Female transgender (male to female) is an individual assigned male sex at birth born but who identifies itself and desires to live as female. To achieve and maintain these characteristics, sometimes, it is necessary to undergo hormone therapy and/or surgical treatment.
Benign lesions have been described including: fibroadenoma, lobular hyperplasia, pseudoangiomatous stromal hyperplasia, myofibroblastoma, angiolipoma and benign prosthesic reactions. And malignant pathology such as: ductal carcinoma in situ, Paget's disease, infiltrating carcinoma of non-special type (ductal, NOS), secretory adenocarcinoma, malignant phyllodes tumor and breast implant associated anaplastic large cell lymphoma.
The described cases of each of these entities are reviewed.
In conclusion, hormonal action or prosthesis implantation in female transgender can lead to associated pathologies in the mammary gland that follow a similar pattern to that found in the male breast. Although breast cancer is less frequent than in cisgender women, gynecological control or screening is recommended by some associations.
La mujer transgénero (hombre a mujer) es aquella persona nacida varón pero que se identifica y desea vivir como una mujer. Para lograr este objetivo muchas veces precisa de tratamiento hormonal o quirúrgico para alcanzar los atributos sexuales de una mujer.
La patología mamaria que estos pacientes pueden presentar es superponible a la patología de la mama masculina, a la patología derivada del tratamiento hormonal y a la relacionada con los implantes mamarios sintéticos.
Se han descrito lesiones benignas que incluyen: fibroadenoma, hiperplasia lobulillar, hiperplasia estromal seudoangiomatosa, miofibroblastoma, angiolipoma y reacciones benignas a la prótesis. Y patología maligna como: carcinoma ductal in situ, enfermedad de Paget, carcinoma infiltrante de tipo no especial (ductal, NOS), adenocarcinoma secretor, tumor filoides maligno y linfoma anaplásico de célula grande asociado a prótesis.
Se revisan los casos descritos de cada una de estas entidades.
En conclusión, la acción hormonal o la implantación de prótesis en las mujeres transgénero pueden llevar asociadas patologías en la glándula mamaria que siguen un patrón similar al de la patología encontrada en la mama del varón. Aunque el cáncer de mama es menos frecuente que en las mujeres cisgénicas, se recomienda un control ginecológico o mediante cribado igual al de estas.
Transgender is an adjective used to describe an individual whose gender identity or expression does not correspond to the one assigned at birth. It is independent of genotype, physical appearance, sexual orientation and behavior. A Female transgender (FT) (male to female) is an individual assigned male sex at birth born but who identifies itself and desire to live as female. To achieve and maintain these characteristics, sometimes, it is necessary to undergo hormone therapy and/or surgical treatment.1,2
Hormonal effectsThe purpose of hormone treatment is to induce female changes and suppress secondary male changes.3 However, this treatment can induce disorders such as: venous thromboembolic disease, hypertriglyceridemia, cholelithiasis, coronary artery disease, cerebrovascular disease, macroprolactinoma, breast and prostate cancer among others might be side effects of such treatment.3,4
The effect of estrogenic treatment on FT is the induction of breast development, redistribution of body fat and reduction of muscular mass. The male breast has only mammary ducts and under normal conditions lacks lobular units. Lobular development has been observed in situations of hyperestrogenism and Klinefelter's syndrome5 and occurs in approximately 1% of cases.6 Continuous and permanent exposure to estrogens stimulates the estrogen receptors located in the rudimentary ducts of the areola-nipple complex, elongating and branching them. These ducts will be organized into lobes and lobules, with small terminal buds appearing. This growth is accompanied by an increase in stroma and adipose tissue that will give volume to the breast (Figs. 1–3). The evolution of this process depends on type, duration and dose of treatment. Changes usually appear rapidly in 6–12 months and then stabilize and in general after 2 years there are no further changes.2,3,6–8 Studies that compare the histology of the mammary gland in FT with those found in men chemically castrated for prostate cancer describe the development of acinar and lobular units in FT treated with estrogen and progesterone. Elevated plasma levels of estrogen/androgen ratio and orchiectomy alone do not contribute significantly to acinar and lobe formation.1,5 In hormonally treated FT with estrogens and progestogens, the presence of intralobular milky secretion material and pseudolactational changes in the cells surrounding the lobule, apocrine metaplasia and certain degrees of hyperplasia in the ductal lining epithelium have been described5 (Fig. 4). The findings of FT breast tissue are in contrast to gynecomastia seen in male breast, which involves only ductal and stromal hyperplasia secondary to a mildly increased plasma estrogen-to-androgen ratio, which commonly manifests as nodular subareolar density. For this reason, the term gynecomastia should not be used when reporting on breast tissue in transgender individuals.2
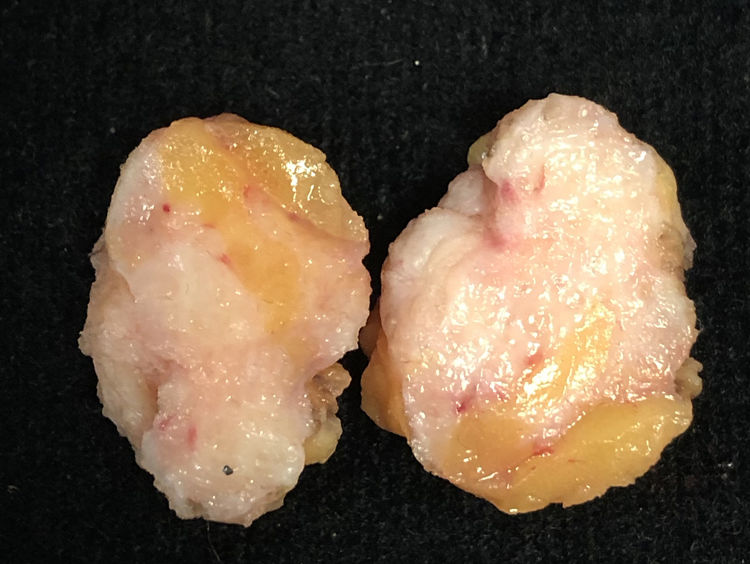
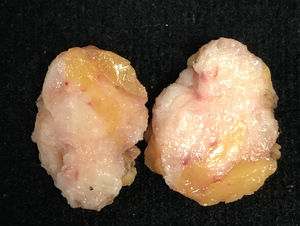
Macroscopic appearance of a surgical specimen removed due to a suspicious image on mammography. The patient was a 61-year-old FT with breast implants and under hormonal treatment. She was surgically treated for having a palpable and spiculated image at mammography which proved to be a benign lesion with stromal fibrosis.
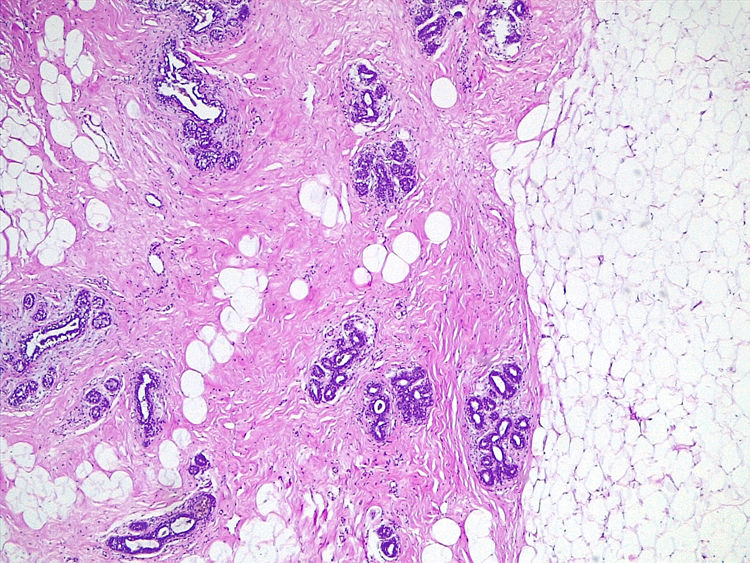
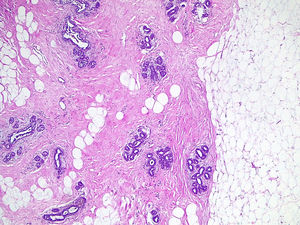
Histological image of the resection specimen with adipose tissue, connective tissue and duct-lobular units. This histological structure is the same that the one seen in the female breast (Same patient as Fig. 1) (H&E ×40).
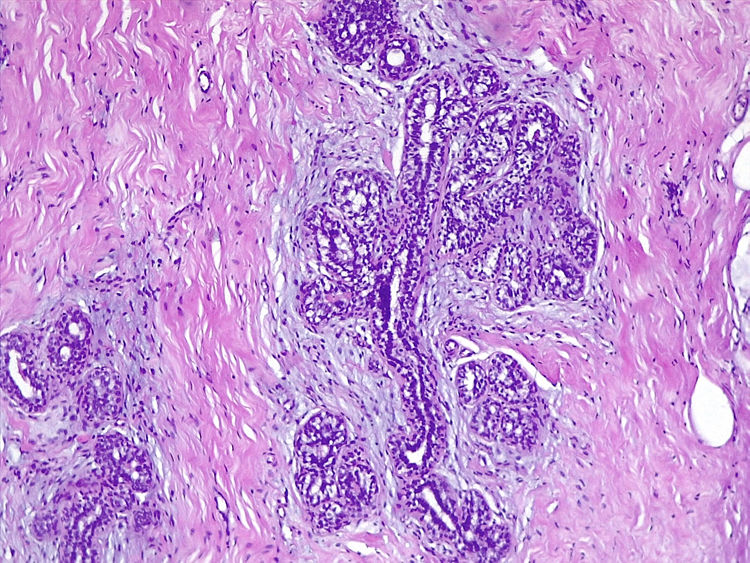
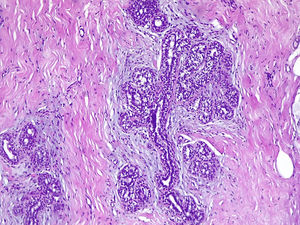
Detail of a ductal unit surrounded by alveolar sacs (Same patient as Fig. 1) (H&E ×100).
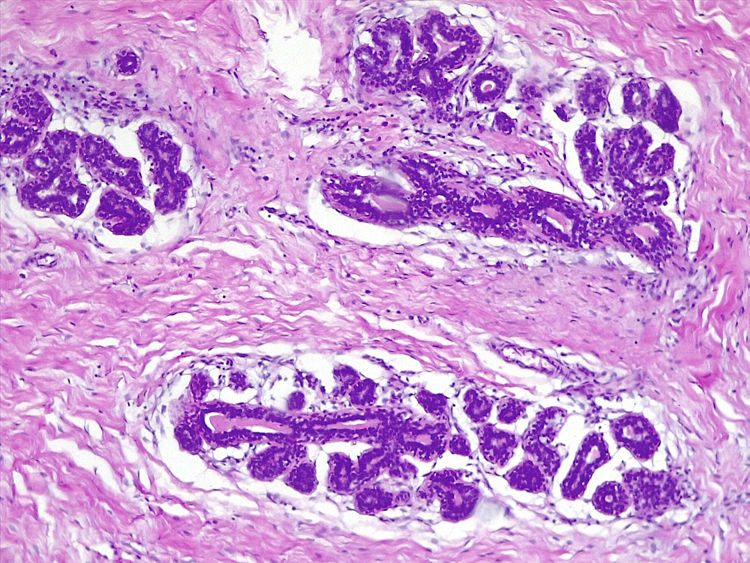
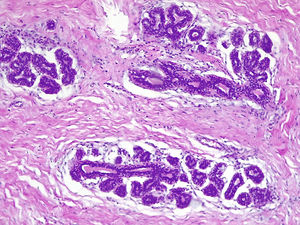
Presence of intraluminal secretion in the alveolar sacs (Same patient as Fig. 1) (H&E ×400).
The time from the beginning of the hormonal treatment and the appearance of esthetically satisfactory breasts is an inconvenience that makes it necessary to recur to breast augmentation through surgery by means of prosthesis implantation.7 It is estimated that between 60–70% of FT might require the implantation of breast prostheses to this end.1,10
The effect of hormonal treatment on the risk of breast cancer is well known, although this effect on the male breast is not well stablished.2,10 In addition to hormonal treatment, the risk of cancer in the male breast is also increased by obesity, chronic liver disease, hyperlipidemia and genetic predisposition, especially a defective BRCA 2.11–13 The risk of cancer in FT has to be considered in the context of the native sex, contrary to male transgender in whom it has to be considered in the context of the new sex.11 The epidemiology of cancer in FT follows a similar or slightly higher pattern than that of male breast cancer rather than a female pattern,9,14,15 although there are studies in which the incidence of standardized breast cancer for FT is 0.7 (95% CI 0.03–5.57) compared to cisgender women, but 33.3 (95% CI 21.89–45.17) compared to cisgender men.16 A slight increase in risk has also been seen if there is a direct family history.17 Although there is no evidence to carry out a specific screening program for these patients, although it is recommended by most authors and scientific societies.1,15,18,19 Current screening recommendations in the transgender female population vary according o the age of the individual and other risk factors including the duration of hormone therapy. Generally, advocates recommend annual or biennial screening starting at age 50 years.2 However, none of the diagnosed cancer cases in FT have been detected through screening programs.18
PathologyThere are about 40 cases of cancer in FT described in the literature and most of them correspond to isolated cases.9,12,13,20 The incidence of breast cancer is 4.1 per 100,000 person-year. It has been calculated that this incidence does not differ significantly from that adjusted for the expected age in men.12 In a study of 5135 transgender people from the US Veterans Affairs, 10 cases of breast cancer were detected, three of them in FT. In another series of 2307 FT only one breast cancer was detected.11 The average age at diagnosis is 51.5 (27–69) years. Finally, in a nationwide study in the Netherlands, out of a population of 4432 FT, 18 cases of breast cancer were identified in 17 women (one with two tumors), diagnosed after an average of 18 months (87–37 months) of hormonal treatment.
Breast cancer in FT, which is diagnosed in advanced stages,11,12 is usually hormone receptor positive,11,12 although there is a described case of triple negative.21 HER2 overexpression in breast cancer, which is estimated at 4% of FT,12 has been found to be higher than that observed in men (1.7%), but lower than that observed in women (6–12%).9,12
Despite the fact that the pathology that may appear in the breast of FT shows similar morphological characteristics to those of the male breast, benign and malignant entities, that have been described in the literature will be reviewed below.
Benign pathology- -
Fibroadenoma: There are two cases reported in the literature of fibroadenoma in FT. The ages at presentation were 35 and 41 years, both receiving hormonal treatment from 13 and 19 years respectively.20 The fibroadenoma shows a histological image characterized by a biphasic proliferation with an epithelial component forming glands and clefts with a double cell lining, and a mesenchymal component of variable density that can sometimes show myxoid changes. Atypia is not seen in neither component. Most of the fibroadenomas described in the male breast are part of the context of a gynecomastia.5,22
- -
Lobular hyperplasia: A case of lobular hyperplasia has been described in the right breast of a 38-year-old FT who has been under hormone treatment for one year.23 The lesion is similar to conventional lobular carcinoma in situ although some diagnostic criteria are lacking. There is a distension of the lobule due to a monomorphic cellular proliferation but without the attachment of some lobular units to others.22 This is the only lesion involving lobular structures found in the literature in FT.
- -
Pseudoangiomatous stromal hyperplasia (PASH): There are two cases of PASH in FT reported in the literature. One is the same patient cited previously with lobular hyperplasia in which both lesions coexisted.23 Another case corresponds to a patient with a family history of cancer. The lesion was in the periareolar region of the left breast and the age is not specified.24
- -
PASH, which on many occasions is a casual finding in the context of gynecomastia, is characterized by the presence of a complex network of interanastomosing spaces in a densely collagenous, keloid-like stroma. Some spaces are lined by flattened myofibroblasts that simulate endothelial cells. They do not show atypia.6
- -
Myofibroblastoma: A case of myofibroblastoma has been described in a 76-year-old FT after 13 months of hormone treatment. The lesion was discovered in the right breast in a mammographic study.20 Histologically the lesion shows characteristics similar to soft tissue myofibroblastoma. It is a spindle cell proliferation of the mammary stroma composed of myofibroblasts. These fusiform cells are arranged in bands separated by bundles of collagen and adipocytes. Depending on the cellular characteristics there are the following variants: collagenized, cellular, epithelioid, myxoid, fibrous, lipomatous, deciduoid, atypical and infiltrating.
- -
Cytological atypia is minimal. Immunohistochemically, cells express CD34, desmin, vimentin, calponin and smooth muscle actin. The expression of estrogen and progesterone receptors is also frequent. Cytokeratins are negative.
- -
Angiolipoma: The only case of angiolipoma described in a FT was 61-year-old who had received hormonal treatment for 18 months.20 Angiolipoma shows a proliferation of mature adipocytes containing numerous small-size vessels, some with small intraluminal thrombi.4
- -
Pathology associated with prosthesis or filling elements: In search of a rapid increase in breast volume and with the desired esthetic characteristics, breast implants are used frequently.2,13,25 Due to problems of access to the health system or socioeconomic reasons, other unorthodox and/or illegal practices of substance injection are used to achieve a breast volume increase. These include food- or industrial-grade silicone, liquid paraffin, petroleum jelly, lanolin, beeswax, flax oil, linseed oil, olive oil, tire sealant, cement glue, automobile transmission fluid, among others.25 Aside from the toxic and allergenic reactions that these substances can cause, the pathologies that can arise are5,13,22:
- •
Inflammation: chronic and acute inflammatory infiltration around the foreign body or the mammary ducts and lobules.
- •
Granulomas: Proliferation of histiocyte cells with a foreign-body type giant cell reaction. Necrosis may occur.
- •
Siliconoma: Consists of a non-specific foreign body type granulomatous reaction, identifying multinucleated giant cells that contain microvacuoles or asteroid bodies, with fibrosis and inflammatory changes. Sometimes metaplasia can be identified in the capsule of the prosthesis that simulates the synovial lining.
- •
Necrosis: fat necrosis is a disruption of adipocytes accompanied by bleeding and histiocyte deposits. Sometimes there is calcification, multinucleated giant cells and inflammatory changes.
Thirty-one adenocarcinomas (18 ductal, 13 unclassified),4 ductal carcinomas in situ, one secretory carcinoma, one malignant phyllodes tumor, one Paget's disease associated with infiltrating carcinoma, two unclassified malignant lesions and 4 lymphomas associated with breast prosthesis have been described.9,12,20,26
- -
Ductal carcinoma in situ: It is malignant epithelial proliferation confined to the mammary duct, limited by the basal membrane, without invasion of the adjacent stroma.22,27 Four cases of ductal carcinoma in situ in FT are found in the literature.9,18 No lobular carcinomas in situ have been described in the breast of transgender women.
- -
Paget's disease: Characterized by the presence of large cells with abundant clear cytoplasm and nucleus with prominent nucleolus that are located as a single cell, in small nests or glands in the epidermis of the nipple, areola or both. It can be clinically confused with eczema or erosions of the nipple-areola complex. It is usually associated with an underlying, infiltrating or in situ carcinoma5,22 especially in male patients.28 One case of Paget's disease associated to invasive ductal carcinoma has been reported in a 55-year-old FT wits breast silicone injection.18
- -
Infiltrating adenocarcinoma of non-special type: As in the female breast, infiltrating carcinoma of non-special type (Ductal, NOS) is constituted by a proliferation of cells that group in nests, trabeculae or tubules, or sometimes in a solid pattern. The cases reported in FT are usually hormone receptors positive. HER2 is positive in 8% of cases.9,12 Although the breast of FT may have lobules,5 no lobular carcinoma has been described in this population.10,20,21
- -
Secretory adenocarcinoma: This term classifies those tumors in which cells produce secretion, similar to lactic fluid, intra or extracellular. They can be arranged in a microcystic, solid or tubular pattern.5 A case of secretory adenocarcinoma in a 46-year-old FT with silicone breast implants and more than 20 year of hormone treatment is recorded in the literature.29
- -
Malignant phyllodes tumor: It is a biphasic lesion of the breast constituted by a benign epithelial component that forms clefts of foliaceous morphology, sometimes with cystic dilation, and a hypercellular stromal component. According to the characteristics of the mesenchymal component, they are classified as benign, borderline and malignant.5,6,27 Only one case of malignant phyllodes tumor has been described in a 53-year-old FT.12
- -
Anaplastic large cell lymphoma (ALCL) associated with breast implant: Four cases of ALCL associated with breast implant have been described in FT aged 27, 49, 54 and 56 years.10,12,26,30 Three of them in the left breast and one in the right one. The period from the implant of the prosthesis and the appearance of the lesion is 7, 7, 9 and 20 years. The form of presentation was as a diffuse increase in breast volume in two and as a mass of 1.5 and 5cm in the other two cases. Three patients were treated with prosthesis explantation and capsulotomy, adding chemotherapy in two of them, and with mastectomy and radiotherapy in the remaining one. One of the described cases showed the involvement of two sentinel lymph nodes by lymphoma26 and another one showed infiltration beyond the breast into the pectoral muscle.30
It is a T-cell lymphoma that can be diagnosed in the periprosthetic fluid by the presence of large and dispersed pleomorphic blasts. The neoplastic cells are usually found in the capsule that surrounds the prosthesis. Extension to the adjacent breast parenchyma is rare. They are large non-cohesive and pleomorphic cells. The cells express CD30 and are negative for CD20 and CD15. Most are ALK negative.27
In conclusion, hormonal action or prosthesis implantation in FT can lead to associated pathologies in the mammary gland that follow a similar pattern to that found in the male breast. Although breast cancer is less frequent than in cisgender women, gynecological control or screening is recommended by some associations.
Conflict of interestsF. Tresserra is Co-Managing Editor of “Revista de Senologia y Patologia Mamaria”.
This article has been done Under the auspices of the “Càtedra d’ Investigació en Obstetrícia i Ginecologia de la Universitat Autònoma de Barcelona”.