infiltration by a malignant epithelial tumor, with solid, cribriform and discohesive areas, occasionally forming lines, composed by monomorphic cells (H&E; original magnification 40×). Inlet: The tumor was positive for mammoglobin immunohistochemical marker (highlighted by blue arrows), supporting breast origin.
The case was discussed in a multidisciplinary team and the patient was proposed to start systemic therapy with palbociclib (125 mg/day for 21 consecutive days, followed by a 7-day break), in addition to hormonal therapy with letrozole (2.5 mg/day).
DiscussionAbout 45% of breast tumors metastasize and tumor cells can reach virtually any organ. In patients with metastatic breast cancer, 30%–60% have bone lesions, 21%–32% lung lesions, 15%–32% liver lesions, and 4%–10% brain lesions.6 Bladder metastasis are rare, being reported in literature occasionally with necropsy studies describing incidences up to 7%.6
It is thought that the pattern of breast cancer metastasis may be related to the histological type, with bladder metastasis being more common in ILC.3,5 The metastatic pattern of ILC differs from that of the NST in that the former tends to occur as a diffuse thickening of the mucosa rather than an isolated lesion. In fact, the greater propensity of lobular carcinoma to metastasize to serous surfaces (such as the gastrointestinal or gynecological tract) may explain its higher rate of bladder involvement.
With regard to the clinical presentation, it ranges from asymptomatic to painless macroscopic hematuria (the most frequent symptom), obstructive uropathy, and/or renal failure. Furthermore, detrusor involvement may lead to irritative voiding symptoms and may manifest prior to hematuria.5 In fact, the appearance of macroscopic hematuria and/or urinary symptoms in a patient with a history of breast cancer should lead to careful clinical investigation.7
In the physical examination, it is essential to perform a rectal evaluation and bimanual examination, to exclude advanced and invasive disease, such as a palpable pelvic/hypogastric mass. Regarding complementary diagnostic tests, the ultrasound is the first-line test indicated in patients with breast cancer and urinary tract symptoms.8 Contrast-enhanced CT can be useful for assessing local and distant disease.8 Additionally, cystoscopy should be performed to confirm the presence of lesions and allow defining their characteristics such as number, size, and appearance (papillary, sessile, or flat).5 In this exam, biopsies, excision of some lesions, and collection of vesical lavage for cytological study can be performed. It should be noted that if no lesion is observed but the diagnostic suspicion is high, random bladder biopsies may be justified.9
After confirming the diagnosis of bladder metastasis, transurethral resection of the lesion must be performed. This procedure will also facilitate the placement of a ureteral stent in case of obstruction. Regarding treatment, CDK4/6 inhibitors are drugs approved for use in metastatic or locally advanced breast cancer with hormone receptor positive and Cerb-B2 negative and should be used in combination with an aromatase inhibitor or in combination with fulvestrant (in women who have received previous endocrine therapy). Another option is the isolated use of chemotherapy.5 If hematuria is present, radiotherapy can be used to control this symptom.
In the case of this patient, before the detection of bladder metastasis and given the good local control and the disappearance of the initial bone oligometastatic disease, tamoxifen10 was chosen as adjuvant hormone therapy. Only with the progression of the metastatic disease did it become clear that tamoxifen therapy was not sufficient and the therapeutic regimen was changed to letrozole10 together with a CDK inhibitor.10
The prognosis, owing to few published cases, is still uncertain. If, on the one hand, there are studies that claim that the prognosis of breast cancer with bladder metastasis is similar to that of cases with metastatic involvement from other sites, on the other hand, there are authors who argue that bladder metastasis have a worse prognosis than bone metastasis considering that the first is usually detected at a later stage.5,11 Another aspect to be taken into account is the fact that most bladder metastasis appear as a result of disseminated disease, which negatively affects survival. In contrast, isolated bladder metastasis showed an increase in disease-free survival after treatment.5,12 In the case of this patient and until today remains the control of the locoregional disease. The control of bladder metastatic disease has been slow with hormone therapy and CKD inhibitor, however, allowing symptomatic and quality of life improvements.
In short, despite the fact that bladder metastasis from breast neoplasms is an infrequent phenomenon, the appearance of painless hematuria or irritating voiding symptoms together with the finding of focal or diffuse bladder thickening should imply the diagnosis of metastatic disease.
FundingThere are no funding sources.
Ethical considerationsThis clinical case report has been made of a patient treated in a Senology Unit, keeping the patient's identification data confidential, being approved for publication by the Institution's Research Ethics Committee.
Patient consentThe authors declare that the patient's consent has been obtained for the publication of this article.