Injury reports are medico-legal documents containing the required information about injuries (from accidental, criminal or self-inflicted origin) to be delivered to the judicial authority. Nevertheless, forensic routine work suggests a high rate of inadequate or erroneous injury reports. This hinders forensic evaluation and, consequently, damage repair. The main objective of this paper is to evaluate the quality of the completion of injury reports issued by Primary Care and Emergency services in Córdoba, Spain, by using a new scale, as well as to identify the most prevalent mistakes made during that completion.
Material and methodsDescriptive cross-sectional and retrospective study conducted on 127 injury reports issued by Primary Care and Emergency services selected from the archive of the Institute of Legal Medicine and Forensic Science of Córdoba, using consecutive sampling, between 1 January 2015 and 30 June 2015. A quality scale of our own creation was then applied to them.
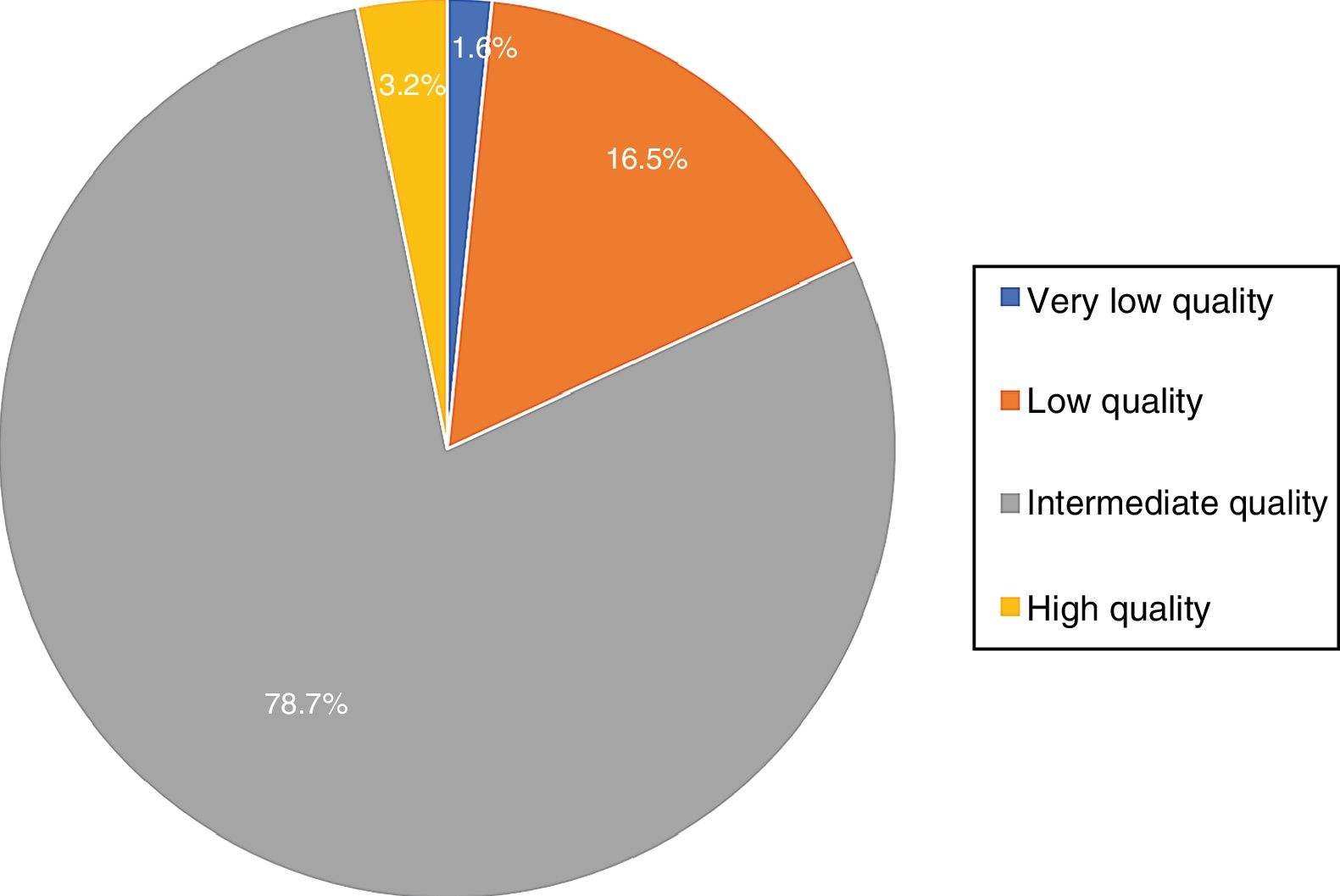
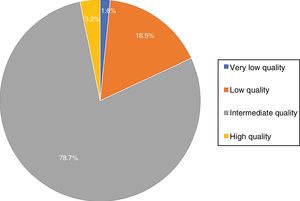
ResultsThe analysis showed that 18.1% of injury reports are of low or very low quality, while the majority (78.7%) are considered as intermediate quality. Nevertheless, most of them are very poorly described – with the lowest scores – in relation to strictly medico-legal parts; the description of the injury, including type, dimension and evolutionary stage.
ConclusionsThe study shows the poor quality of the injury reports issued by Primary Care and Emergency services within the province of Córdoba. Further strategies are needed in order to improve the completion of these medico-legal documents.
Los partes de lesiones son documentos médico-legales que contienen la comunicación a la autoridad judicial de cualquier lesión consecuencia de una conducta delictiva, accidental o autoinflingida. La experiencia diaria indica una elevada prevalencia de cumplimentación incompleta o errónea, lo que dificulta la tarea del médico forense y, con ello, la posterior reparación del daño producido a la víctima. El objetivo de este trabajo es evaluar la calidad de la cumplimentación de los partes de lesiones emitidos por Atención Primaria y Urgencias en el ámbito provincial de Córdoba mediante la propuesta de una escala e identificar los errores más prevalentes cometidos durante dicha cumplimentación.
Material y métodosEstudio descriptivo, transversal y retrospectivo. Se seleccionaron 127 partes de lesiones del archivo del Instituto de Medicina Legal y Ciencias Forenses de Córdoba, emitidos por los servicios de Urgencias y Atención Primaria entre 1 de enero y 30 de junio de 2015, mediante un muestreo consecutivo, y se les aplicó una escala de calidad de realización propia.
ResultadosEl 18,1% de los partes de lesiones son de baja o ínfima calidad, encuadrándose la mayoría (78,7%) como de calidad intermedia. No obstante, la generalidad de los partes son muy defectuosos en los apartados estrictamente médico-legales, que son los relacionados con la descripción de las lesiones (localización, tipo, dimensión y estado evolutivo de las mismas), que han obtenido las puntuaciones más bajas.
ConclusionesSe demuestra la deficiente calidad de los partes de lesiones emitidos por los servicios de Atención Primaria y Urgencias en nuestra provincia y se hace necesaria una estrategia para mejorar la cumplimentación de estos documentos médico-legales.
Injury reports are included within what we know as medical–legal documents, that is, all of the written communications by which doctors liaise with the authorities, official bodies, the public and private individuals in general.1,2 More specifically, the case covered here concerns the document which informs the judicial authority of any injury that may constitute an offense, including those which are accidental in origin, criminal or self-inflicted. The purpose of this document is to ensure that the said authority is aware of the fact and its consequences, so that it is able to undertake the relevant investigation and, if applicable, adopt suitable measures respecting the author.2–4
Documents of this type are widely used in normal medical practice, regardless of the speciality in question or the way in which medicine is practiced. Although it is true that in our country they are usually prepared by Primary Care and Accident and Emergency professionals, few doctors will not at some stage of their career have had to fill out an injury report, while ensuring that they do so correctly.
Such widespread usage is firstly the result of the large number of injuries seen by healthcare services which should be reported. Only in the year 2016, 365,202 offenses were committed, of which 15.1% corresponded to injuries (55,272).5 Injuries resulting from gender-based violence have to be added to this figure, as they are counted in independent data bases. This also applies to industrial accidents, which amounted to a total of 1,299,632,6 and traffic accidents (102,362 traffic accidents with victims, resulting in 9755 hospitalised patients and 130,635 non-hospitalised injuries).7 Secondly we should recall the obligation established by art. 262 of the Criminal Indictment Law for all citizens in general to report criminal offenses, and more specifically for doctors to report aiding an injured person. This is established by art. 355 of the Criminal Indictment Law: “[…] the doctors who treat an injured person will be obliged to prepare a report on their condition”.8 This legal obligation is also contained in the Penal Code, which describes the offenses of omission to punish crimes, while there is also the offense of refusing to aid justice (articles 408 and 412).9
Due to all of the above reasons we believe that it is fundamental for all doctors to be aware of the importance of this document and the need to fill it out correctly. Nevertheless, the personal everyday experience of forensic doctors indicates that a high proportion of reports are filled out incompletely or even erroneously. This hinders our working and is therefore also an obstacle to the subsequent redress of the damage caused to the victim, which will finally be determined by the competent court or judge.
There is therefore a need to properly evaluate the quality of injury reports, and to do so is the main objective of this study. Likewise, it also aims to discover the most common errors committed in preparing these reports, so that they can be avoided and thereby create a good quality document that aids the assessment work of forensic doctors and correct evaluation by the judge. This will lead to a just punishment for guilty parties and/or economic compensation for the injured.
Material and methodsThe experimental design is descriptive, transverse and retrospective, and it is based on analysis of 127 injury reports in cases assessed by the Legal Medicine and Forensic Science Institute, Córdoba. Consecutive sampling was used for inclusion in the study, from 1 January 2015 until the previously determined sample size had been attained. This is therefore a random sample of 127 documents (injury reports), which is calculated to be sufficient to estimate, at 95% confidence and a precision of ±7.5 percentage units, a population percentage that may be foreseen to stand at around 75%.
The documents studied originate in the injury report registry in the Legal Medicine and Forensic Science Institute, Córdoba, according to the following selection criteria: injury reports were selected that had been issued by Accident and Emergency and Primary Care from 1-1-2015 to 30-6-2015. They cover non-mortal physical injuries and exclude those which only mentioned psychological harm or injuries that were visually undetectable.
The study protocol was reviewed and approved by the Teaching and Research Commission of the Legal Medicine and Forensic Science Institute, Córdoba and the Research Ethics Committee of Reina Sofía Hospital, Córdoba. The study was conducted according to the rules governing good clinical practice, and it fulfils the ethical precepts contained in the Helsinki Declaration.
The main study variable is the quality of injury report content, which is defined by the following secondary variables:
- 1.
Data of the hospital or medical department where treatment was given.
- 2.
Data identifying the doctor who gave treatment.
- 3.
Personal data of the injured individual.
- 4.
Alleged cause.
- 5.
Location of the injury.
- 6.
Type of injury.
- 7.
Size of the injury.
- 8.
Evolution of the injury.
- 9.
Psychological and emotional state of the victim at the moment of treatment.
- 10.
The need for additional tests.
- 11.
Therapeutic measures applied.
- 12.
Action plan.
- 13.
Clinical prognosis.
- 14.
Description of how the actions occurred.
- 15.
Date and time of treatment.
- 16.
Data of the supposed aggressor.
- 17.
Clear and legible writing.
- 18.
The presence of corrections.
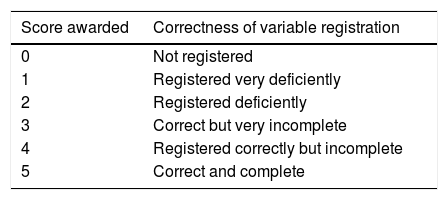
We created a Likert-type scale to evaluate the quality of reports, in which each one of the variables is given a numerical score depending on how suitable it was (Table 1).
This scale measured the 2 major problems which arise when preparing an injury report: the lack of data or the existence of incomplete data, together with faults in the description of actions and their consequences. For the score on the scale, we considered the presence of erroneous or inappropriate items to be “very deficient”, while the existence of vague terminology or terms considered to be unscientific were scored as “deficient”.
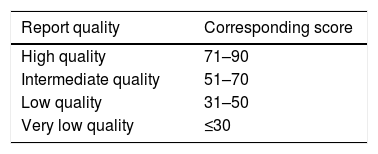
After scoring each variable according to the scale described above, the scores for each one of the reports was added to give a total that reflects the quality of the same, according to the established standard. We thereby classified the reports into 4 categories (Table 2).
For the final objective of the study the sample was characterised according to the distribution of the descriptive variables by showing their core tendency (average, median and mode) and their absolute and relative frequencies were calculated. The Excel program (Microsoft Office® version 2013) was used to label and screen the database arising from tabulation of the recorded data and subsequent statistical analysis using the available valid data.
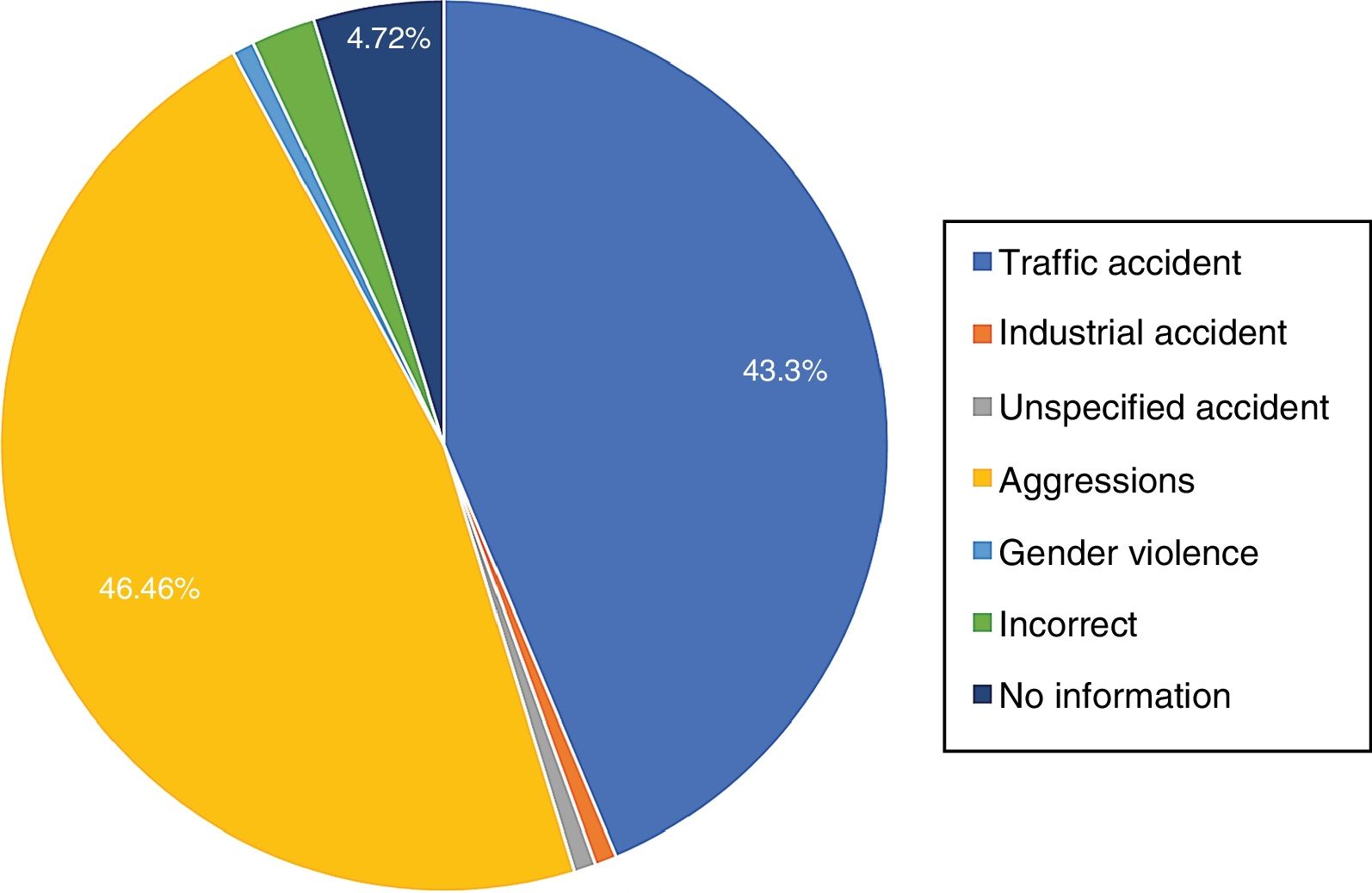
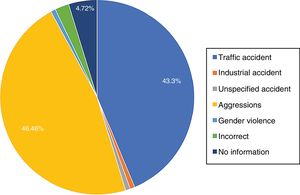
ResultsOf the 127 reports analysed, 55 were issued after traffic accidents (43.3%), one was issued after an industrial accident (0.79%) and one after an accident with an unspecified cause (0.79%). A total of 59 reports were issued after aggressions (46.46%) and one was issued for gender-based violence (0.79%). 3 must be added which were not filled out properly under the heading of “alleged cause” (2.3%) and there were 6 reports in which this was not included (4.72%) (Fig. 1).
These figures do not correspond with the actual proportion of reports received by the Legal Medicine and Forensic Science Institute, as we have to remember that one of the inclusion criteria was the presence of visually detectable injuries, while many of the reports consulted that were issued due to traffic accidents did not fulfil this requisite.
Once the quality scale had been applied the total average score obtained by the injury reports studied amounted to 58.54 points, taking the maximum score of 90 as the reference. In this way, 2 reports (1.6%) were classified within the range defined as “very poor quality”, 21 (16.5%) were “low quality”, 100 (78.7%) were “intermediate quality”, and only 4 could be considered “high quality” (3.2%). The highest score found was 75 points (Fig. 2).
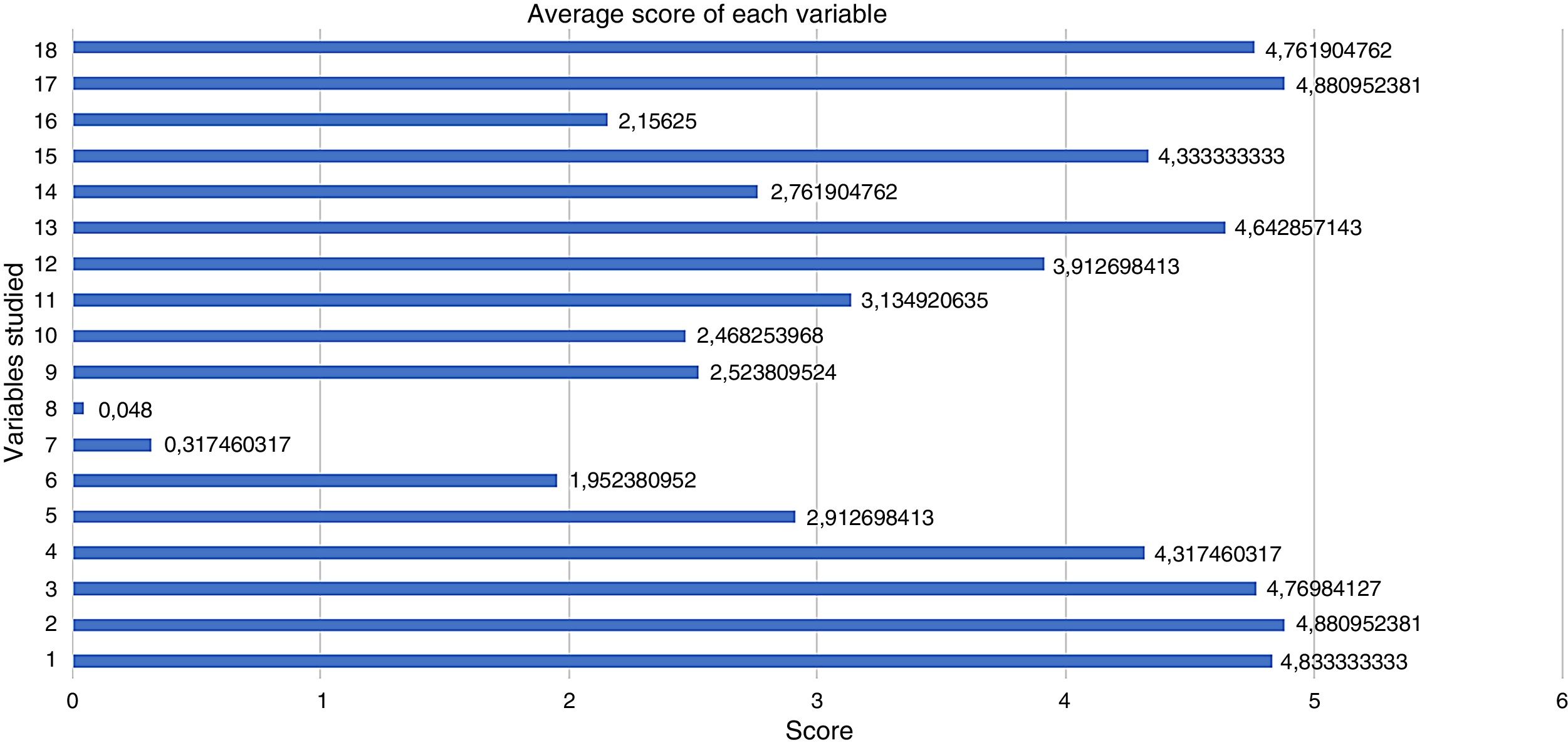
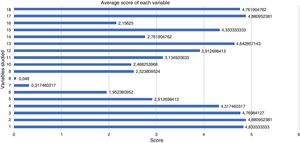
On the other hand, Fig. 3 shows the data obtained from individual analysis of each variable. The differences in scores depending on the type of each variable are very clear here. For example, the data corresponding to the hospital, the treating doctors and the injured individual attain very high scores close to 5, while those for the description of the injury and above all correct identification of the same, its size and evolution, obtain extremely low scores.
Average score of each variable studied, where 5 is the maximum score and 0 is the minimum score. 1: hospital data; 2: doctor identification data; 3: personal data of the injured party; 4: alleged cause; 5: location of the injury; 6: type; 7: size; 8: state of evolution; 9: psychological and emotional state of the victim; 10: additional tests; 11: therapeutic measures; 12: action plan; 13: clinical prognosis; 14: description of the facts; 15: date and time of treatment; 16: data of the supposed aggressor; 17: clear and legible writing; 18: the presence of corrections.
Few studies now exist of the quality of the injury reports issued by Primary Care and Accident and Emergency Departments.10–12 This situation is aggravated by the fact that this procedure is not subject to international regulation and that, even within Spain, we found that Regional norms differed widely from one autonomous community to another. Nor are there any uniform models for the said document.13 The fact is that only the Autonomous Community of Andalusia has a specific and complete regulation of this subject, by means of Decree 3/2011, of 11 January, which created a uniform and normalised model of the report to courts, and it also established the applicable regulations and instructions for filling out and processing these reports.14
In spite of this lack of regulation, all of the studies and bibliography consulted agree unanimously that injury reports are highly important when forensic doctors prepare assessment reports and, lastly, in the determination of the importance of injuries by judges, which directly affects their civil and penal consequences.15,16 This is because in the majority of cases the medical-forensic examination takes place some time after the injuries were caused, so that it is possible that none of them will be detectable.10,17 Additionally, we should remember that, according to article 147 of the Penal Code, the severity of injuries and, due to the same, compensation for the damage caused, largely depends on the therapeutic measures applied and the clinical prognosis. These data are highly valuable and must be shown in the report.9,18
Nevertheless, experience in the everyday work of forensic doctors together with some studies of this subject11,12 show that, in spite of their importance, the injury reports issued by doctors lack the quality that could be desired. The results obtained in this study support this widespread impression, offering objective data that show the low quality of how these documents are prepared and the most common faults committed during their preparation.
When the quality scale designed for this work was applied the average score was 58.54 points, and the majority of reports (78.7%) were classified as “intermediate quality”. Nevertheless, the majority of these intermediate quality reports are highly defective in the sections on the description of injuries (their location, type, size and evolution). The size and evolution of injuries obtained the lowest scores, with average scores of 0.32 and 0.048, respectively. The average score for the strictly medical–legal items (variables 5–13 in Fig. 3) stands at 2.43, as opposed to the average of 4.19 obtained by the other variables. The average score of 58.54 points was therefore obtained due to compensation of these low scores by the higher scoring variables, fundamentally the hospital data and personal data of the doctor and patient, together with the alleged cause, which are often filled out by secretarial staff. 2 other variables also contributed, these being numbers 17 and 18 (corrections and legible writing), which given that the vast majority of reports were in electronic format explains high scores in these respects.
Nor is much attention paid to describing the psychological and emotional state of the victim, narrating the events that took place and the data of the supposed aggressor, in cases of aggression. Likewise, the scores in the sections on the severity of the injury are alarming, i.e., on whether additional tests have been requested or not, and if so of what type, together with the treatment applied and the action plan. It must be remembered that to determine the medical–legal prognosis it is fundamental to know, apart from the nature of the injuries, the treatment given and the therapeutic prescriptions necessary to cure them. On the other hand, although the section on the clinical prognosis, classifying it as slight to very severe, is almost always included, striking differences were found in the criteria used by different professionals. There is a need for more objective and uniform criteria that would add to the validity of this information. Thus a range of injuries were considered to be “moderate” even though they ran from a marginal non-displaced fracture of the patella, bruising and sprain of the left ankle, dental extraction or a cervical contraction, while fracture of own bones was classified as “slight”.
All of these findings agree with those of similar studies found in the bibliography. The majority of these studies conclude that a high percentage of reports are poorly filled in, while a great many of them lack data which are considered to be necessary.11,13,19 Traffic accidents predominated In some previous studies,10,11 while in ours aggressions were in first place (46.46% of cases), closely followed by traffic accidents (43.3%). This fact may be due in one case to differences in the population analysed (as it was paediatric),10 or because one of the inclusion criteria in our work was the presence of visually detectable injuries, and many reports issued due to traffic accidents do not fulfil this requisite. They agree with our findings in that they often find deficiencies in the completion of sections on the cause or prognosis of injuries. Special mention must be made of gender violence, for which a specific standard model of injury report is usually available in hospitals. García-Minguito et al.12 analysed how 700 injury reports were filled out in cases of gender violence using a scale based on 10 criteria. Their results were similar to ours, with an average score of 78.1 points which would correspond to intermediate quality. They also detected deficiencies, especially in the content of injury descriptions and the lack of a report on psychological state, among other aspects. Our sample only included one report on gender violence, although together with observations in other works it does not seem that this improves the quality of the document, in spite of how important it is in the legal approach to this problem.12,20
The main deficiencies found during our analysis were the presence of hardly legible writing in those documents which had been completed by hand. Although these are now in the minority they still form a relevant percentage of incomplete reports, which do not contain all of the information that is required, with no description of injuries or an unsuitable form of the same using terms that are vague or inappropriate, such as bruises, multiple contusions, red patches, swellings or bite wounds, as well as numerous errors in connection with the treatment given (medical treatment and observation, radiology, analgesia, disinfection and cleaning). Many of these problems have been resolved in the majority of autonomous communities, as they have standardised and computerised models which aid their completion, preventing difficulties arising due to illegible writing and slightly reducing the number of incomplete reports; this is especially so in Andalusia, where this matter is regulated.14 In spite of this, we still detect a high prevalence of the other problems described, and this leads us to consider where they arise in order to find an appropriate solution. We believe that new studies will be necessary to discover whether the origin of these problems lies in a lack of knowledge of legal matters, a lack of time during clinical care, insufficient awareness of the importance of this subject, lack of medical involvement or a specific deficit in Legal Medicine training.
Thus definitively, this study firstly contributes by establishing a scale which, after validation, will make it possible to evaluate the quality of injury reports. Secondly, it contributes by showing that this important medical–legal document is poorly completed, based on analysis of a sample of 127 reports.
Given the importance of injury reports, as they are the sole objective record of the initial medical treatment which largely forms the basis for subsequent actions by the forensic doctor, Ministry of Justice and the judge, all doctors should know when and how to complete them correctly. In the light of the above findings a strategy is required to improve how these medical–legal documents are filled out, most especially in the sections that cover the description of the injury, the treatment given and the prognosis.
Study limitationsGiven the specific geographical location of the sample studied (injury reports in the province of Córdoba), and in spite of the fact that the results are comparable with those of other similar studies, the conclusions obtained cannot be extrapolated to how these documents are filled out in other Primary Care and Accident and Emergency departments.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Linares-González L, Sáez Rodríguez J, Beltrán-Aroca CM, Girela-López E. Control de calidad de los partes de lesiones emitidos en Atención Primaria y Urgencias de la provincia de Córdoba. Rev Esp Med Legal. 2019;45:12–17.