Occult breast carcinoma is very rare and will appear initially as metastatic with undetectable primary breast tumor. This is the first case described in the literature with thrombocytopenia as first clinical symptom.
El carcinoma oculto de mama es una rara entidad que suele debutar con afectación metastásica sin primario detectable. Este es el primer caso detectado en la literatura en el que un carcinoma oculta debuta como trombocitopenia.
Occult breast cancer (OBC) is a very rare subtype of breast cancer and is defined as a clinically recognizable metastatic carcinoma from an undetectable primary breast tumor on physical examination or imaging, or as the presence of axillary metastases without a breast primary seen on mammogram or ultrasound.1 It accounts for less than 1% of breast carcinomas.2 Metastatic OBC usually appears in axillary nodes, bone, or skin. Other rare sites of metastases have been described in the gastrointestinal tract,3 bone marrow,4 or orbit.5
Thrombocytopenia as first symptom only of OBC has never been reported. In OBC, the immunohistochemical profile of tumor cells must be consistent with the immunohistochemical findings of breast carcinoma. Imaging, including US, mammogram, MRI, and a whole-body CT will not identify any primary.
OBC can be picked up on MRI in 72% of cases, as this imaging has greater sensitivity and this is an important part of diagnostic workup according to the National Comprehensive Cancer Network guidelines for occult primary.6 However, there are cases that have not been visible on MRI but have had positive immunohistochemical profile in the breast tissue after mastectomy.
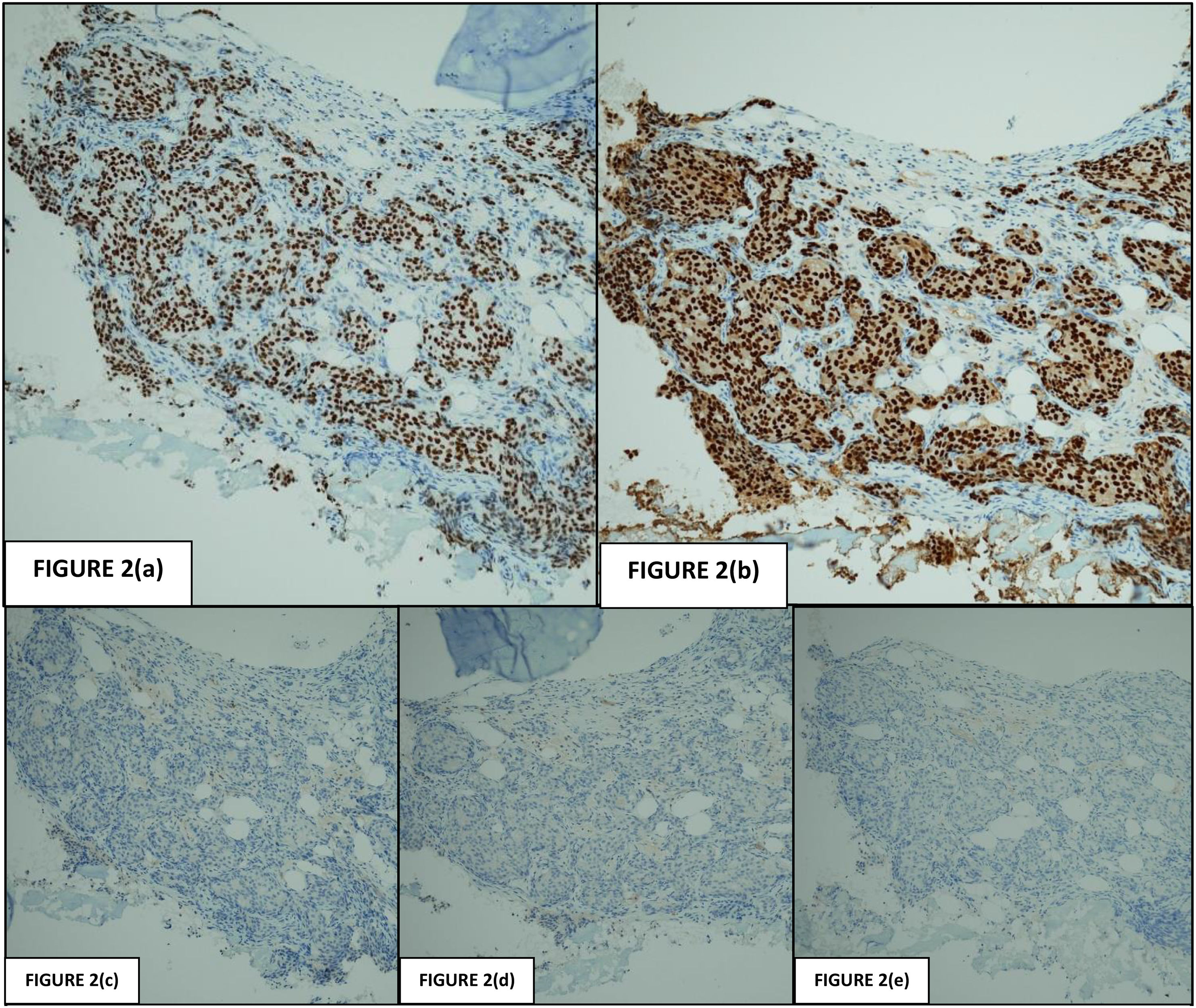
The typical immunohistochemical profile of a breast primary carcinoma is CK7+/CK20−, GATA3+, GCDFP-15+/−, mammoglobin+/−.7 Prognostic significance of IHC for occult disease is also controversial with conflicting reports of whether overall survival and disease-free survival are impacted. Occult bone marrow metastasis has been associated with a decrease survival.8 The treatment for OBC has also been up for debate. A 2016 meta-analysis concluded that the overall survival outcome was the same for patients with OCB who underwent mastectomy vs ALND and radiotherapy.9
This case report is unique as it describes a patient with negative axillary nodal status and metastatic bone marrow causing thrombocytopenia. Only one other case has been reported with anemia and thrombocytopenia simultaneously,4 but no one has ever been described with only thrombocytopenia as the first symptom to our knowledge in the literature reviewed.
Case reportA 69-year-old female was referred to the Hematology Department at Royal Bolton NHS Foundation Trust due to repeated moderate thrombocytopenia (45.000 plt, normal 150.000–400.000) detected by the General Practitioner at her surgery in a blood test as part of her checking for hyperglycemia. All the rest of the blood test were in normal limits. The patient's past medical history includes asthma, atrial fibrillation, and borderline diabetes mellitus.
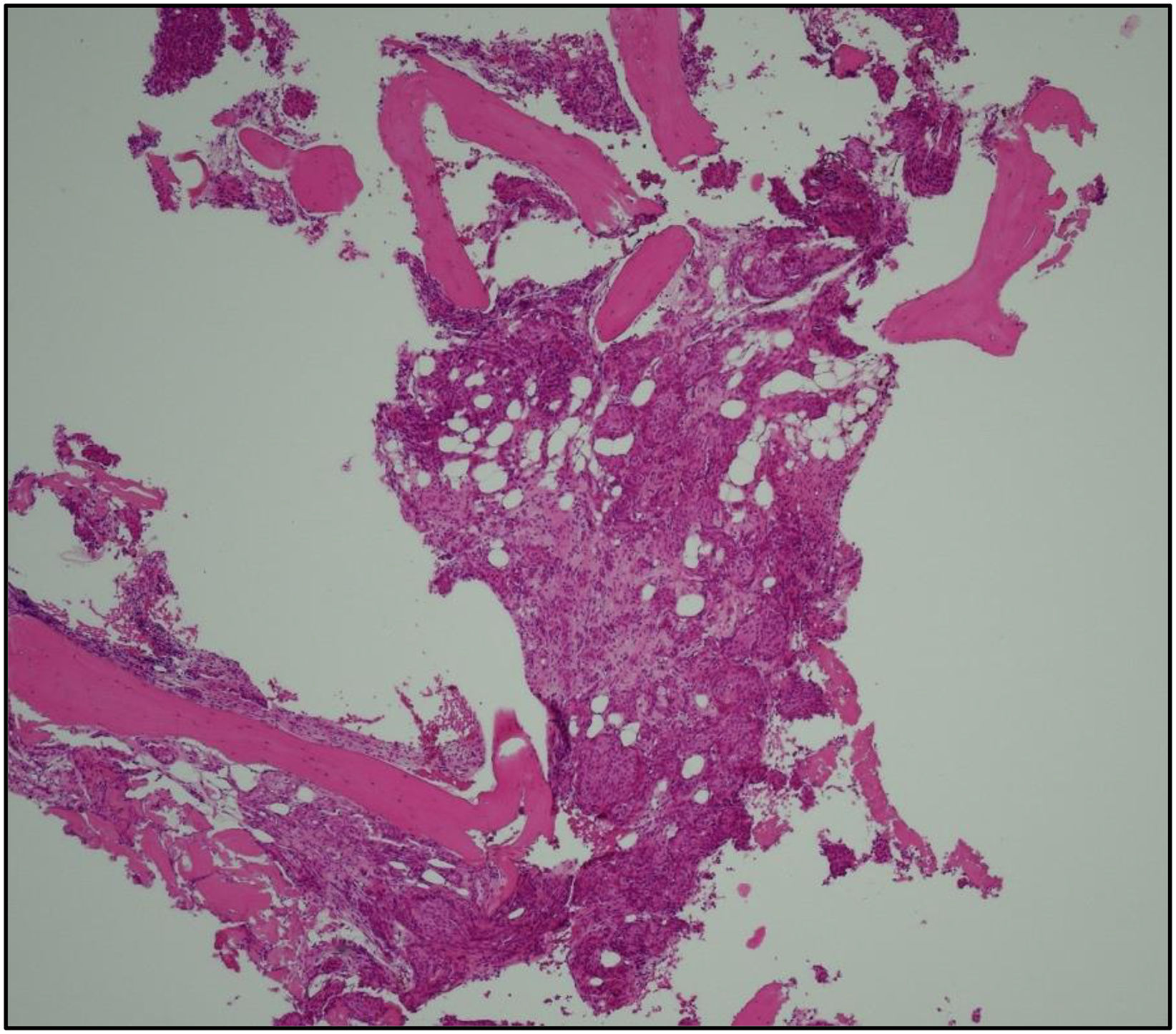
A routine bone marrow aspirate was performed at the Hematology Department and the trephine biopsy was found to be infiltrated by irregular nests and clusters of atypical cells with round to ovoid nuclei and moderate amounts of eosinophilic cytoplasm (Fig. 1). The immunohistochemistry was negative for CD45 and positive for CK7 and MNF116. It was negative for CDX2 and CK20. ER and PR were positive and HER2 was negative, GATA3 and mammoglobin were positive. TTF1, p40, and p63 were negative (Fig. 2). Proliferative index (Ki 67) was 15%. The profile was in keeping with metastatic breast carcinoma. Stage was T0 N0 pM1 (bone marrow).
The case was discussed in the breast MDT and the patient was appointed at the triple assessment clinic. The patient had felt no breast lump and most recent mammogram screening was 2 years prior (normal). On examination, there were no palpable lumps in either breast, only bilateral nodularity noted. No axillary nodes were palpable. US and mammogram showed no masses, mammogram only showed longstanding fibrotic changes. Tomosynthesis was normal. Contrast-enhanced MRI showed no masses or enhancements. CT thoraco-abdominal-pelvis staging scan showed no evidence of breast primary or other metastasis.
This patient was further discussed in the MDT in which it was decided that despite a lack of evidence of primary on imaging, the immunohistochemical profile was in keeping with metastatic breast cancer disease, and she was referred to Oncology to start with treatment.
DiscussionThis case is unique to our knowledge in the literature reviewed as the patient had no clinical findings of lymphadenopathy and no breast primary could be ascertained through any imaging, even MRI. The diagnosis based on immunohistochemical findings alone is extremely rare. Thrombocytopenia in a patient with cancer and bone marrow metastases may occur secondary to fibrosis induced by malignancy.10 Although the standard triple assessment approach was utilized for this case, it opens up a wider discussion around being confirmed outside of these parameters. It is difficult to gain an evidence base for OBC due to the rarity of disease. For sites of metastases other than axillary lymph nodes, this problem is clearly exacerbated. Most of the literature consulted to review prognosis and treatment includes patients in which the site of metastasis was the axillary lymph nodes. It is therefore important that these rare cases and its evolution are documented to gather more data.
FundingThe article did not receive any funding.
Patient consentThe authors declare that they have obtained the patient's consent for publication of the article.
Ethical considerationsThe authors declare that they have followed their institution's protocols on the publication of patient data and have obtained the appropriate permissions.