Gender violence is a health problem with legal consequences. Health professionals must notify these cases to the judicial authority through injury reports. The aim of this study was to analyse the quality of injury reports in gender-based violence cases, assessing whether the recommendations of health protocols are being followed.
Material and methodsA retrospective study in a sample of 474 documents issued in cases with suspicion of gender-based violence was carried out. A scale was developed and applied to assess their quality.
ResultsMost of the mandatory reporting documents were of medium quality. In 90% of cases data referring to medical staff, women and primary health care were reflected. Likewise, gender violence and the type of violence were specified in 80%. The most widespread deficiencies related to the history of abuse, which were only incorporated in 15% and reference to whether the patient came alone or accompanied in 9%. In addition, more than 72% of documents had abbreviations. The best injury reports were made in primary care facilities.
ConclusionsThe quality of injury reports is related to the structure of documents and their origin, highlighting the importance of having a standard document, as well as the need to improve training and awareness of health professionals.
La violencia de género es un problema de salud con repercusiones jurídicas. Los/las profesionales sanitarios/as deben comunicarlo a la autoridad judicial a través del parte de lesiones. El objetivo de este estudio ha sido analizar la calidad de los partes de lesiones elaborados en casos de violencia de género, valorando si se siguen las recomendaciones de los protocolos de actuación sanitaria.
Material y métodosSe realizó un estudio retrospectivo en una muestra de 474 documentos emitidos en casos con sospecha fundada de violencia de género. Se elaboró y se aplicó una escala para valorar su calidad.
ResultadosLa mayoría de los documentos tenían una calidad media. En el 90% de los casos se reflejaron datos referidos al personal facultativo, a la mujer y a la primera atención sanitaria. Asimismo, la especificación de violencia de género y el tipo de violencia se cumplimentaron en el 80%. Las deficiencias más extendidas estaban relacionadas con los antecedentes de maltrato, que solo se incluyeron en el 15%, y la referencia a si la paciente acude sola o acompañada, en el 9%. Además, el 72% de los documentos presentaban abreviaturas. Los mejor elaborados fueron los partes de lesiones procedentes de atención primaria.
ConclusionesLa calidad de los partes de lesiones tiene relación con la estructura de los documentos y su procedencia, poniendo de manifiesto la importancia de contar con un documento estándar, así como la necesidad de mejorar la formación y sensibilización de los/las profesionales sanitarios/as.
Gender-based violence is a health problem with legal repercussions. Healthcare professionals play an important role here, as they have to respond to clinical aspects as well as medical and legal ones. Their responsibilities include reporting mistreatment to the judicial authority using an injury report.1
Preparing and sending this report is a legal2,3 and professional ethics4 imperative, with the primary aim of protecting the victim. The importance of the injury report lies in the fact that, as it is usually prepared at a time close to the aggression, it is often the only proof of a possible crime. It is also extremely important for the subsequent forensic report, as the lesions have often disappeared by the time this examination of the woman takes place.5 It is also highly useful in bringing about the application of protective measures1 and supporting the victim’s testimony.6,7 It is important as legal proof, whether the victim decides to report the crime or not, in case she decides to do so in the future, when it is used as evidence for the habitual and repetitive nature of the violence.8,9 The lack of documentary proof, above all in cases of psychological violence, may lead to absolution of the accused party.6,10
There has been debate about which model would be recommendable for the injury report. On the one hand, some healthcare professionals believe that, due to the particular characteristics of gender-based violence, there should be a specific form which would make medical personnel more sensitive to the subject.9 However, others believe that the excessive amount of bureaucracy in medical departments hinders their work, and they are in favour of using the same form for all incidents.11 Both parties agree that any standardised type of document always facilitates, simplifies and promotes equity.8 If the form is not specifically for gender-based violence, this must be made clear so that the document can be sent using the routes established for such cases.1
The majority of medical facilities use standardised documents in printed or electronic format, based on the recommendations of medical intervention protocols and prepared at national1 or regional level.12 Nevertheless, these documents are often not properly completed.13,14 This may lead to problems in how the document is interpreted by the forensic doctor in question, and as a result of this it may have repercussions in the judicial sentence.
The general objective of this study was to analyse the quality of injury reports in cases of gender-based violence. More specifically, the aim was to evaluate whether medical intervention protocols were followed, and to discover whether any differences exist depending on the structure or medical department which issues these forms.
Material and methodsStudy designThis is a retrospective study of 474 documents (injury reports and primary care medical reports), issued in cases of gender-based violence during the period from 2009 to 2016, with an open judicial procedure in the courts of Pontevedra, Cangas, Cambados, Marín and Caldas.
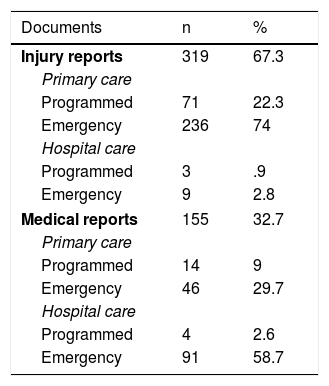
Sample selectionThe study sample was mainly composed of standardised injury reports. In one third of the cases primary care medical reports were reviewed, as these functioned as injury reports for forensic evaluation. Both groups were considered together for the purpose of content analysis. The majority of the documents were prepared in primary care or hospital Emergency Departments, as is shown in Table 1.
Documents analysed according to care structure (N = 474).
| Documents | n | % |
|---|---|---|
| Injury reports | 319 | 67.3 |
| Primary care | ||
| Programmed | 71 | 22.3 |
| Emergency | 236 | 74 |
| Hospital care | ||
| Programmed | 3 | .9 |
| Emergency | 9 | 2.8 |
| Medical reports | 155 | 32.7 |
| Primary care | ||
| Programmed | 14 | 9 |
| Emergency | 46 | 29.7 |
| Hospital care | ||
| Programmed | 4 | 2.6 |
| Emergency | 91 | 58.7 |
Cases classified as gender-based violence according to Law 1/200415 were included (women maltreated by their partner or ex-partner), excluding cases violence against women perpetrated by individuals other than their partner or ex-partner. The forensic reports were also reviewed, to properly evaluate the injury reports. This made it possible to check the described injuries as well as their causal link with the mechanism described.
Preparation and application of the quality criterionA criterion was prepared to evaluate the quality of the documents, based on another one that had been described previously,14 and taking into account the recommendations of the current protocols.1,12
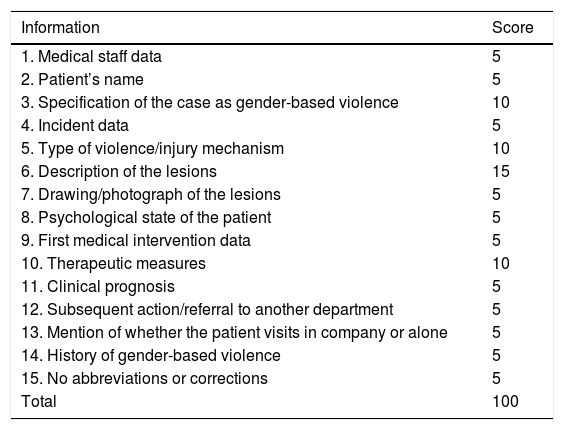
Table 2 shows the data which have to be included in the injury reports, together with the score awarded to each one of them. Medical staff data were given 5 points if they included the name and/or the number of the doctor. For the incident, 5 points were awarded when at least 2 descriptive data about the same were shown (the date, time and place). The description of the injuries was awarded 5 points if it included the type of injury, and 5 more points were awarded if it described the location of the injury, together with 5 points more if it described an additional characteristic (number, colour, shape or size). The documents with at least 2 data describing the medical care (date, time hospital/department) were awarded 5 points. Of the required information was not shown, 0 points were awarded. After adding up all of the sections, the maximum score possible would be 100 points.
Variables included in the criterion, and score.
| Information | Score |
|---|---|
| 1. Medical staff data | 5 |
| 2. Patient’s name | 5 |
| 3. Specification of the case as gender-based violence | 10 |
| 4. Incident data | 5 |
| 5. Type of violence/injury mechanism | 10 |
| 6. Description of the lesions | 15 |
| 7. Drawing/photograph of the lesions | 5 |
| 8. Psychological state of the patient | 5 |
| 9. First medical intervention data | 5 |
| 10. Therapeutic measures | 10 |
| 11. Clinical prognosis | 5 |
| 12. Subsequent action/referral to another department | 5 |
| 13. Mention of whether the patient visits in company or alone | 5 |
| 14. History of gender-based violence | 5 |
| 15. No abbreviations or corrections | 5 |
| Total | 100 |
The quality of the documents was classified on the basis of adding the scores in all of the sections. It was divided into high quality: >70 points; medium quality: 50–70 points, and low quality: <50 points.
Statistical analysisA descriptive analysis was carried out of the variables using absolute frequencies and percentages. A comparative analysis was also performed using the Chi-squared test. Three comparisons were made: the injury report was compared to the primary care medical report, the primary care report was compared to the hospital report, and emergency care was compared to programmed care. A 5% level of significance was assumed. The statistical program R (R Core Team 2018) was used for the study.
Ethical aspectsThis study was undertaken while respecting current law regarding personal data processing and protection. Disassociated information was used which prevents the identification of those involved, and all of the members of the research team committed to confidentiality. This study was assessed and approved by the Research Ethics Committee of Galicia (Santiago-Lugo Territorial Committee), with number 2015/553.
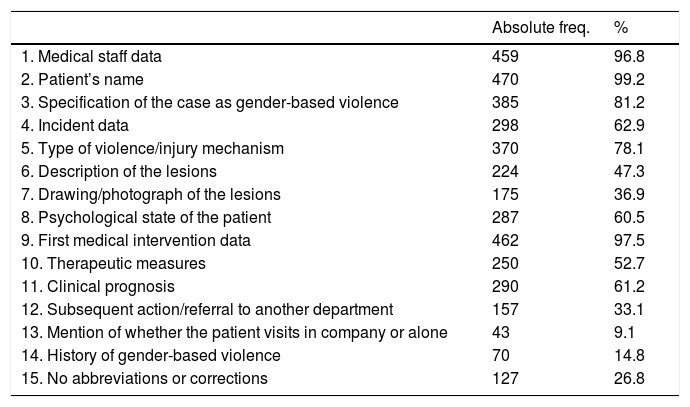
ResultsTable 3 shows the number of documents reflecting each one of the recommended data, with the corresponding percentage. The majority of the injury reports contained the personal details of the medical staff who supplied care, as well as the personal data of the women and their relationship with the alleged attacker.
Degree of compliance with the data included in the criterion.
| Absolute freq. | % | |
|---|---|---|
| 1. Medical staff data | 459 | 96.8 |
| 2. Patient’s name | 470 | 99.2 |
| 3. Specification of the case as gender-based violence | 385 | 81.2 |
| 4. Incident data | 298 | 62.9 |
| 5. Type of violence/injury mechanism | 370 | 78.1 |
| 6. Description of the lesions | 224 | 47.3 |
| 7. Drawing/photograph of the lesions | 175 | 36.9 |
| 8. Psychological state of the patient | 287 | 60.5 |
| 9. First medical intervention data | 462 | 97.5 |
| 10. Therapeutic measures | 250 | 52.7 |
| 11. Clinical prognosis | 290 | 61.2 |
| 12. Subsequent action/referral to another department | 157 | 33.1 |
| 13. Mention of whether the patient visits in company or alone | 43 | 9.1 |
| 14. History of gender-based violence | 70 | 14.8 |
| 15. No abbreviations or corrections | 127 | 26.8 |
The incident data shown were mainly the type of violence, the mechanism of injury and the data of the event (>70%). Although the place and time were generally shown, this was to a lesser degree (±60%).
The type or location of injuries are shown in more than 90% of the documents. On the contrary, other important data for correct characterisation of the same such as shape, size, colour or time of development were included in fewer than 10% of the documents. 40% of the cases specified the number of injuries, and about 37% of the documents contained a body diagram showing the location of the injuries, although no photographs were taken in any case. The psychological state of the woman was described in 60% of cases.
The data associated with the first medical attention, such as the date, time, city, hospital or department were filled in in more than 90% of the documents. The therapeutic interventions and clinical prognosis were shown in 53% and 61% of the cases, respectively. Other data such as the need to hospitalise the patient, referral to another department or whether the woman visited alone or in company were less relevant.
Approximately 15% of the documents refer to the background of gender-based violence, which in 13% of cases was physical and in 7% it was psychological. Hardly any data were included on the commencement and frequency of the violence or any previous reports. Almost 57% of the documents were computerised and somewhat more than 61% were written in legible lettering. 73% contained abbreviations and/or corrections.
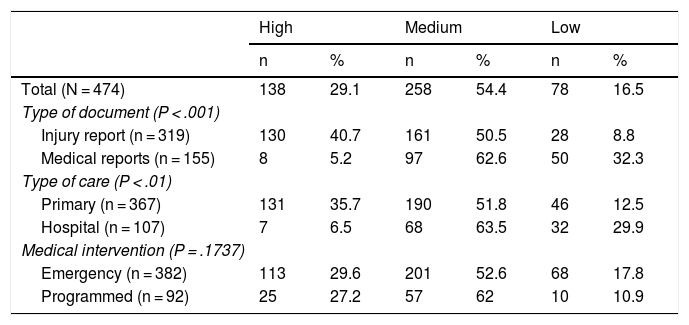
Respecting the overall score, the lowest score was 15 and the highest was 90, with an average of 62.74 points (median 65 and standard deviation 14.86). As may be seen in Table 4, medium quality documents predominated throughout the sample.
Document quality according to the criterion.
| High | Medium | Low | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total (N = 474) | 138 | 29.1 | 258 | 54.4 | 78 | 16.5 |
| Type of document (P < .001) | ||||||
| Injury report (n = 319) | 130 | 40.7 | 161 | 50.5 | 28 | 8.8 |
| Medical reports (n = 155) | 8 | 5.2 | 97 | 62.6 | 50 | 32.3 |
| Type of care (P < .01) | ||||||
| Primary (n = 367) | 131 | 35.7 | 190 | 51.8 | 46 | 12.5 |
| Hospital (n = 107) | 7 | 6.5 | 68 | 63.5 | 32 | 29.9 |
| Medical intervention (P = .1737) | ||||||
| Emergency (n = 382) | 113 | 29.6 | 201 | 52.6 | 68 | 17.8 |
| Programmed (n = 92) | 25 | 27.2 | 57 | 62 | 10 | 10.9 |
When we compare the information included in the injury reports with the medical reports, we find statistically significant differences depending on the type of document (P < .001). Although medium quality documents predominated in both groups, the majority of high quality documents were injury reports, while the majority of low quality ones were medical reports (Table 4).
We also found statistically significant differences when comparing document quality according to the nature of the issuer: primary care services as opposed to hospital departments (P < .01). Although average quality documents predominated in both groups, there were more high quality documents issued by primary care (Table 4).
Comparison of document quality according to the type of medical care (emergency as opposed to programmed) showed no statistically significant differences, as may be seen in Table 4.
DiscussionIt is indispensable that injury reports be properly prepared for the correct care and treatment of cases of gender-based violence and to establish effective preventive measures. In spite of this, the quality of the said documents has hardly been studied in the literature.14
The majority of the documents analysed were prepared in primary care or hospital emergency departments, in numbers even higher than those described by other authors.14 These differences may be due to the different ways departments are organised and their working hours in different autonomous communities. In this study, standardised injury reports were used more in primary care surgeries than they were in hospitals, and they were also used more in programmed vs emergency care. This may be associated with having more time to carry out the clinical interview of the patient.
Respecting the information contained in the documents, we found that they often include the data of the medical staff and the patient’s name, and this finding coincides with those of other studies.14 This information was included in the standardised reports above all, which contained specific places for it, especially those prepared in primary care departments and programmed visits.
Regarding the episode of mistreatment, the protocols advise reporting whether it was a case of gender-based violence, as this affects how the report will be processed, and this was shown in more than 80% of the documents, a similar percentage to the one described by García Minguito et al.14 Another recommendation is to include data which describe the incident and the type of violence, and this was shown in the majority of cases in our series (63% vs 54%), above all in the standardised reports used in primary care. The type of violence and the mechanism of injury were shown in 78% of cases, above all in the standardised reports used in primary care. These aspects were not evaluated by García Minguito et al.14 in their study.
The type and location of the injuries were described in the majority of cases, although this was not the case for their number, which was shown in fewer than half of the reports. In a similar way to the findings of Linares-González et al.,16 other characteristics were shown in far fewer cases (less than 10% of the documents), and this sometimes hindered the determination of the patient’s evolution, which is important to establish injury data. Nor were photographs of the injuries included, even though this is recommended by the intervention protocols. However, in 37% of the cases a diagram of the body was included which indicated the location of the lesions. These diagrams were only shown in the standardised injury reports, as they include a sketch of the human body, and these diagrams only appeared in the documents prepared in primary care.
When preparing an injury report it is important to describe the psychological state of the woman. This was shown in 60.5% of the documents, above all the ones prepared in primary care, and this figure is clearly higher than the one described beforehand, of 28%.14 The reason for the poor result corresponding to this datum in other series has been attributed to the lack of psychological assessment in cases of mistreatment, as it is less evident than physical injuries.
The majority of the data which describe the first medical care given were mainly contained in the standardised reports and those drawn up in hospitals. The therapeutic measures applied are also considered to be important, as they show the scope of the injuries. These measures were described in more than half of the cases, although the study by García Minguito et al.14 reports a figure of less than 78% of cases. The clinical prognosis is an important datum for penal classification, and it was shown in 61% of the cases, chiefly in the standardised reports used in primary care. On the other hand, the description of whether the patient visited alone or in company, which could be an indicator of social support for them, was not included very often and was mainly given in hospital medical reports.
Respecting the plan for action after the first assistance, the protocols advise including information as to whether the patient was admitted to hospital, referred to another department or discharged. Almost 33% of the documents mentioned referral to another department, above all the reports drawn up in hospitals. It is also important to know whether there is a history of violence using records of previous injuries, if there were any, as this would make it possible to classify each mechanism of injury with its consequences, for subsequent forensic evaluation and a judicial report. Almost 15% of the documents contained a reference to previous attacks, and they were mainly primary care reports, which coincides with the findings of other studies.14
Although these documents are now usually completed by data transmission, if they are filled out manually it is advisable not to use abbreviations or corrections, as these may be interpreted as manipulation. In the sample we analysed less than 27% of the documents had no corrections or abbreviations, and similar figures are described in the literature.14
After applying the criterion we were able to establish that the majority of the documents were of average quality, which agrees with the results obtained by García Minguito et al.14 and Linares-González et al.16 A higher proportion of the high quality documents were standardised injury reports prepared in primary care. On the other hand, a higher proportion of hospital medical reports were low quality.
ConclusionsEvaluation of the documents prepared to inform the judicial authority of the facts in cases of gender-based violence showed that average quality ones predominate. They contain important deficiencies in describing data that are important for subsequent judicial and forensic actions, such as specific characteristics of the lesions and reference to previous attacks, among others. Document structure and origin are associated with better completion of the data, showing the importance of using a standard form that helps medical personnel to correctly report cases. Although this study was restricted to a specific geographical area and the results cannot be extrapolated, it shows the need to improve the training and sensitivity of medical professionals when completing injury reports in situations of gender-based violence, given the importance of this for case resolution.
FinancingThis study received no specific support from public or private sector bodies or not-for-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.
This work was made possible thanks to the collaboration of the Pontevedra office of the Legal Medicine Institute of Galicia and that of the courts of Cangas, Cambados, Marín and Caldas, which allowed us access to the information.
Please cite this article as: Diéguez Méndez R, Medrano Varela M, Rodríguez Calvo MS. Calidad de los partes de lesiones por violencia de género en la provincia de Pontevedra. Rev Esp Med Legal. 2021;47:99–104.