To present the epidemioclinical features, the immunohistochemical profile and the overall survival rate of women over 65 with breast cancer.
Materials and methodsIn a retrospective study, we recruited women over 65 years old with breast cancer who were treated in the district of Abidjan. Our study took place in a period of 60 months, from 2014 until 2018. The patients were selected from several sources; namely the consultation's registers, the hospitalization's units, the operating theater and the archive files of all the above. The data were collected using a survey sheet, processed then analyzed from the Epi info7 software. The Kaplan–Méier test helped us appreciate the survival.
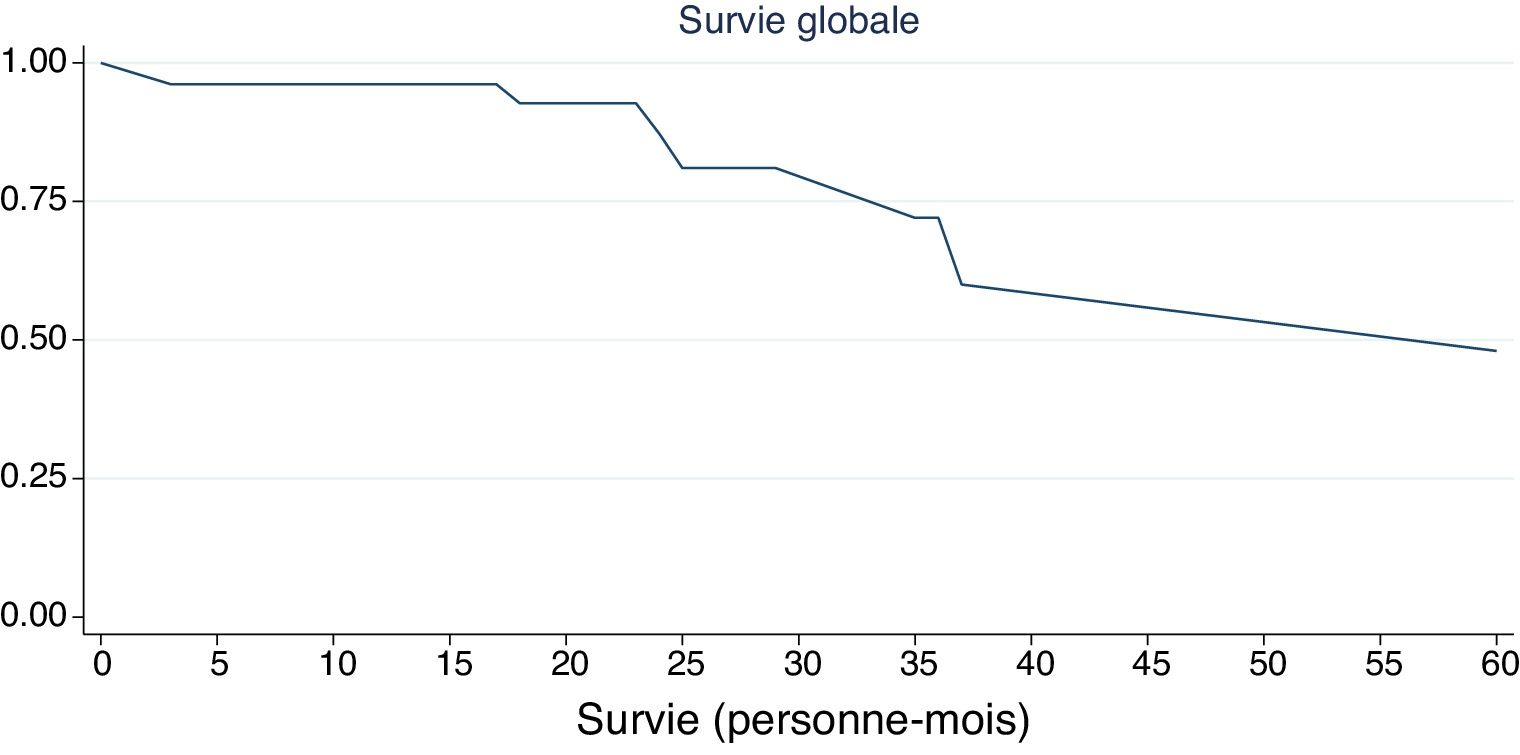
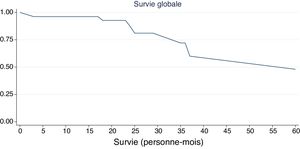
ResultsFrom a total of 2233 breast cancers, we got 52 patients over the age of 65, i.e. a proportion of 9.53%. These patients’ age range was between 65 and 86 years old with an average age of 72 years old. The non-specific invasive carcinoma represented the most frequent histological type with 94.23% of the cases. 1 out of 2 women (56.41%) received a neoadjuvant chemotherapy. The overall survival rate for 5 years were 9.62%. The median survival of the patients was 15.50 months. The immunohistochemical profile was determined for 21 patients and among them there was no Luminal B Her 2- and the Luminal A (43%) was the dominant profile.
ConclusionThe management of elderly Ivoirian breast cancer was essentially non-surgical with a low survival.
Presentar las características epidemiológicas, el perfil inmunohistoquímico y la tasa de supervivencia global de mujeres mayores de 65 años con cáncer de mama.
Materiales y métodosEn un estudio retrospectivo, reclutamos mujeres mayores de 65 años con cáncer de mama que fueron tratadas en el distrito de Abiyán, Costa de Marfil. Nuestro estudio se llevó a cabo en un periodo de 60 meses, desde 2014 hasta 2018. Las pacientes fueron seleccionadas de varias fuentes; a saber, los registros de consulta, las unidades de hospitalización, el quirófano y los archivos de todos los anteriores. Los datos se recopilaron mediante una hoja de encuesta, se procesaron y luego se analizaron desde el software Epi Info 7 (version 7.2.1.0). La prueba de Kaplan-Meier nos ayudó a apreciar la supervivencia.
ResultadosDe un total de 2.233 cánceres de mama, obtuvimos 52 pacientes mayores de 65 años, es decir, una proporción del 9,53%. El rango de edad de estas pacientes estaba entre los 65 y los 86 años, con una edad promedio de 72 años. El carcinoma invasivo inespecífico representó el tipo histológico más frecuente, con el 94,23% de los casos. Una de cada dos mujeres (56,41%) recibió quimioterapia neoadyuvante. La tasa de supervivencia global durante cinco años fue del 9,62%. La mediana de supervivencia de las pacientes fue de 15,50 meses. Se determinó el perfil inmunohistoquímico para 21 pacientes, y entre ellas no hubo Luminal B Her2− y el Luminal A (43%) fue el perfil dominante.
ConclusiónEl tratamiento del cáncer de mama de Costa de Marfil de edad avanzada fue esencialmente no quirúrgico, con una baja supervivencia.
Nowadays the management of breast cancer is personalized due to its number varieties, hence its genomic and molecular classification.1–3 Breast cancers account for 25% of all women's cancer.4 In fact, this incidence increases with age and reaches 400/100,000 women from 65 years old and above.5 In 2016, the incidence of breast cancer in women over 65 was 436.9 for 100,000 per year.1,2 The World Health Organization and Medicare define older people as women over 65 years old.2,3 In terms of mortality, breast cancer is responsible for 11,000 deaths per year that to say 16.2/100,000 women, according to standardized data on the world's population.5 In Côte d’Ivoire, according to data from the cancer registry of Abidjan, the incidence and mortality associated with breast cancer are constantly increasing, respectively going from 21.4 to 33.7 per 100,000 women in 1997 to 2012.6
The diagnostic period is generally long due to several intertwined factors (cultural, socio-economic, political) concerning both the patient and the healthcare system in our countries. Unlike in Western countries, this age group of the female population attend less the healthcare centers. In Côte d’Ivoire, there are few data on the socio-demographic, genetic and molecular characteristics of breast cancers affecting the elderly women.
Therefore, presenting the various epidemiological, clinical, immunohistochemical and therapeutic aspects of breast cancers in women above 65 years old will be the aim of our study.
Materials and methodsStudy designThis was a descriptive cross-sectional study that looked at women with breast cancer from 2014 to 2018, that to say over a period of 60 months. Our study took place in the public services which take care of women with breast cancers in the district of Abidjan, namely the Gynecology-Obstetrics services of the Teaching Hospital of Yopougon, Treichville and Cocody, as well as the oncology department of the Teaching Hospital of Treichville. The anatomical pathology laboratories of the Teaching Hospital of Treichville, Cocody and the central laboratory of Plateau.
The histological diagnosis for some of the cases were carried out in the anatomical pathology department of the Teaching Hospital from a micro-biopsy, lumpectomy or mastectomy specimen. Then, the paraffin blocks or the samples were for some cases sent to the central anatomical pathology laboratory of Plateau for the hormonal receptors (HR) dosage and to look for the HER2. Three antibodies were used: estrogen receptors (OR) (clone SP1), progesteron receptors (PR) (clone 1E2), HER2/neu (clone 4B5). The overexpression of the oncoprotein HER2 is considered positive for a 2+ and 3+ score according to the recommendations of the evaluating group of prognostic factors by immunohistochemistry in breast cancer (GEFCI).6 The prognostic index value Ki 67 in percentage with a limit of 15% helped us determined five molecular subtypes, Luminal A, Luminal B (HER2− and HER2+), non-Luminal HER2+ and triple negative or basal like carcinoma.
Study populationWe included in the study all the patients above 65 years old at the moment of the histological diagnosis of the breast carcinoma, which gave their free and informed consent or that of their right holders. In contrast, those lost to follow-up and the patients whose questionnaires had incomplete items for any reason were not selected. In the literature the studies concerning the elders are above 65, 70 or even 75 years. We chose the minimum age of 65 as the cut off in our study given that life expectancy in Côte d’Ivoire is in general 57.4 years and particularly 58.7 years for women,7 hoping to have a large workforce.
Methods of investigationOur study interested patients above 65 years old with breast cancer. After our authorization request to investigate were accepted, our recruitment initially began in the pathology laboratories of Plateau and Cocody. Subsequently, patients who met our study criteria were identified as well as their healthcare center. The missing information on the files, namely the gynecologic and obstetric history, the treatment received and the survival, were completed by calling the patients after an explanation of the study and an oral consent. The cost of the phone calls was at our own expense. The average call time was 6min
Collection of dataThe patients were selected during the period of our survey, through the consultation, hospitalization, operating room registers, archives and laboratories of the aforementioned departments. Data was collected using a survey form. In addition to the classic socio-demographic and clinico-histological parameters, data on the different biologico-molecular types, therapeutic principles and survival were collected. Once the survey was completed, the data was processed and analyzed using the Epi info7 software. The Kaplan–Méier test made it possible to assess overall survival.
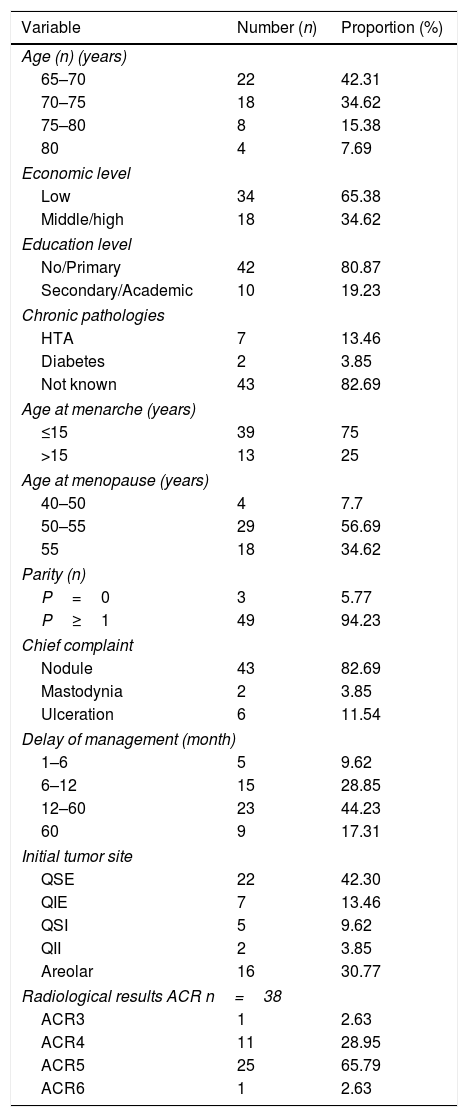
ResultsWe collected 52 cases of patients over 65 years old with breast cancer out of 2233 patients with breast cancer of all ages, i.e. 9.53%. These patients ranged from 65 to 86 years old with an average age of 72 years. Women without a fixed income, with a low socioeconomic status, without school education, represented respectively 65%, 86%, and 76% of our study population. The average age at menarche and menopause were 15 and 50 years respectively. 5.77% were nulliparous. The breast lump represented the most frequent reason for consultation (82.69%). 44.23% of our patients had consulted 1 year after the first sign. The upper outer quadrant was the most affected quadrant (42.30%). Among the patients who performed the mammography 65.79% were classified by American Classification of Radiology ACR 5 (Table 1).
Epidemiological features, consultation reason and delay, management delay, tumor site, ACR classification of 52 patients.
| Variable | Number (n) | Proportion (%) |
|---|---|---|
| Age (n) (years) | ||
| 65–70 | 22 | 42.31 |
| 70–75 | 18 | 34.62 |
| 75–80 | 8 | 15.38 |
| 80 | 4 | 7.69 |
| Economic level | ||
| Low | 34 | 65.38 |
| Middle/high | 18 | 34.62 |
| Education level | ||
| No/Primary | 42 | 80.87 |
| Secondary/Academic | 10 | 19.23 |
| Chronic pathologies | ||
| HTA | 7 | 13.46 |
| Diabetes | 2 | 3.85 |
| Not known | 43 | 82.69 |
| Age at menarche (years) | ||
| ≤15 | 39 | 75 |
| >15 | 13 | 25 |
| Age at menopause (years) | ||
| 40–50 | 4 | 7.7 |
| 50–55 | 29 | 56.69 |
| 55 | 18 | 34.62 |
| Parity (n) | ||
| P=0 | 3 | 5.77 |
| P≥1 | 49 | 94.23 |
| Chief complaint | ||
| Nodule | 43 | 82.69 |
| Mastodynia | 2 | 3.85 |
| Ulceration | 6 | 11.54 |
| Delay of management (month) | ||
| 1–6 | 5 | 9.62 |
| 6–12 | 15 | 28.85 |
| 12–60 | 23 | 44.23 |
| 60 | 9 | 17.31 |
| Initial tumor site | ||
| QSE | 22 | 42.30 |
| QIE | 7 | 13.46 |
| QSI | 5 | 9.62 |
| QII | 2 | 3.85 |
| Areolar | 16 | 30.77 |
| Radiological results ACR n=38 | ||
| ACR3 | 1 | 2.63 |
| ACR4 | 11 | 28.95 |
| ACR5 | 25 | 65.79 |
| ACR6 | 1 | 2.63 |
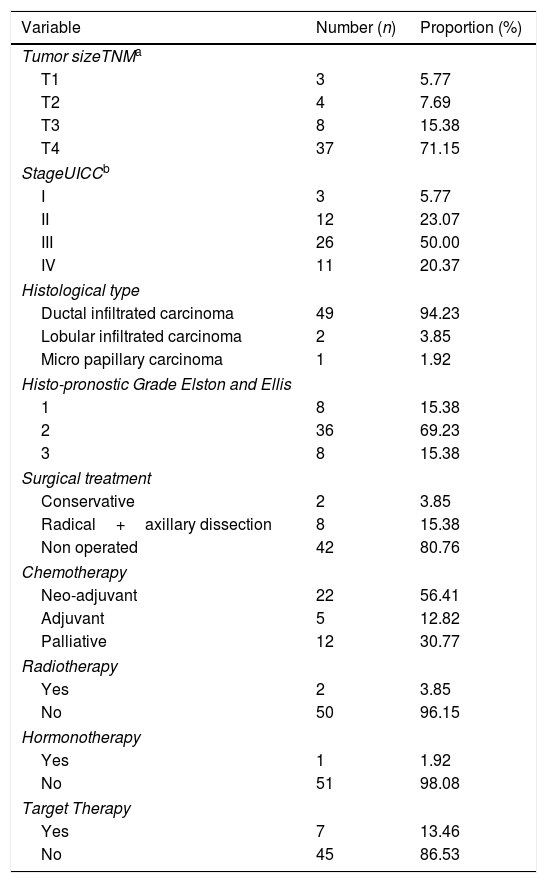
Among our patients 71.15% were diagnosed at stage T4 (TNM) and 20.37% were at stage IV (UICC). Invasive nonspecific carcinoma was the most frequent histological type with 94.23% of cases and 69.23% of women had grade 2 histopronostic. 1 out of 2 women (56.41%) had neo-adjuvant chemotherapy and 3.85% of women had performed radiotherapy. Only 1.92% had hormonal therapy. 13.46% of our patients had received targeted therapy (Table 2).
TNM tumor size, stage UICC, histological type, histopronostic grade of Elston and Ellis and management of 52 patients.
| Variable | Number (n) | Proportion (%) |
|---|---|---|
| Tumor sizeTNMa | ||
| T1 | 3 | 5.77 |
| T2 | 4 | 7.69 |
| T3 | 8 | 15.38 |
| T4 | 37 | 71.15 |
| StageUICCb | ||
| I | 3 | 5.77 |
| II | 12 | 23.07 |
| III | 26 | 50.00 |
| IV | 11 | 20.37 |
| Histological type | ||
| Ductal infiltrated carcinoma | 49 | 94.23 |
| Lobular infiltrated carcinoma | 2 | 3.85 |
| Micro papillary carcinoma | 1 | 1.92 |
| Histo-pronostic Grade Elston and Ellis | ||
| 1 | 8 | 15.38 |
| 2 | 36 | 69.23 |
| 3 | 8 | 15.38 |
| Surgical treatment | ||
| Conservative | 2 | 3.85 |
| Radical+axillary dissection | 8 | 15.38 |
| Non operated | 42 | 80.76 |
| Chemotherapy | ||
| Neo-adjuvant | 22 | 56.41 |
| Adjuvant | 5 | 12.82 |
| Palliative | 12 | 30.77 |
| Radiotherapy | ||
| Yes | 2 | 3.85 |
| No | 50 | 96.15 |
| Hormonotherapy | ||
| Yes | 1 | 1.92 |
| No | 51 | 98.08 |
| Target Therapy | ||
| Yes | 7 | 13.46 |
| No | 45 | 86.53 |
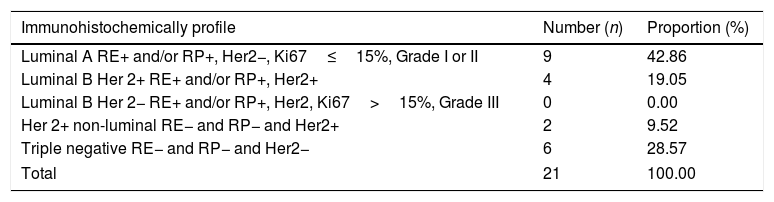
The immunohistochemical profile was determined in 21 patients and among them there was no Luminal B Her 2, and the Luminal A (43%) was the dominant profile (Table 3). Among the operated patients only two received conservative treatment.
Immunohistochemically profile of 21 elderly patients.
| Immunohistochemically profile | Number (n) | Proportion (%) |
|---|---|---|
| Luminal A RE+ and/or RP+, Her2−, Ki67≤15%, Grade I or II | 9 | 42.86 |
| Luminal B Her 2+ RE+ and/or RP+, Her2+ | 4 | 19.05 |
| Luminal B Her 2− RE+ and/or RP+, Her2, Ki67>15%, Grade III | 0 | 0.00 |
| Her 2+ non-luminal RE− and RP− and Her2+ | 2 | 9.52 |
| Triple negative RE− and RP− and Her2− | 6 | 28.57 |
| Total | 21 | 100.00 |
Our overall 5-year survival rate was 9.62%. The median survival of the patients was 15.50 months with extremes, ranging from 3 to 60 months (Fig. 1).
DiscussionAge is one of the main risk factors for breast cancer: more than 30% of all new breast cancers occur in women aged 65 and above. The incidence of breast cancer increases with age.8 Aging is often linked to frailty9,10 and is characterized by a decrease in physiological, psychological and social well-being11 and disturbed homeostasis after stress. Elderly patients generally some defects which constitute a greater burden of co-morbidity12 by making the diagnosis and management of cancer difficult. In fact, some predict that 60% of new breast cancer patients will be 70 years old by 2035.8
Our study population responded to a classic hormonal risk factors such as precocious puberty (48.08%) before the age of 15 and late menopause (35%). Among the non-hormonal and genetic risk factors (age and race), some studies also show an influence of socio-economic status on the incidence and prognosis of breast cancer. Indeed, the low level of education, low fixed income and rural residence which are constitutive factors of the socio-economic status in our context would justify this influence. Our study population was not outdone with an average age of 72. 77% out of school, 65% living in rural areas and 87% without fixed income. Thus, this population excludes itself from systematic screening or is excluded by the healthcare systems or the providers, due to the lack of information and awareness on breast cancer screening. Even when they have signs, few women go for a consultation and some do not at all, as it is shown by the consultation time which exceeds a year for more than 60% of the patients. Also, the lack of a routine mammography screening program for women over 65 years of age should be noted, whereas mammography is the first-line examination for screening, especially for this category of people.13
Regarding the symptomatology of breast cancer, it is variable and likely to occur at advanced stages in older women; This is due to the lack of screening (40%), the long consultation time (44%) and the co-morbidity (17%). This is the case in our study knowing that 86.5% had a tumor larger than 5cm (T3) and 20% with metastases at the time of diagnosis. Other authors have also found comparable figures with almost 50% of elderly patients with breast cancer seen at stage T4 and 10% at a metastatic stage.14,15 This is explained by the fact that it is the same African population.
Histological and immunohistochemical dataSome studies show that older people have a characteristic malignant tumor that is more favorable than their younger counterparts. Invasive nonspecific ductal or infiltrating cancer (76%) constitutes the majority of breast cancers in the elderly. Lobular carcinoma represents 5.6% and ductal carcinoma in situ alone 10.0%.16 The most frequently encountered histological type in Ivorian women over 65 years of age was the invasive non-specific carcinoma (94%) and sometimes lobular carcinoma (3.85%). Other studies showed that the cancer in patients diagnosed early was poorly differentiated with a high grade and Ki67 proliferation similar to their younger counterparts.17 We made the same observation with our patients, 75% were of high grade (2 and 3). Also, recent studies have also shown an increase in the presence of estrogen receptors with age, while the human epidermal growth factor2 (Her2) receptor decreases with age.18,19 Overall, the most common presentation in elderly patients is the invasive ductal cancer of higher grade with positive hormonal receptor.
These results are similar to ours. In fact, 21 out of 52 women were able to perform immunohistochemistry allowing the molecular profiling of Ivorian women over 65 years old. Our study found that the most frequently encountered type is luminal A (43%) and few tumors expressed the HER2 oncogene (28%). However, triple negative breast cancer accounted for 28% of cases. This high prevalence of basal like carcinoma can be justified by the racial character with a higher incidence in black women as demonstrated by the work of Kurian20 and Parise.21
Breast cancer managementThe management of breast cancer in the elderly is complex because it has to take into account several elements such as co-morbidity and psychology. Age-related health risks and socio-cultural factors, especially in our African countries, contribute to the factors limiting adherence to the therapeutic standard.22 In some cases, they did not receive treatment as recommended.23,24 Thus, in our study only 19% of women underwent surgery also related to the advanced stage of the disease at the time of diagnosis which required neoadjuvant therapy. In fact, 75% of them received chemotherapy (56% neoadjuvant vs 13% adjuvant). This population (19%) corresponded to 10 out of 22 women with an indication for surgery after neoadjuvant chemotherapy. They have withdrawn either for a lack of finances or a categorical refusal or because they were inoperable due to their general condition. Thus, elderly patients with breast cancer are less likely to obtain chemotherapy compared to younger patients, for reasons including comorbidities, life expectancy and chemo toxicity. The high costs of chemotherapy and the lack of health coverage in our countries are all factors limiting this therapeutic method. Also, women themselves may refuse treatment knowing that there are serious and unwanted toxicities with deleterious effects on the quality of life,25 and it might also be an infringement due to the idea that those women at the end of their lives, are getting chemotherapies for socio-cultural reasons.26
On the other hand, the knowledge of the hormone receptor status may influence the management in favor of endocrine treatment. Endocrine therapy was the most administered non-surgical treatment elsewhere. Generally, a high proportion of elderly women receive endocrine therapy,27,28 which reflects a higher cancer's rate with ER and PR positives receptors, in elderly population. This therapy is also a less toxic treatment than chemotherapy, and is therefore a good option for patients with co-morbidities or the very old patients which are not eligible for surgery. This is why 6 out of 6 (100%) and 6 out of 21 patients with HER2 status, all benefited from this targeted therapy. However, the hormonal therapy was only performed in 2 patients. The practice of radiotherapy decreased with age associated with co-morbidity. In addition, radiotherapy is an adjuvant therapy after surgery, while the indications for surgery are reducing as previously described.1
Overall survivalWhile the incidence of breast cancer increases with age, the relationship between survival and age has not been clearly established in patients over 65 years of age. Previous studies have shown that the advanced age is associated with a statistically significant increase in mortality.29,30 Our work showed that the 5-years overall survival rate was 9.62% for all stages and no matter the molecular profile. This low rate encountered is linked in part to life expectancy and the low level of the human development index in our country.
LimitsThe present study shows some limitations linked to its retrospective character with its corollary of bias. Moreover, the nature of the questionnaire (direct non-anonymous questioning, relating to past information) submitted to the women or to the parents of the patients could have been the source of memorization bias and suggestiveness. Despite these constraints, it is one of the rare studies in Ivory Coast among women over 65 years of age with a small but representative sample, because the sampling base is made out of the cancer registry of Ivory Coast. It has the advantage of guiding future studies concerning this age group.
ConclusionThe present study showed a prevalence of 9.53% of women over the age of 65 with breast cancer. Regarding management, it was essentially non-surgical with a poor survival.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerationsThe informed consent form was obtained from all the participants in this study, and the data confidentiality where also preserved.
Conflict of interestThe authors declare that they have no conflict of interest.
Ivoiry Registry Cancer (ICR).
Society of Gynecologist and Obstetricians of Ivoiry Coast (SOGOCI).