Paget's disease (PD) of the male breast represents less than 2% of male breast cancer. The diagnosis usually delays about 8 months, until it is decided to biopsy the nipple–areola complex lesion. Immunohistochemical techniques help us to differentiate it from other diseases that affect the nipple–areola complex. Most of the patients present an underlying breast carcinoma, which conditions the prognosis. Mastectomy with sentinel lymph node biopsy is the initial treatment in clinically node-negative patients. Two systematic reviews have collected 57 cases of PD of the breast in men published up to 2016. We report an unusual case of mammary PD in a male patient with cytokeratin 7-negative variant.
La enfermedad de Paget (EP) de la mama supone menos del 2% del cáncer de mama en el varón. El diagnóstico suele demorarse alrededor de 8 meses, hasta que se decide biopsiar la lesión del complejo areola-pezón. Las técnicas inmunohistoquímicas nos ayudan a diferenciarla de otras enfermedades que afectan al complejo areola-pezón. La mayoría de los pacientes presentan un carcinoma de mama asociado, que condiciona el pronóstico. El tratamiento inicial en pacientes sin sospecha de enfermedad ganglionar axilar es la mastectomía con biopsia de ganglio centinela. Dos revisiones sistemáticas han recogido 57 casos de EP de la mama en el varón publicados hasta el año 2016. Presentamos un caso inusual de EP de la mama en un varón, con la variante citoqueratina 7 negativa.
Sir James Paget described Paget's disease (PD) in 1874, presenting a series of 15 cases in women.1 PD of the male breast is a rare entity that accounts for less than 2% of male breast cancer.2
Skin biopsy is essential to confirm the diagnosis. Surgery is usually the first treatment, both in women and men. Most patients had associated an underlying breast carcinoma.3
Fifty-seven cases of PD of the male breast have been reported in 2 systematic reviews up to 2016.2,4 During the 20th century, radical mastectomy or modified radical mastectomy were the predominant surgical procedures. In this article we describe an unusual variant of PD in a male patient and discuss relevant aspects in diagnostic and therapeutic management.
Clinical caseWe report the case of a 70-year-old male with history of prostate cancer, referred to our Breast Unit with an erosive lesion in left nipple–areola complex (NAC) of 8 months of evolution, whose biopsy revealed PD (Fig. 1). The patient had been previously treated with topical corticosteroid by dermatologist. From the family history highlighted: 2 brothers with prostate cancer, one brother and one sister with pancreatic cancer, and 2 nieces with breast cancer. The study was completed with a mammography and ultrasound, without other alterations in breast or axilla.
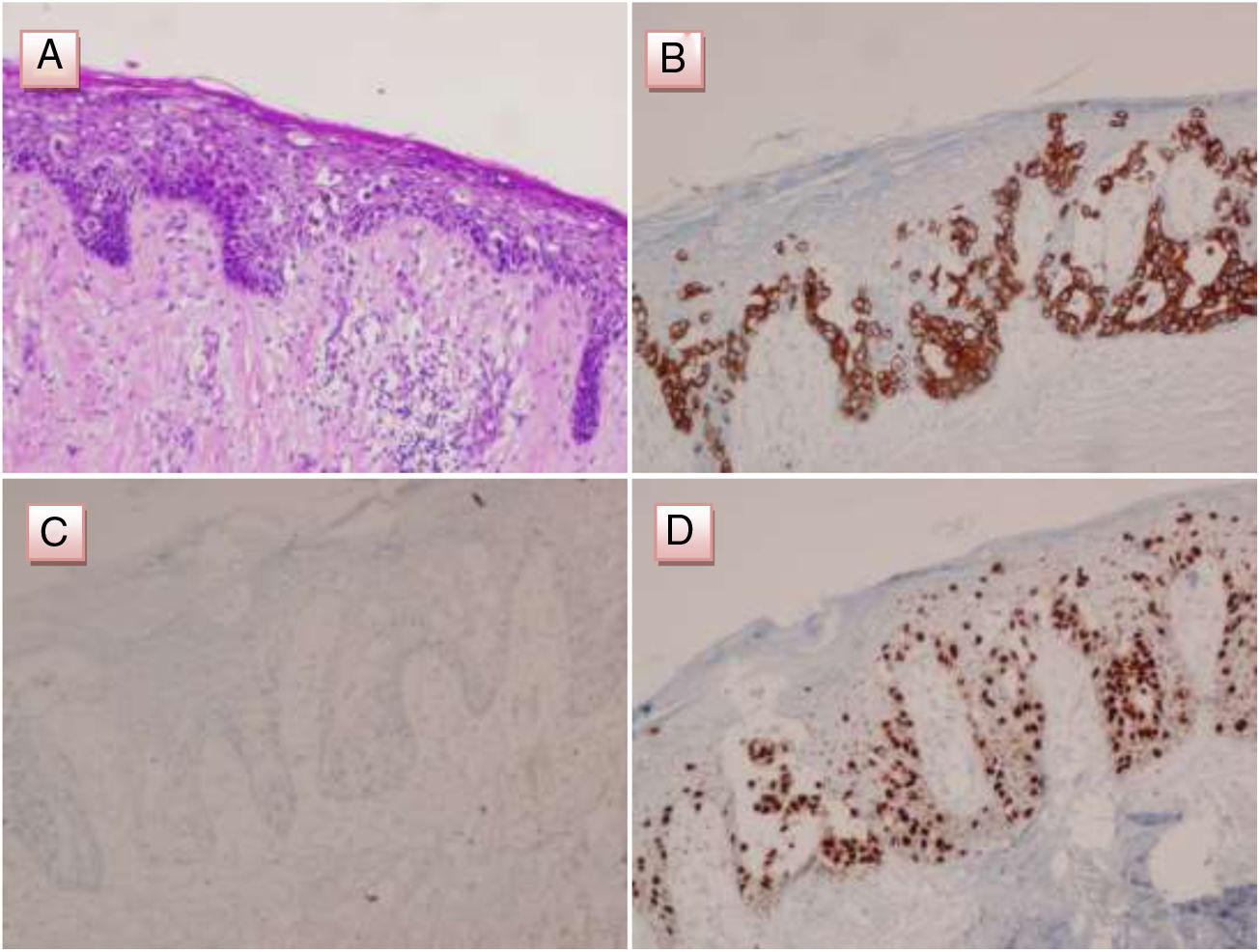
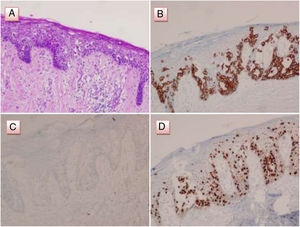
A left mastectomy, including NAC, with sentinel lymph node biopsy (SLNB) was performed. Pathologic examination showed PD of the nipple and the presence of a small focus of ductal carcinoma in situ (DCIS), while immunohistochemical staining of Paget's cells was positive for estrogen receptors (ER), androgen receptors and CAM5.2, and negative for cytokeratin 7 (CK7) and HER2 (Fig. 2). Staining for GATA3 was performed later, being positive. Negativity of SOX10, S100 and HMB-45 helped rule out the possibility of melanoma. In addition, cells of the DCIS were positive for ER. SLNB was negative. The patient did not received other treatments and remains free of disease after 30 months of follow-up.
Pathological and immunohistochemical analysis of the PD of the male breast. (A) Infiltration of the epidermis of the nipple by Paget's cells, characterized by hyperchromatic nuclei with prominent nucleoli and clear cytoplasm (H&E). (B) Immunostain for CAM5.2 in Paget cells was positive. (C) Immunostain for cytokeratin-7 in Paget cells was negaive. (D) Immunostain for GATA3 in Paget cells was positive.
The patient was referred for genetic counseling. Germline mutation testing for BRCA 1/2, ATM, CDH1, CHEK2, MEN1, MLH1, MSH2, MSH6, PALB2, PTEN, RAD50, STK11 genes were negative.
Informed consent was obtained from the patient for the publication of the data and images of the case.
DiscussionPD of the breast is more frequent in women than in men. Approximately 2% of all patients with PD are men.5 PD usually appears after the sixth decade of life in male patients, and presents as an unilateral eczematous or erosive lesion involving de NAC.
Diagnosis tends to be delayed due to its confusion with benign entities of the NAC, with an average diagnostic delay of around 8 months.4 In case of clinical suspicion, it is essential to perform a biopsy of the NAC lesion. PD of the nipple is characterized by epidermal invasion by Paget's cells. Immunohistochemical techniques help us to differentiate the PD from other diseases affecting the NAC, like eczema, Bowen's disease, Toker cell hyperplasia, squamous cell carcinoma or melanoma. Paget's cells of the breast usually express a positive staining for HER2 (80–100%), androgen receptor (71–88%), MUC1 (≈100%), CAM5.2 (70–100%), CK8/18 (98%) and CK7 (98–100%), being the staining of the latter marker the most useful to differentiate the disease.6 CK7-negative variant of PD of the breast is extremely rare, representing a diagnostic challenge of great magnitude. In these cases, positivity of GATA3 help to confirm diagnosis of PD, especially when staining for HER2 is negative.7 To our knowledge, this is the first report of PD of the male breast with CK7-negative variant. Only 2 cases of PD of the breast with CK7-negative and HER2-negative variant have been reported, such as the one we have presented, both in women.8,9
The underlying breast carcinoma conditions the prognosis. The presence of a palpable lesion increases the probability of presenting an associated invasive carcinoma, while its ausence is more frequently associated with the presence of an underlying DCIS.
Breast size in men use to be small and the underlying carcinoma use to be located in the central region of the breast, so mastectomy is considered the standard surgical procedure. Most patients have an underlying carcinoma, which requires an axillary staging. SLNB is the technique of choice if there is no suspicion of axillary lymph node involvement, as reflected in recently published cases.10–14 The first reported case of PD of the male breast treated with SLNB dates from 2003.15
Adjuvant treatment and prognosis, that is usually worse in men tan in women, depends on characteristics of the underlying carcinoma and status of axillary lymph nodes.
It is more common to find a positive family history of breast cancer in male patients that in female patients. It has recently been suggested that PD of the breast and the underlying breast carcinoma are distinct molecular entities.16
In conclusion, an early diagnosis of PD of the male breast influences treatments and prognosis. The treatment of choice in clinically node-negative PD of the male breast is mastectomy with SLNB. Negativity of CK7 in PD of the breast may lead to a diagnostic error and, therefore, the pathologist must recognize this variant and know other markers that can help to confirm the diagnosis.
FundingThe present research has not received specific aid from agencies of the public sector, commercial sector or nonprofit entities.
Confidentiality of dataAuthors declare that standard protocols on the publication of patient data and images have been followed, and the corresponding informed consent has been obtained from the patient.
Conflict of interestThere are no conflicts of interest by any of the authors.
The authors gratefully acknowledge Dr. Begoña Graña (Department of Oncology), member of the Breast Unit of Complejo Hospitalario A Coruña, for their contribution.