We present a case of a 66-year-old female with a history of traumatic breast injury treated with mastectomy and subsequent bilateral breast prosthesis surgery and presenting with a suspected right breast nodule with histological confirmation of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Subsequently, she underwent a 18F-FDG PET/CT scan that demonstrated increased focal uptakes along the perimeter of the right breast implant corresponding to several nodules. She underwent a right mastectomy with prosthesis removal. With this report, we underline the potential usefulness of 18F-FDG PET/CT in detecting BIA-ALCL.
Presentamos el caso de una mujer de 66 años con antecedente de lesión mamaria traumática tratada con mastectomía y cirugía de prótesis mamaria bilateral y que presenta sospecha de nódulo mamario derecho con confirmación histológica de linfoma anaplásico de células grandes asociado a implante mamario (BIA-ALCL). Posteriormente, se le realizó una PET / TC con 18F-FDG que demostró captaciones focales aumentadas a lo largo del perímetro del implante mamario derecho correspondiente a varios nódulos. Se sometió a una mastectomía derecha con extracción de prótesis. Con este articulo, subrayamos la posible utilidad de la PET / TC con 18F-FDG en la detección de BIA-ALCL.
BIA-ALCL is a rare form of non-Hodgkin lymphoma thought to be arising from a chronic T cell proliferation in periprosthetic tissues.1–4 ALCL represents approximately 2–3% of all non-Hodgkin's lymphomas.5 Subtypes of ALCL can be grouped by the presence or absence of anaplastic lymphoma kinase (ALK) surface receptor and also by primary site of involvement, that is, primary cutaneous ALCL and breast implant-associated (BIA)-ALCL.6 BIA-ALCL is ALK negative. The estimated incidence of BIA-ALCL is 2.03 per 1 million person years with an estimated prevalence of 1 per 30,000 women with breast implants.7 The first case report of BIA-ALCL was published in 1997 by Keech and Creech,8 but only in 2016, almost two decades later, the World Health Organization recognized BIA-ALCL as a distinct entity.9 Given the widespread use of breast implants, there is an increased awareness of the risk for developing BIA-ALCL. The role of 18F-FDG PET/CT in BIA-ALCL hasn't been completely defined yet, with only several exceptional cases reported in literature.2 With this report, we underline the potential usefulness of 18F-FDG PET/CT in detecting BIA-ALCL.
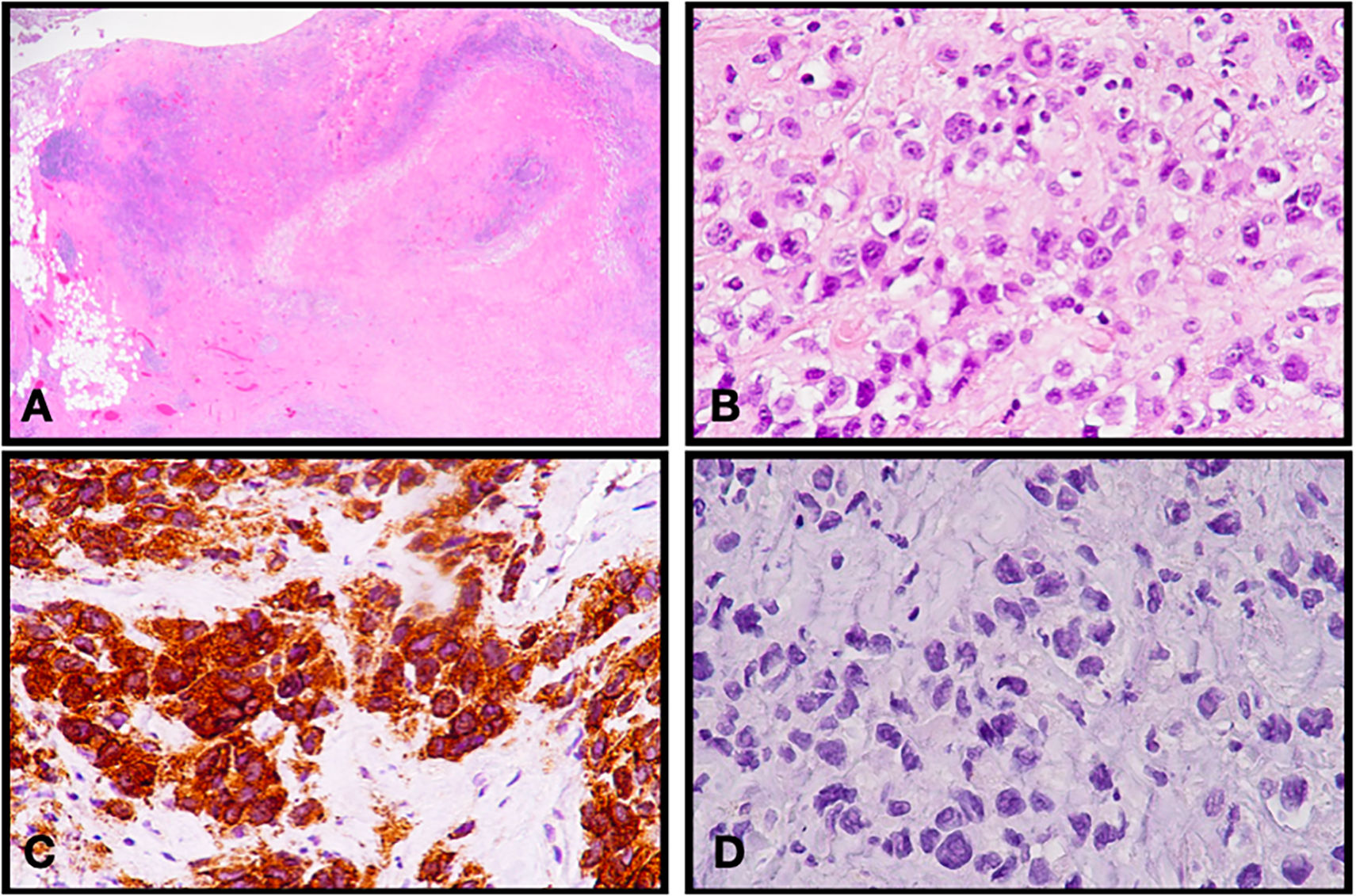
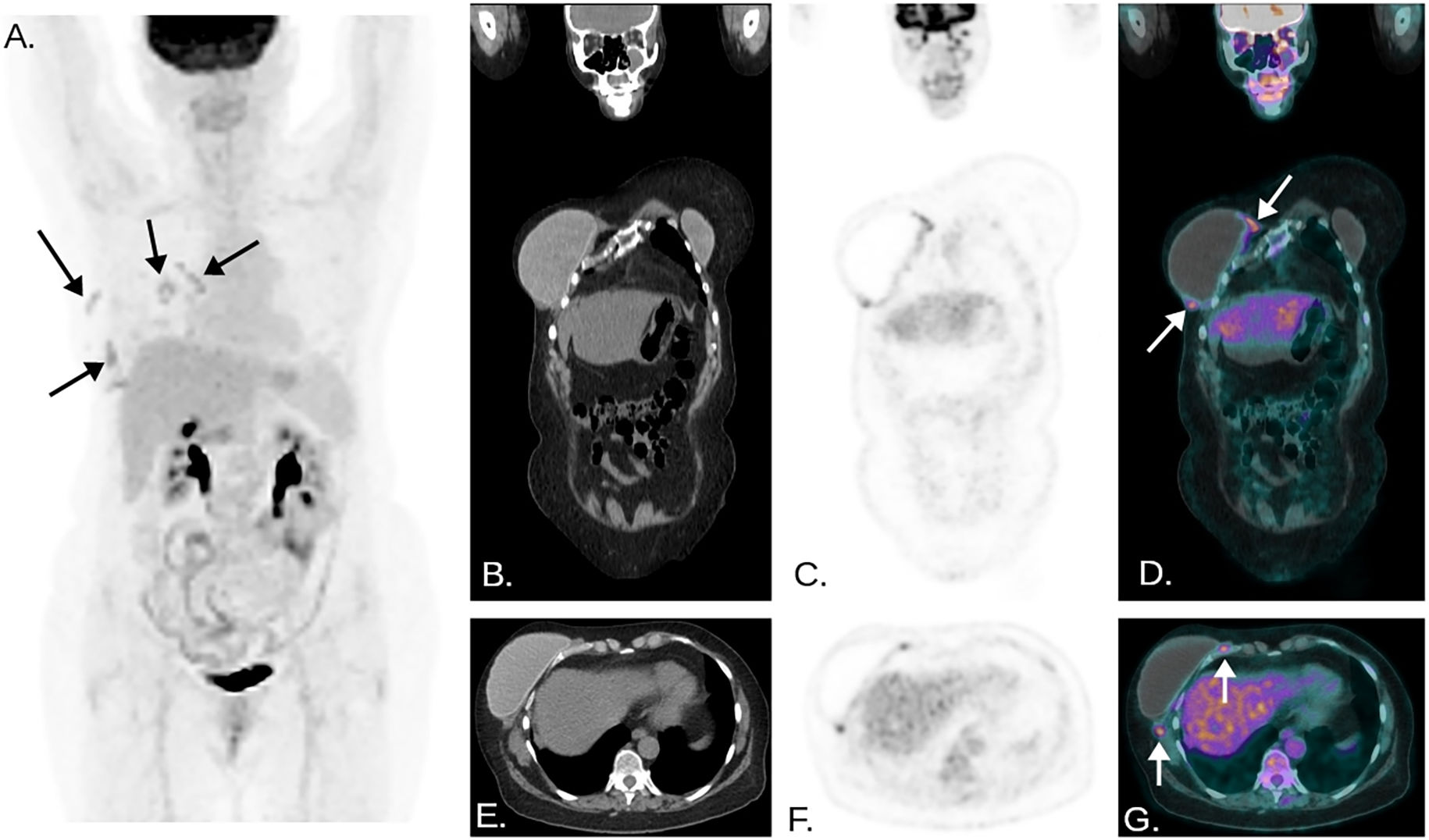
Clinical caseA 66-year-old female was treated with right mastectomy in 1985 after a traumatic breast injury and subsequently underwent three bilateral breast augmentation mastoplasty procedures, the last one being performed in 2009. In 2020 she presented with mastodinia and a suspicious 15 mm right breast nodule, adherent to the periprosthetic capsule. The patient underwent a core biopsy of the breast nodule showing breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) (Fig. 1). A subsequent 18-Fluorine-fluorodeoxyglucose positron emission tomography/computer tomography (18F-FDG PET/CT) was performed to stage the patient. PET-CT images were acquired about 60 min after an intravenous injection of 3.5 MBq/Kg of radiotracer on a Discovery 690 tomograph (GE; Milwaukee, WI; 64-slice CT, 100 mA, 120 kV, 2.5 min/bed; 256x256 matrix, 60-cm field of view) (Fig. 2). PET/CT images showed increased focal uptake along the perimeter of the right breast implant corresponding to several nodules. A magnetic resonance imaging (MRI) confirmed the presence of several nodules (at least six) around the prosthesis and a chest CT scan also showed the presence of periprosthetic solid tissue. The patients then underwent a right capsulectomy with prosthesis removal together with all nodules surrounding the implant and axillary node sampling, with final diagnosis of BIA-ALCL on the right breast mass and reactive-type lymph node.
Hematoxylin and eosin stained histologic sections (fig. A and B) revealed a diffuse lymphomatous infiltrate of atypical large sized appearing cells, with moderate amounts of pink cytoplasm, pleomorfic vesicle looking nuclei, prominent nucleoli and several mitotic figures. The histological sample also demonstrated BIA-ALCL CD30 positivity (fig. C) and ALK negativity (fig. D) without lymph nodes involvement.1 (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
PET/CT images showed increased focal uptake along the perimeter of the right breast implant corresponding to several nodules, especially on the postero-medial and lateral aspects, as seen in maximal intensity projection (MIP) images (black arrows, image A). Coronal and axial views also clearly show the uptakes previously described (white arrows, image D and G). No other increased FDG uptake was detected.
BIA-ALCL is a rare form of non-Hodgkin lymphoma thought to be arising from a chronic inflammation of the biofilm surrounding implants, leading to malignant transformation of activated T cells in genetically susceptible individuals.1–4 A predominance of cases of breast implant-associated anaplastic large cell lymphoma in patients with a certain type of implants (macrotexturized surface implants vs smooth surface implants) have been shown,1,2 though there is no scientific evidence supporting this correlation yet. It is thought that the higher surface area of textured implants may provide a better platform for bacterial growth.2 Breast implant-associated anaplastic large cell lymphoma presents most commonly approximately 10 years after implantation of textured silicone or saline breast implants.10 This disease may present with breast enlargement, peri-implant effusion and swelling, a palpable breast or axillary mass, lymphadenopathy, breast skin erythema, or pain.2,10,11
Diagnosis is based on ultrasound, to assess the presence and the extent of peri-implant effusion and to evaluate any associated capsule masses or swollen regional lymph nodes,12 and pathology studies such as sampling of peri-implant fluid, biopsy/FNA of peri-implant masses or regional lymph nodes and immunohistochemical staining.10,12,13
MRI is adopted for US equivocal cases.12 Surgical treatment with capsulectomy is the main treatment option, including the removal of all pathological masses around the capsule itself and axillary lymph nodes, if involved. Chemotherapy and Radiotherapy can be helpful in case of inoperable or disseminated disease.1 With the exception of advanced cases, prognosis is good with BIA-ALCL having an indolent course.13,14 The role of 18F-FDG PET/CT in BIA-ALCL hasn't been completely defined yet, with only several exceptional cases reported in literature.10
Whereas US and MRI are the most performing imaging methods for detecting peri-implant collections, with 84% and 82% sensitivity, PET/CT has the highest sensibility (64%) in assessing the solid mass pattern of BIA-ALCL.15 It is the established imaging modality for pre-operative staging of the disease and it may be useful in evaluating the regional extension, axillary nodes and distant metastasis involvement. The recommended routine surveillance regime also suggests performing either a CT or a 18-FDG PET/CT scan for the first year of follow up.14–16 Hybrid PET/MRI is an emerging and promising imaging technique that can provide comprehensive morpho-functional imaging information which improves patients' management in this newly recognized sub-type of lymphoma.12
Ethical considerationsThe protocols of our institution on the publication of patient data have been followed, that privacy has been respected, and we have the consent of the patient for our publication.
FundingNo financial support for the conduct, preparation, writing and submission decision of this work was provided.