The phenomenon of occult breast cancer represents a rare scenario raising crucial questions regarding its clinical presentation, diagnosis, and timely treatment. The therapeutic challenge can become even more difficult in the specific case of triple-negative breast cancer. This article presents the case report of a patient who had a palpable axillary nodule during a routine gynecological exam. A core needle biopsy confirmed that the patient had metastatic ductal carcinoma of mammary origin, which was triple-negative. Despite several diagnostic procedures, there was no evidence of a primary tumor in the breast clinically or in imaging studies. The patient underwent neoadjuvant chemotherapy with satisfying outcomes and later, to radical surgery therapy regardless of the feasibility of receiving a conservative treatment.
El fenómeno del cáncer oculto de mama representa un escenario raro que plantea preguntas cruciales sobre su presentación clínica, diagnóstico y tratamiento oportuno. El desafío terapéutico puede volverse aún más difícil en el caso específico del cáncer de mama triple negativo. Este artículo presenta el caso clínico de una paciente con un nódulo axilar palpable durante un examen ginecológico de rutina. Una biopsia con aguja gruesa confirmó que la paciente tenía un carcinoma ductal metastásico de origen mamario, que era triple negativo. A pesar de varios procedimientos diagnósticos, no hubo evidencias ni clínicas ni en estudio de imágenes de un tumor primario en la mama. La paciente recibió quimioterapia neoadyuvante con resultados satisfactorios y posteriormente, una terapia quirúrgica radical, independientemente de la viabilidad de poder recibir un tratamiento conservador.
Breast cancer, one of the most prevalent and studied malignant neoplasms in oncology, can challenge traditional paradigms of early detection despite significant improvements in diagnosis and therapy.1 One example is the phenomenon of occult breast cancer, a rare scenario raising crucial questions regarding its clinical presentation, diagnosis, and timely treatment.2 In this case report, we present an analysis of a patient facing an unusual diagnosis: occult breast cancer (OBC). This term refers to the absence of a palpable mass or detectable lesion in the breast parenchyma, despite clinical signs or symptoms suggestive of mammary neoplasm, primarily presenting a metastatic axillary lymph node.3
The initial steps in the diagnostic process for OBC involve clinical and radiological examinations. Nevertheless, the comprehension of diagnostic and therapeutic strategies for occult breast cancer remains indeterminate. It is advisable to regularly conduct breast magnetic resonance imaging (MRI) for individuals with diagnostic presumptions of OBC, since it can detect the primary tumor in most of these cases, although confirming lesions through histological examination is crucial because of the reduced specificity of this procedure.4 The specific biologic subtype of breast cancer, present in this patient (triple-negative), exhibits a poor responsiveness to both endocrine therapy and molecular-targeted treatments. As a result, chemotherapy stands out as the primary systemic treatment choice.5
Traditionally employed for locally advanced breast cancer, neoadjuvant chemotherapy (NAC) works primarily to facilitate surgical downstaging. Moreover, it provides patients with triple-negative breast cancer (TNBC) the chance to enhance survival, even in cases of early-stage disease.5 Researchers have explored different approaches, comparing extensive procedures like mastectomy and axillary lymph node dissection (ALND) with less invasive options such as breast-conserving radiotherapy. The latter modality seems to exhibit analogous efficacy.3 This case report was prepared following the CARE guidelines.6
Clinical caseA 52-year-old woman with a family history of colon and cervical cancer, after a routine gynecological review at a public general hospital, was referred to a breast surgery consultation due to a palpable nodule in the right axilla, painless, without other signs or symptoms. Physical examination revealed a cluster of nodes in the right axilla, but no tumors were found in the breasts. An ultrasound of the right axilla reports a right axillary lymph nodes conglomerate measuring 10 mm×14 mm in level I. One lymph node with subtle diffuse cortical thickening measuring 3.6 mm×3.3 mm×3.9 mm, and another with loss of its morphology measuring 4.5 mm×4.9 mm. An ultrasound-guided core needle biopsy of a right axillary nodule confirmed the diagnosis of metastatic breast cancer. Lymphoid structures were identified in the sample. The pathological report indicated a ductal carcinoma grade II with a negative immunohistochemistry profile for estrogen and progesterone hormone receptors, as well as HER2-NEU (triple-negative cancer). The KI67 proliferation index was calculated at 25%.
Follow-up breast ultrasound revealed heterogeneous tissue in the right breast without solid nodules. Additionally, mammography showed no pathological findings in bilateral breast tissue. Extension studies, such as chest, abdomen, and pelvic CT scans, ruled out distant metastases. In the absence of a tumor on the imaging studies, a breast MRI with intravenous contrast was ordered, revealing no pathological findings in the breast parenchyma (Fig. 1). According to the 8th edition of the American Joint Committee on Cancer (AJCC) – TNM staging system for breast cancer, due to clinical characteristics, this case is classified as occult breast cancer (cT0), with a cluster of axillary lymphadenopathies (N2), no evidence of distant metastasis (M0), stage III-A.
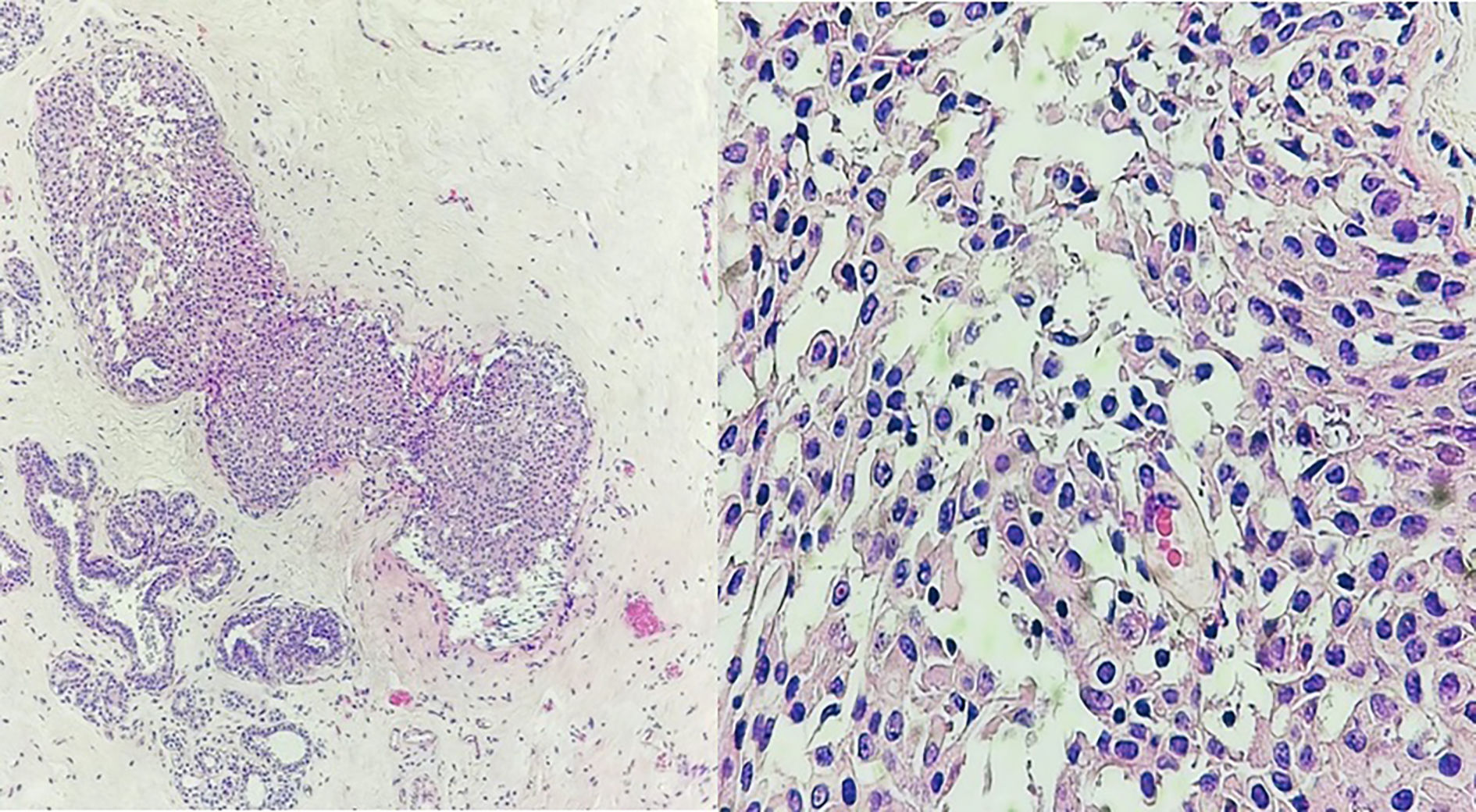
The patient received neoadjuvant systemic chemotherapy—Doxorubicin and Cyclophosphamide every 21 days, followed by 12 weeks of weekly Taxane. After 4 cycles of chemotherapy, fine needle aspiration of a lymph node was performed, revealing negative cytology for malignancy. No decrease in the size of the cluster lymph nodes measures was evidenced in an ultrasound realized once NAC therapy ended. The patient continued the treatment in a specialized private cancer center where surgical therapy was performed. The breast committee discussed the case and recommended a therapeutic approach. Despite being informed about the benefits of conservative breast treatment, the patient chose radical mastectomy with ALND based on her preference. Post-surgery, the pathological report of the right breast specimen revealed a focus of cribriform and solid-type ductal carcinoma in situ with nuclear grade 2, measuring 3 mm in diameter in the surgical bed (Fig. 2). A total of 7 regional lymph nodes adjacent to the axillary extension of the breast corresponding to the palpable cluster in level I were resected, showing no residual neoplasia (0/7), as did the 18 axillary level II lymph nodes (0/18). All these pathological findings indicate a complete pathological response to neoadjuvant chemotherapy.
Ductal carcinoma in situ. (A) Intraductal proliferation of atypical ductal cells. Cohesive in a solid growth pattern, columnar changes in slightly dilated and ecstatic ducts are seen. (B) Close-up at 40× magnification. Uniformly spaced cells with moderate nuclear pleomorphism and occasional prominent nucleoli.
Currently, the patient remains under follow-up. Imaging studies show no signs of lymph node or primary breast tumor recurrence. The final TNM staging system for breast cancer for this is classified as stage III-A (ductal carcinoma in situ <1 cm: T1; a cluster of axillary lymphadenopathies: N2; no evidence of distant metastasis: M0).
DiscussionThe identification of occult breast cancer relies on the existence of an axillary adenopathy without signs of a primary tumor in the breast. Clinical and radiological evaluations are the initial steps in the diagnostic process.4 An axillary adenopathy may suggest the presence of other diseases, such as malignant neoplasms in other organs (e.g., thyroid carcinoma, lymphoma, melanoma, sarcoma, germ cell tumor) or benign processes like local inflammation.7 Biopsy of axillary lymph nodes is essential to confirm the diagnosis and determine the molecular subtype of breast cancer, guiding therapeutic decisions.8 MRI can be used to locate the primary lesion or to rule out breast tumors when other diagnostic methods have failed.4,9 However, exceptional cases like the present one may fail to detect breast parenchymal lesions even with MRI. The treatment of occult breast cancer is still controversial.10
TNBC requires specialized treatment due to its poor prognosis and its insensitivity to systematic therapies such as the endocrine and target ones.5 NAC was chosen as the initial treatment following the National Comprehensive Cancer Network (NCCN) guidelines for triple-negative invasive carcinoma.11 This therapy shows a high rate of nodal-level response. The use of Cyclophosphamide and Taxane for this particular biological subtype of breast cancer reduces the risk of local recurrence and distant metastasis.12 Standard treatment for nodal disease in OBC involves ALND, however, a clinical and radiological axillary response might allow de-escalation of surgery,13,14 by removing the marked metastatic node before chemotherapy and recommending a minimum of 3 sentinel lymph node biopsies to avoid false negatives.15
The “GeparOcto Trial” on NAC response in HER2+ and triple-negative cases reveals the limitations of clinical and imaging assessment for nodal response. 57.1% of patients with suspected persistent clinical axillary involvement post-chemotherapy showed a complete pathological response, clinically unsuspicious lymph nodes (ypN0), without residual metastatic disease in pathology.16 Although all these facts, according to NCCN guidelines, patients with OBC diagnosed by MRI should be treated based on nodal condition: (1) For T0N1M0 disease, options include breast-conserving therapy or mastectomy and ALND with or without radiotherapy; (2) for T0N2-3M0 disease, NAC followed by axillary nodal dissection and mastectomy as for patients with locally advanced disease.12
The choice between local radiotherapy and total mastectomy represents a debatable therapeutic challenge. Scientific evidence shows that there is no difference between radiotherapy and surgery on the breast, revealing similar survival outcomes to patients who underwent mastectomy.17,18 While local radiotherapy has achieved effective therapeutic results, primary breast cancer may be identified in the precise location in mastectomy specimens.19 Each diagnostic method comes with its strengths and weaknesses, making it beneficial to combine multiple modalities for an effective breast cancer staging and treatment approach.20
Professionals in breast surgery and radiation oncology, who provide equivalent outcomes with various treatment options, face the task of guiding patients through decision-making. Themes like the fear of recurrence and physician preference are important, but defining and measuring patient preferences proves to be complex because of the psychological factors shaping decisions, the interplay between patients' risk assessments, and societal influences. Furthermore, when making the therapeutic decision, the patient's preference must be considered.21,22
In conclusion, OBC management requires precise evaluation. Opting for conservative treatment might be a viable choice in cases of triple-negative OBC, considering the complete pathological response achieved through NAC. De-escalating axillary surgery after NAC may be feasible but is still arguable. The choice between local radiotherapy and total mastectomy, with similar outcomes, demands individualized consideration respecting patient preferences. Healthcare professionals play a key role in integrating diagnostic modalities for effective management, emphasizing a personalized, multidisciplinary approach for optimal outcomes.
FundingThe authors declare that there are no public or private sources of funding for this article.
Ethical considerationsProtection of people and animals. The authors declare that no experiments have been conducted on humans or animals for this research. Confidentiality of data, right to privacy, and informed consent. The authors declare that patient consent was obtained for this article, and no patient data are disclosed.
Patient consentInformed consent was obtained from the patient for publication of this case report and accompanying images.