Occult breast cancer is a rare presentation of breast cancer (<1%), as an isolated axillary lymphadenopathy. It represents a diagnostic challenge, gradually improved by technological innovations. The difficulty in deciding therapeutic conduct lays in the paucity of prospective studies and thereby of consensus. We present a brief review of the literature, concerning the case report of a 56-year-old woman diagnosed with this type of cancer at our center, after presenting with an axillary nodule. No relevant abnormality in the breast or other organs was found. Immunohistochemical and imaging diagnosis are assessed as well as treatment, which consisted of homolateral axillary lymph node ressection, followed by chemotherapy, radiation therapy and hormone therapy.
El cáncer oculto de mama es una forma inusual de cáncer de mama (menos del 1%) y se presenta como una linfadenopatía axilar aislada. El diagnóstico supone un desafío, que gracias a las innovaciones tecnológicas está mejorando gradualmente. La dificultad en decidir la conducta terapéutica se debe a la escasez de estudios prospectivos y, por lo tanto, de consenso. Presentamos una breve revisión de la literatura, con relación al informe del caso de una mujer de 56 años, diagnosticada con este tipo de cáncer en nuestro centro, después de presentar un nódulo axilar. No se encontraron anomalías relevantes en la mama ni en otros órganos. Se evalúa el diagnóstico inmunohistoquímico y por imagen, así como el tratamiento que consistió en una resección homolateral de los ganglios linfáticos axilares, seguido de quimioterapia, radioterapia y terapia hormonal.
Occult breast cancer (OBC) is a subgroup of cancer of unknown primary site. It is characterized by an axillary metastasis, pathologically resembling from a breast cancer, with no abnormality on clinical nor diagnostic work-up.1,2 It accounts for less than 1% of all diagnosed breast cancers2–7 and its initial presentation as an isolated axillary lymphadenopathy is a clinical challenge.8 Treatment lacks consensus and tends to progressively become more conservative.
Clinical caseA 56-year-old women was admitted to our institution in January 2017 to clarify an asymptomatic right axillary lump. She was postmenopausal (2014), and besides having chronic hypertension, was otherwise healthy. Previous surgeries included 3 cesarean sections, tubal ligation and spine intervention. She presented no smoking habits or alcohol consumption; she denied previous intake of oral contraceptives or hormone replacement therapy, and had no relevant family history.
On physical examination, a right, hard, mobile, painless 3cm nodule was identified in the right axilla. No lumps in the left axilla, breasts or supraclavicular areas bilaterally were identified.
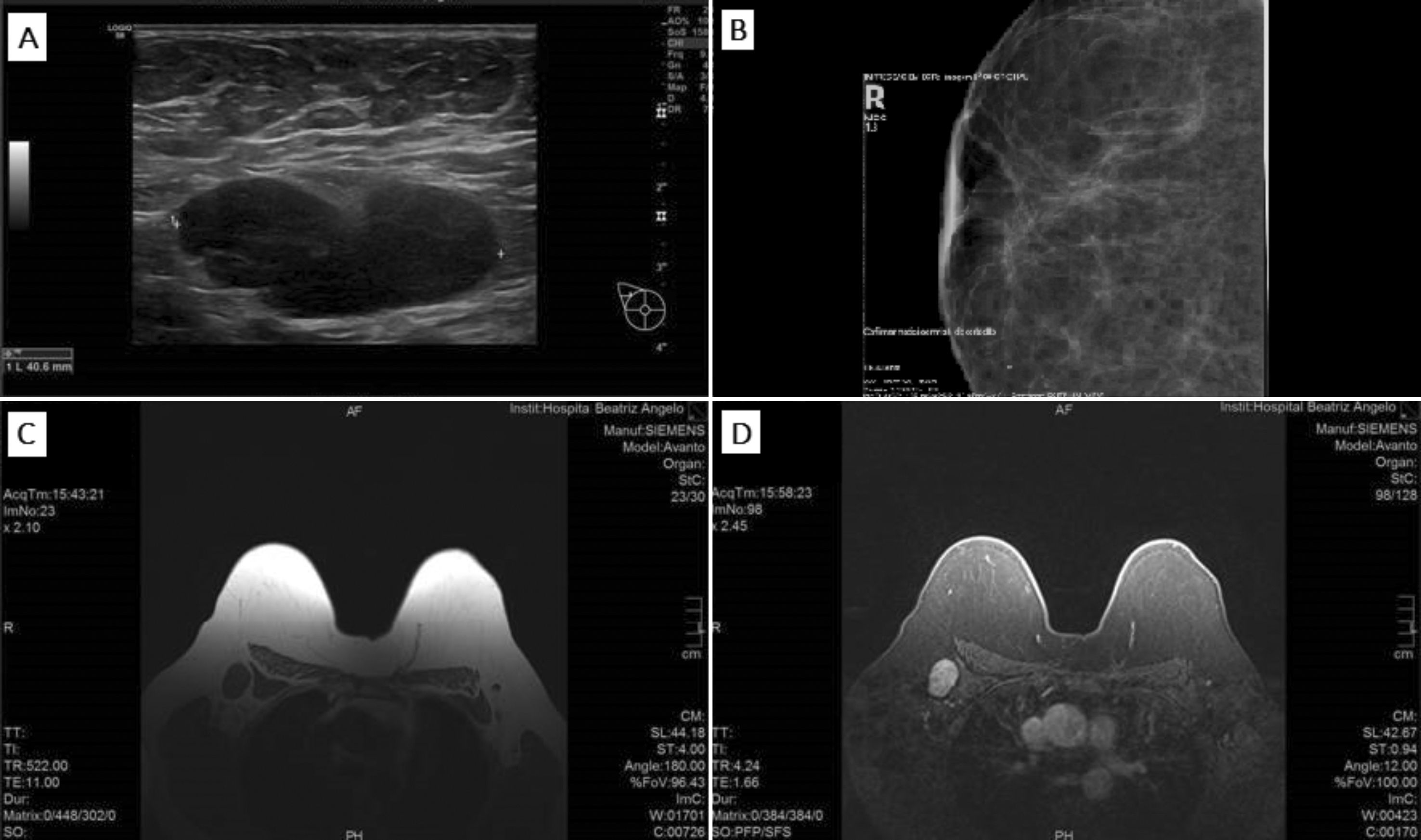
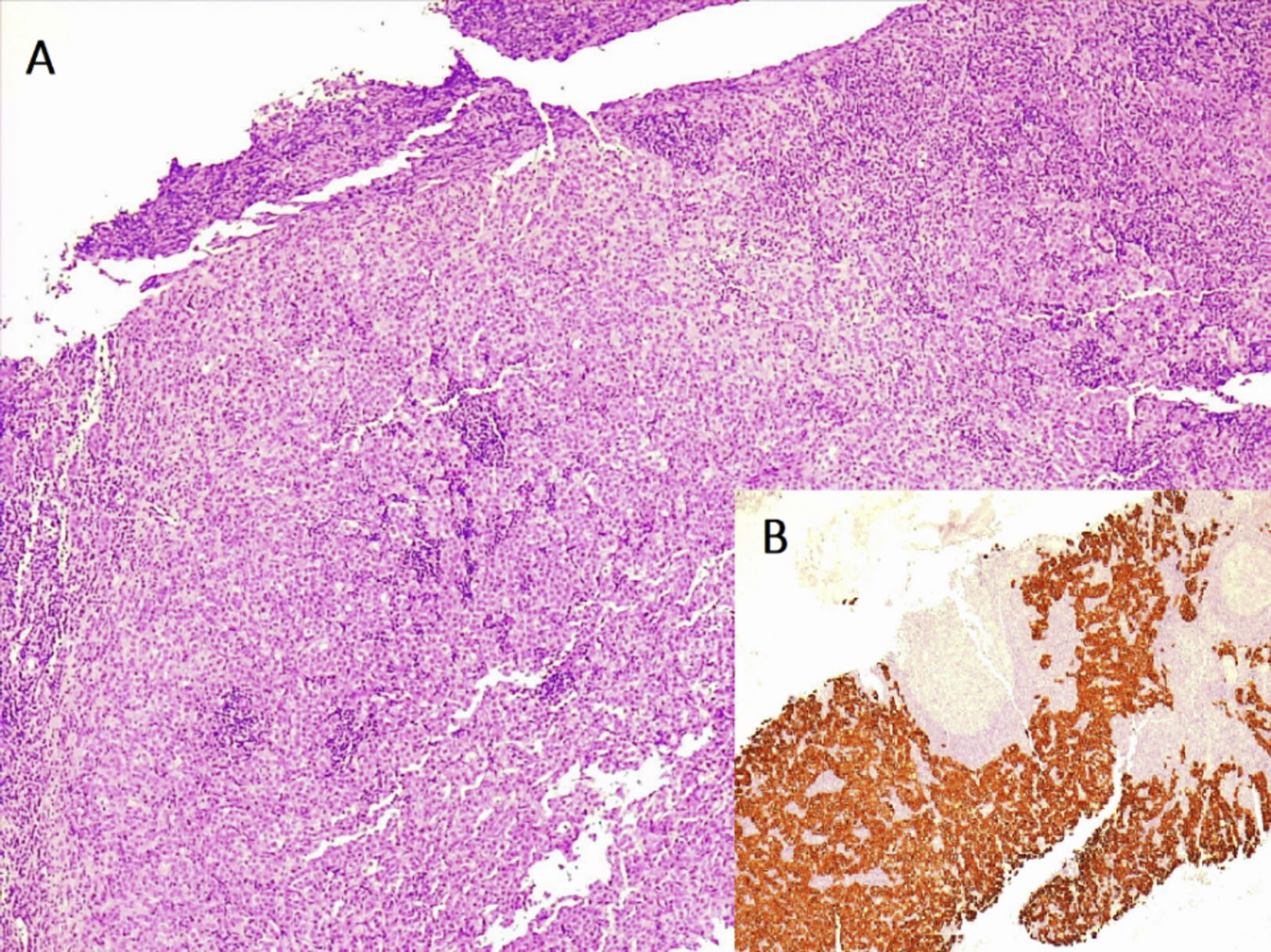
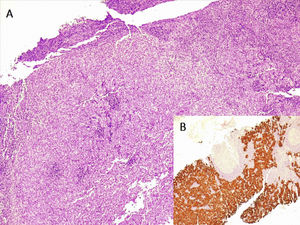
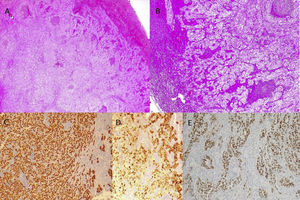
A bilateral mammogram (Fig. 1B) and a breast ultrasound were recently done in an imaging center outside the hospital, that were normal. Images were reviewed and a needle biopsy was performed (Fig. 1A). Pathological examination revealed a right axillary metastasis (Fig. 2). Immunohistochemical (IHC) results were: ER(+), CK7(+), CK20(−), RCC(−), GCDFP15(+), HER2(−), TFF1(−). Primitive breast cancer was the suspected etiology. She had recently done a colonoscopy and underwent breast MRI (Fig. 1C and D), whole body CT and bone scintigram – no other lesions were found.
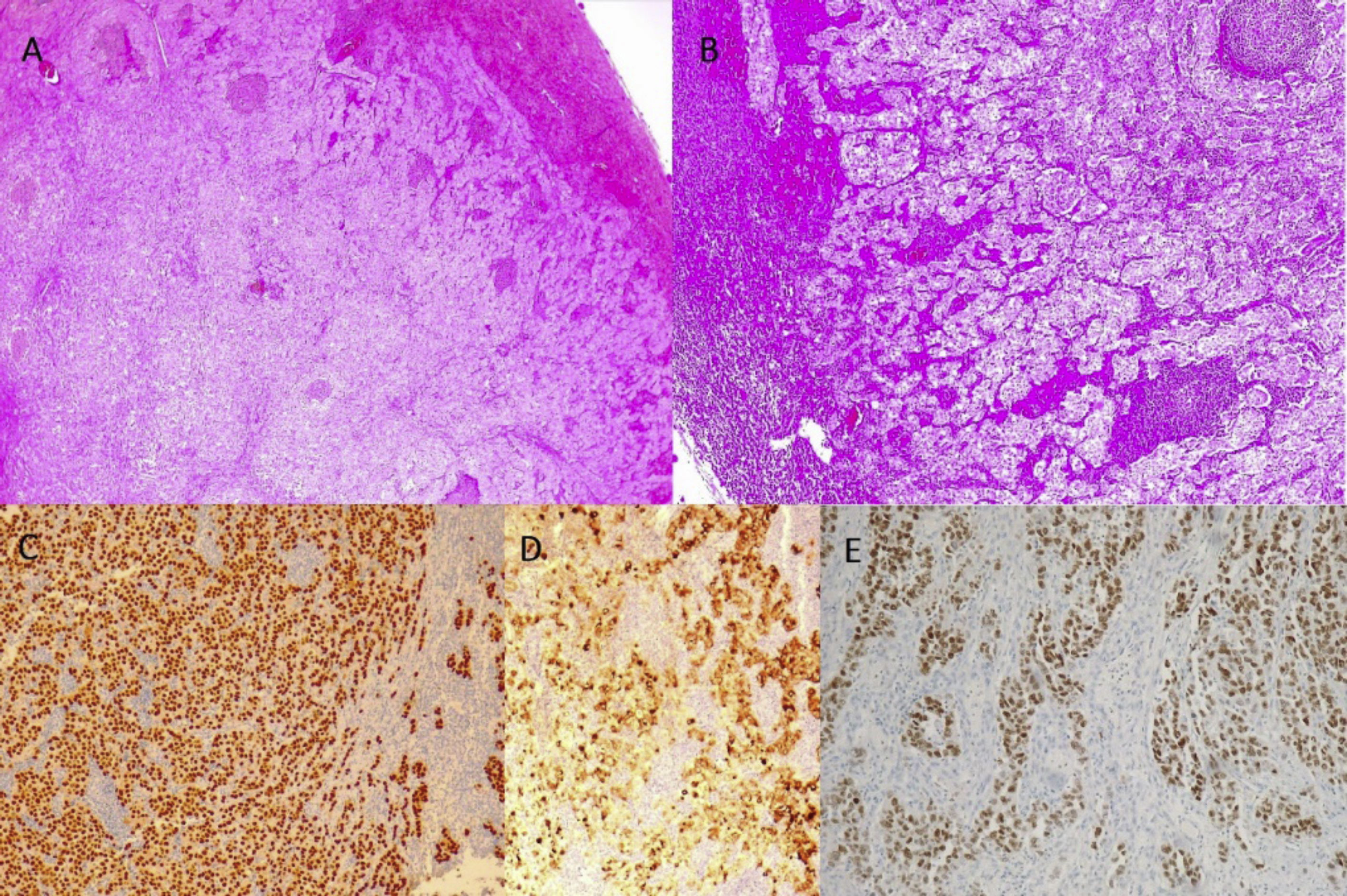
The patient was diagnosed with OBC and underwent right Axillary Lymph Node Ressection (ALND). Pathological examination showed 1/9 dissected lymph nodes with metastasis, ER 90%, PrR 30%, remaining IHC results confirmed (Fig. 3). The tumor-node-metastasis classification was T0N1a(1/9)M0, stage IIA.
Surgery was followed by chemotherapy with anthracyclines and taxanes, whole breast radiation therapy (WBRT) and HT with letrozole.
She has now 3 years of surveillance since surgery, maintains letrozole and mamography every year. No recurrence or distant metastasis was observed so far.
DiscussionA cancer of unknown primary site accounts for 4–5% of all invasive cancers.9 Despite generally having a poor prognosis,3,10 improvements have been made in treating some subgroups, namely OBC.10 Its peak incidence is 55 years old.11
Due to its low prevalence, studies tend to include diagnosis made throughout broad periods of time, when technological limitations hampered the identification of small breast carcinomas with a falsely increased diagnosis of OBC.12 Its incidence may be decreasing with more sensitive techniques, namely MRI.11
An isolated axillary lymphadenopathy relates more often to benign disorders.3 However, in women, when malignant, breast is the most common primary tumor site.3
IHC staining is an extremely useful tool for diagnosing the primary site but usually a broad panel is needed. Breast cancer usually expresses CK7 but does not express CK20, and rarely TFF1.3 ER and PrR supported the diagnosis of an occult breast primary.3 However, staining negatively would not exclude breast cancer2,4; in fact, hormonosensitivity is lower than in non-occult breast cancer.7 HER2 is generally not useful for differential diagnosis but may help in treatment decision.3 GCDFP15 is breast cancer specific in 65–80% of the cases3 and supports the diagnosis of OBC in our case.
During imagiologic work-up, a breast MRI is essential. It is able to detect a primary breast cancer up to 75–86% of women who present with axillary adenocarcinoma and a negative clinical examination and mammogram±ultrasound.1,3,7,12,13 Despite having a high false positive rate,3 MRI is now considered standard approach for evaluation of breasts in OBC patients.11,14
Other exams are less consensual: bone scan may be reserved for symptomatic women or those with elevated alkaline phosphatase3 and PET scanning is not indicated in stage II disease but may be helpful where standard staging studies are suspicious/equivocal.14
There is no clear consensus about optimal management – studies are usually small and retrospective3,12 and bigger ones comprise long period of data accrual with inevitable changes in clinical practice.12,15
Standard approach used to be a modified radical mastectomy, likely driven by the high percentage of patients whose primary tumor was found upon histological analysis.6–8 Nevertheless, rates have been decreasing.11,12
Mastectomy showed lower rate of local recurrence and superior disease free and overall survival than no local therapy.4,6 However, surgery became more conservative12,13 as studies demonstrated that mastectomy did not improve survival outcomes, locoregional recurrence or distant metastasis5 compared to breast conservative surgery (BCS). An upper-outer quadrantectomy (it was believed to represent the most likely primary site location15) and ALND (Sohn et al.8 showed no difference in overall survival between performing ALND alone, plus BCS or plus mastectomy) were described.
Radiotherapy also gained an important role in the treatment of OBC.1,2,4 ALND plus WBRT showed favorable locoregional recurrence,1,8,12 distant metastasis,8,12 survival4 and breast cancer-specific survival1,8,12 rates compared to ALND alone. Recent NCCN guidelines recommend either mastectomy plus ALND or ALND plus WBRT, with or without nodal irradiation for T0N1M0 disease.14
Regarding adjuvant systemic therapy, NCCN recommends systemic chemotherapy, endocrine therapy and biologic therapy (anti-HER2 monoclonal antibody) according to the same indications as for stage II and III disease.2,6,8,14
Based on the diagnostic and stage work-up, we believe this to be an OBC case. ALND plus WBRT, chemotherapy and HT were performed but anti-HER2 monoclonal antibody was not suitable considering IHC profile.
OBC has a five-year survival rate averaging 75%3 and axillary lymph node status (number of positive nodes) was pointed as the most important prognostic factor.12 With one positive node, we believe this patient has a good prognosis.
Despite obvious need for prospective randomized controlled trials, they will unlikely be performed,12 as low incidence makes it challenging.6 With time, probably there will be more homogeneous and larger retrospective studies with diagnosis of true OBC based on negative MRI.11
Meanwhile, other approaches may be established – some studies defend the use of neoadjuvant systemic therapy, sentinela lymph node biopsy7 or systemic and axillary treatment, with no need for mastectomy or WBRT11 (Terada et al.11 suggested that some cases may be a primary tumor arising from ectopic breast tissue in axillary lymph nodes).
FundingThis work has not received any funding.
Confidentiality of dataThe authors declare that they have followed the protocols of their center on the publication of patient data.
Conflict of interestThe authors declare that they have no conflict of interest.