The objective of this work is to perform a bibliographic review of the literature on sports-related sudden cardiac death (SR-SCD), including competitive and recreational athletes of all ages. A comprehensive literature search was performed in PubMed and SCOPUS, including articles containing relevant information on the epidemiology of SR-SCD or its preventive strategies. The use of different methodologies has led to heterogeneous results. Most authors conclude that the incidence of SR-SCD is very low, sport should not be feared. Preparticipation cardiovascular screening and dissemination of automatic external defibrillators (AED) are used to prevent SR-SCD. Both are complementary and indispensable. Preparticipation screening should include competitive and recreational athletes. A multidisciplinary approach, standardized research protocols and the inclusion of all cases are essential for a better understanding of SR-SCD.
El objetivo de este trabajo es realizar una revisión bibliográfica de la literatura sobre muerte súbita cardiaca en relación con el deporte (SR-SCD), incluyendo deportistas de competición y recreacionales de todas las edades. Se ha hecho una búsqueda comprensiva en PubMed y SCOPUS, incluyendo artículos con información relevante acerca la epidemiologia y estrategias preventivas de SR-SCD. El uso de distintas metodologías ha generado resultados heterogéneos. La mayoría de autores concluyen que la incidencia es muy baja: hacer deporte es seguro. Como estrategias para prevenir SR-SCD se aconseja hacer una revisión médica preparticipación y la diseminación de desfibriladores externos automáticos (AED). Ambas son complementarias e indispensables. La revisión médica debería incluir tanto deportistas de competición como recreativos. Un abordaje multidisciplinario, la estandarización de la investigación y la inclusión de todos los casos son esenciales para entender mejor la SR-SCD.
Cardiovascular diseases are the most frequent cause of death in industrialized countries.1 Within these, sports-related sudden cardiac death (SR-SCD), particularly among high profile athletes, has gained huge attention, attracting substantial public interest in the media and in cardiovascular medicine.2 How can it be that those considered to be the healthiest of the community die suddenly and unexpectedly?
More than 500 papers have been published in the last 5 years, but despite all these efforts, our understanding of the precise epidemiology and circumstances surrounding SR-SCD remains very limited.3 Therefore, there are huge controversies such as different cardiovascular preparticipation screening strategies for athletes from the European Society of Cardiology (ESC) and the American Heart Association (AHA).4,5 Noticeably, these controversies have a global influence in community health planning models.6,7
Many methodological obstacles must be considered when investigating the epidemiology of SR-SCD. One of the most important, is the fact is that most observational reports have not followed a uniform protocol: different inclusion criteria, diverse definitions and characterization of the athletic population and non-uniform methodology in autopsies.3,8 This makes it very difficult to compare different data sets; therefore, high quality meta-analyses are largely unachievable at the present time.
This review aims to perform a bibliographic review of the literature on SR-SCD, with the purpose to evaluate the state of art. More concretely the objectives are:
- 1.
To determine the incidence of SR-SCD in competitive and recreational athletes and compare it to the incidence of SCD in the general population.
- 2.
To establish the causes and circumstances of SR-SCD.
- 3.
To analyze the actual preventive strategies of SR-SCD, including preparticipation cardiovascular screening and public dissemination of automatic external defibrillators (AED).
A comprehensive literature search was performed in PubMed and SCOPUS using: (“sudden cardiac death” or “sudden cardiac arrest”) and (athlete* or “recreational athletes”) and (sport or sports) and (epidemiology or etiology or prevent* or statistic* or “numerical data”), filtering the results between 2013 and 2017. Articles were reviewed for relevance and included if they contained epidemiologic and preventive information on SR-SCD, from both recreational and competitive athletes of all ages. The reference list from each paper was also reviewed for additional relevant articles, amplifying the search up to 2003. Several systematic reviews have been very useful in the production of this paper.2,3,9,10
ResultsThe search resulted in 88 articles in PubMed and 105 in SCOPUS. A total of 50 papers have been included to perform this study. As previously mentioned, articles were selected according to their content in epidemiologic and preventive data.
DefinitionsThere is a lack of consensus with the concepts of sudden cardiac death/arrest, sports-related death or the characterization of the athletic population. We will present some definitions, showing the main controversies found in the literature.
Sudden cardiac death (SCD): Unexpected rapid natural death due to cardiovascular collapse within 1h of initial symptoms. It is usually caused by the worsening of existing heart diseases. The sudden onset of symptoms, such as chest pain and cardiac arrhythmias, particularly ventricular tachycardia, can lead to the loss of consciousness and cardiac arrest followed by biological death. Despite most authors consider <1h in witnessed cases and <24h in unwitnessed cases there is not a clear consensus about the time between the origin of symptoms and death.8,11–13
SCD and sudden cardiac arrest (SCA) are equivalent entry terms in a PubMed MeSH search. However, they are not always used as analogous, having small but crucial differences, which have an important impact in the interpretation of studies on the field. In this way, SCA is sometimes defined as a condition in which the heart suddenly and unexpectedly stops beating. It does not necessarily imply biological death and sometimes authors do not provide data on how many cases are successfully resuscitated.9,10
Sports-related SCD (SR-SCD): SCD that occurs during sport or in close conjunction with sporting activity.14 The time-lapse between sport activity and the onset of symptoms and death is again debated and not well established. The proportion of all deaths defined as SCD is 13% when a definition of 1h from onset of symptoms is used, whereas the proportion rises to 19% when a 24h time-frame is used.3 The issue is even more complicated, since there are reports of SCA happening during sport, with death occurring several days afterwards.15 What is more, some articles do not use a time-frame, they consider a death as SR-SCD if it happens to someone classified as an athlete.16 Therefore, the diverse definitions of SR-SCD impact largely on the epidemiological and incidence data and show different realities of the same problem.
Competitive athletes vs recreational athletes: the 16th Bethesda Conference defines a competitive athlete as an individual who participates in an organized team or in a sport that requires regular competition against others, places a high premium on excellence and achievement, and requires some form of systematic and intense training.17
Recreational athletes are defined as individual that have the ability and freedom to judge when it is prudent to reduce or stop physical exertion.18 They can also be defined as individuals engaged in recreational or leisure-time sports activities, on either a regular basis or intermittently.3
Epidemiology of SR-SCDMost of the research on SR-SCD has been conducted in young competitive athletes, because it was believed that they were in higher risk.4 In this way, most articles focus on athletes younger than 35 years of age, which they define as “young athletes”. A much smaller proportion of studies target athletes older than 35, traditionally defined as “older athletes”. Finally, some target the epidemiology of SR-SCD in the general population of athletes of all groups (competitive and recreational) and ages.
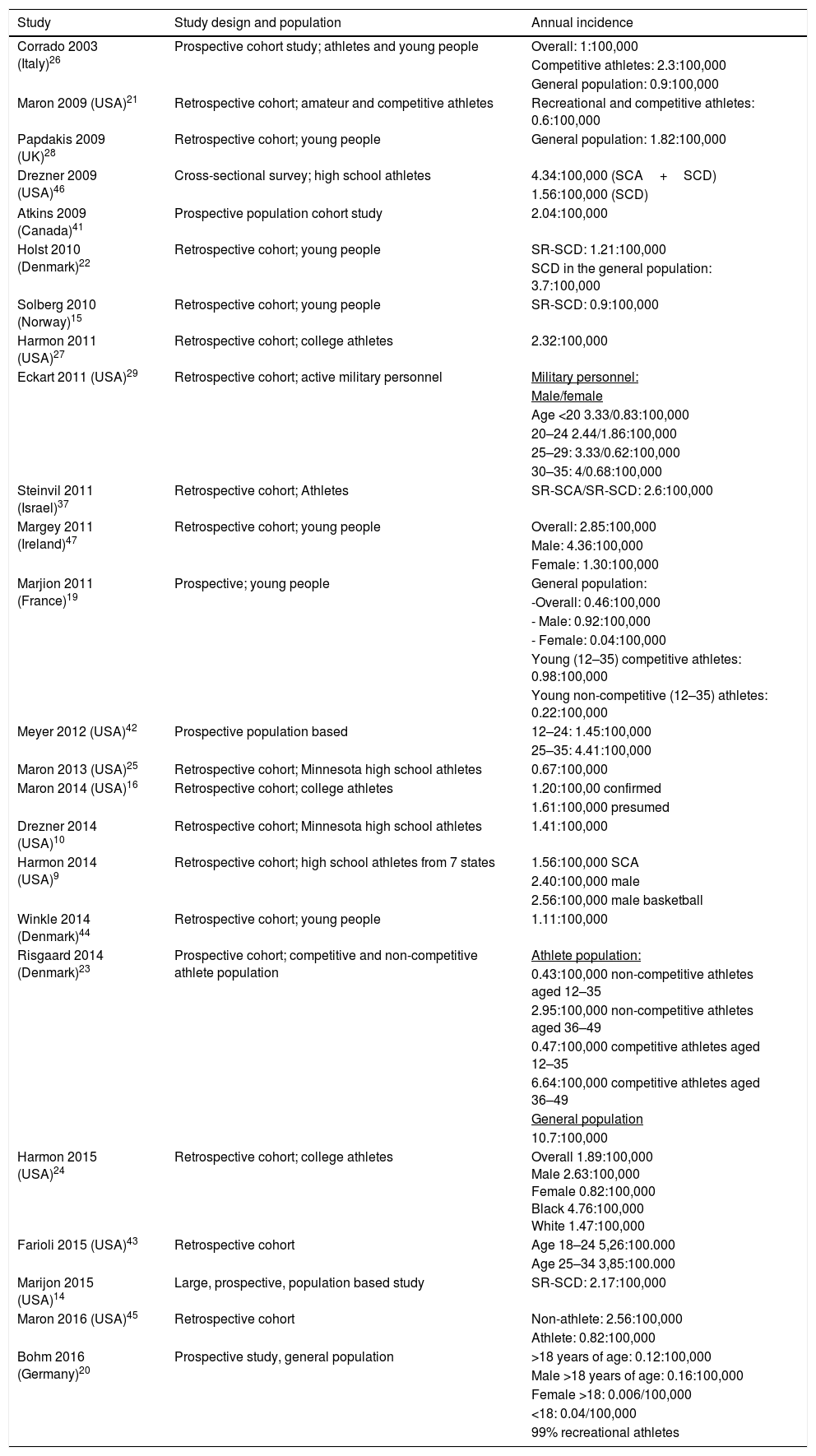
Table 1 summarizes the epidemiological results of 24 observational studies between 2003 and 2016. Only studies that calculate the incidence of SCD or SR-SCD in different populations have been included: in the general population, in competitive and recreational athletes and in subgroups such as male/female or young/older athlete, elite athletes and other.
Epidemiological summary of 24 observational studies in SR-SCD between 2003 and 2016.
| Study | Study design and population | Annual incidence |
|---|---|---|
| Corrado 2003 (Italy)26 | Prospective cohort study; athletes and young people | Overall: 1:100,000 |
| Competitive athletes: 2.3:100,000 | ||
| General population: 0.9:100,000 | ||
| Maron 2009 (USA)21 | Retrospective cohort; amateur and competitive athletes | Recreational and competitive athletes: 0.6:100,000 |
| Papdakis 2009 (UK)28 | Retrospective cohort; young people | General population: 1.82:100,000 |
| Drezner 2009 (USA)46 | Cross-sectional survey; high school athletes | 4.34:100,000 (SCA+SCD) |
| 1.56:100,000 (SCD) | ||
| Atkins 2009 (Canada)41 | Prospective population cohort study | 2.04:100,000 |
| Holst 2010 (Denmark)22 | Retrospective cohort; young people | SR-SCD: 1.21:100,000 |
| SCD in the general population: 3.7:100,000 | ||
| Solberg 2010 (Norway)15 | Retrospective cohort; young people | SR-SCD: 0.9:100,000 |
| Harmon 2011 (USA)27 | Retrospective cohort; college athletes | 2.32:100,000 |
| Eckart 2011 (USA)29 | Retrospective cohort; active military personnel | Military personnel: |
| Male/female | ||
| Age <20 3.33/0.83:100,000 | ||
| 20–24 2.44/1.86:100,000 | ||
| 25–29: 3.33/0.62:100,000 | ||
| 30–35: 4/0.68:100,000 | ||
| Steinvil 2011 (Israel)37 | Retrospective cohort; Athletes | SR-SCA/SR-SCD: 2.6:100,000 |
| Margey 2011 (Ireland)47 | Retrospective cohort; young people | Overall: 2.85:100,000 |
| Male: 4.36:100,000 | ||
| Female: 1.30:100,000 | ||
| Marjion 2011 (France)19 | Prospective; young people | General population: |
| -Overall: 0.46:100,000 | ||
| - Male: 0.92:100,000 | ||
| - Female: 0.04:100,000 | ||
| Young (12–35) competitive athletes: 0.98:100,000 | ||
| Young non-competitive (12–35) athletes: 0.22:100,000 | ||
| Meyer 2012 (USA)42 | Prospective population based | 12–24: 1.45:100,000 |
| 25–35: 4.41:100,000 | ||
| Maron 2013 (USA)25 | Retrospective cohort; Minnesota high school athletes | 0.67:100,000 |
| Maron 2014 (USA)16 | Retrospective cohort; college athletes | 1.20:100,00 confirmed |
| 1.61:100,000 presumed | ||
| Drezner 2014 (USA)10 | Retrospective cohort; Minnesota high school athletes | 1.41:100,000 |
| Harmon 2014 (USA)9 | Retrospective cohort; high school athletes from 7 states | 1.56:100,000 SCA |
| 2.40:100,000 male | ||
| 2.56:100,000 male basketball | ||
| Winkle 2014 (Denmark)44 | Retrospective cohort; young people | 1.11:100,000 |
| Risgaard 2014 (Denmark)23 | Prospective cohort; competitive and non-competitive athlete population | Athlete population: |
| 0.43:100,000 non-competitive athletes aged 12–35 | ||
| 2.95:100,000 non-competitive athletes aged 36–49 | ||
| 0.47:100,000 competitive athletes aged 12–35 | ||
| 6.64:100,000 competitive athletes aged 36–49 | ||
| General population | ||
| 10.7:100,000 | ||
| Harmon 2015 (USA)24 | Retrospective cohort; college athletes | Overall 1.89:100,000 Male 2.63:100,000 Female 0.82:100,000 Black 4.76:100,000 White 1.47:100,000 |
| Farioli 2015 (USA)43 | Retrospective cohort | Age 18–24 5,26:100.000 |
| Age 25–34 3,85:100.000 | ||
| Marijon 2015 (USA)14 | Large, prospective, population based study | SR-SCD: 2.17:100,000 |
| Maron 2016 (USA)45 | Retrospective cohort | Non-athlete: 2.56:100,000 |
| Athlete: 0.82:100,000 | ||
| Bohm 2016 (Germany)20 | Prospective study, general population | >18 years of age: 0.12:100,000 |
| Male >18 years of age: 0.16:100,000 | ||
| Female >18: 0.006/100,000 | ||
| <18: 0.04/100,000 | ||
| 99% recreational athletes |
According to the Heart Disease and Stroke Statistics 2016 the incidence of SCD in the general population is 69:100,000 per year.1 Concerning SR-SCD in the general population of athletes, including competitive and recreational athletes, the incidence for all age groups (12–80 years of age) ranges from 0.12 to 0.46:100,000.19,20 Among young athletes, it ranges from 0.45 to 1.21:100,000.15,21–23 Marijon et al.14 and Risgaard et al.23 present an incidence of 2.17–2.95:100,000 athletes/year for older recreational athletes. The last author, also presents an incidence of 6.64:100,000 for old competitive athletes.
One of the most important and prolific lines of investigation has been conducted in American high school and college athletes, although the results are interesting and the methodologies are more consistent, they are based in a very specific subgroup of younger population. These studies set the annual incidence in approximately 1.25:100,000 in high school athletes and 2:100,000 in college athletes respectively.10,16,21,24,25 Other studies in young competitive athletes range from 0.98–2.3:100,000 athletes/year.19,23,26 In young recreational athletes, the incidence is 0.22–2.33:100,000.19,23
Finally, the athlete's gender and ethnicity may also influence the incidence of both SR and non-SR SCD. According to gender, there has traditionally been a strong male predisposition with ratios 10:1 amongst competitive athletes19,25,27 and up to 20:1 in the general exercising population.19 Regarding ethnicity, black athletes appear to have a higher incidence of SCD compared with Caucasian athletes.16 Black US college athletes had a considerably (about 3–5) times risk of SCD compared to white athletes.16,27
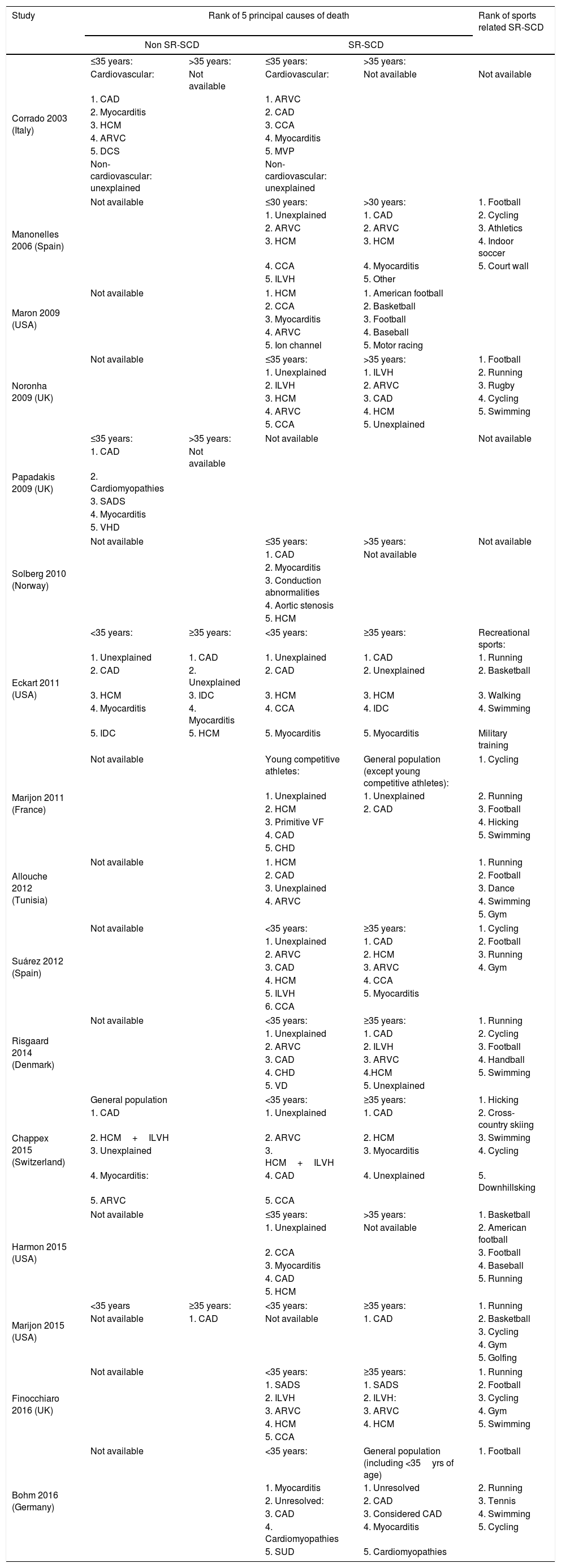
Causes and circumstances of SR-SCDTable 2 shows the results of 16 studies between 2003 and 2016 with the causes and circumstances of death in the general population and in different subgroups of athletic populations.
Causes and circumstances of death in the general population and in the different subgroups of SR-SCD.
| Study | Rank of 5 principal causes of death | Rank of sports related SR-SCD | |||
|---|---|---|---|---|---|
| Non SR-SCD | SR-SCD | ||||
| Corrado 2003 (Italy) | ≤35 years: | >35 years: | ≤35 years: | >35 years: | |
| Cardiovascular: | Not available | Cardiovascular: | Not available | Not available | |
| 1. CAD | 1. ARVC | ||||
| 2. Myocarditis | 2. CAD | ||||
| 3. HCM | 3. CCA | ||||
| 4. ARVC | 4. Myocarditis | ||||
| 5. DCS | 5. MVP | ||||
| Non-cardiovascular: unexplained | Non-cardiovascular: unexplained | ||||
| Manonelles 2006 (Spain) | Not available | ≤30 years: | >30 years: | 1. Football | |
| 1. Unexplained | 1. CAD | 2. Cycling | |||
| 2. ARVC | 2. ARVC | 3. Athletics | |||
| 3. HCM | 3. HCM | 4. Indoor soccer | |||
| 4. CCA | 4. Myocarditis | 5. Court wall | |||
| 5. ILVH | 5. Other | ||||
| Maron 2009 (USA) | Not available | 1. HCM | 1. American football | ||
| 2. CCA | 2. Basketball | ||||
| 3. Myocarditis | 3. Football | ||||
| 4. ARVC | 4. Baseball | ||||
| 5. Ion channel | 5. Motor racing | ||||
| Noronha 2009 (UK) | Not available | ≤35 years: | >35 years: | 1. Football | |
| 1. Unexplained | 1. ILVH | 2. Running | |||
| 2. ILVH | 2. ARVC | 3. Rugby | |||
| 3. HCM | 3. CAD | 4. Cycling | |||
| 4. ARVC | 4. HCM | 5. Swimming | |||
| 5. CCA | 5. Unexplained | ||||
| Papadakis 2009 (UK) | ≤35 years: | >35 years: | Not available | Not available | |
| 1. CAD | Not available | ||||
| 2. Cardiomyopathies | |||||
| 3. SADS | |||||
| 4. Myocarditis | |||||
| 5. VHD | |||||
| Solberg 2010 (Norway) | Not available | ≤35 years: | >35 years: | Not available | |
| 1. CAD | Not available | ||||
| 2. Myocarditis | |||||
| 3. Conduction abnormalities | |||||
| 4. Aortic stenosis | |||||
| 5. HCM | |||||
| Eckart 2011 (USA) | <35 years: | ≥35 years: | <35 years: | ≥35 years: | Recreational sports: |
| 1. Unexplained | 1. CAD | 1. Unexplained | 1. CAD | 1. Running | |
| 2. CAD | 2. Unexplained | 2. CAD | 2. Unexplained | 2. Basketball | |
| 3. HCM | 3. IDC | 3. HCM | 3. HCM | 3. Walking | |
| 4. Myocarditis | 4. Myocarditis | 4. CCA | 4. IDC | 4. Swimming | |
| 5. IDC | 5. HCM | 5. Myocarditis | 5. Myocarditis | Military training | |
| Marijon 2011 (France) | Not available | Young competitive athletes: | General population (except young competitive athletes): | 1. Cycling | |
| 1. Unexplained | 1. Unexplained | 2. Running | |||
| 2. HCM | 2. CAD | 3. Football | |||
| 3. Primitive VF | 4. Hicking | ||||
| 4. CAD | 5. Swimming | ||||
| 5. CHD | |||||
| Allouche 2012 (Tunisia) | Not available | 1. HCM | 1. Running | ||
| 2. CAD | 2. Football | ||||
| 3. Unexplained | 3. Dance | ||||
| 4. ARVC | 4. Swimming | ||||
| 5. Gym | |||||
| Suárez 2012 (Spain) | Not available | <35 years: | ≥35 years: | 1. Cycling | |
| 1. Unexplained | 1. CAD | 2. Football | |||
| 2. ARVC | 2. HCM | 3. Running | |||
| 3. CAD | 3. ARVC | 4. Gym | |||
| 4. HCM | 4. CCA | ||||
| 5. ILVH | 5. Myocarditis | ||||
| 6. CCA | |||||
| Risgaard 2014 (Denmark) | Not available | <35 years: | ≥35 years: | 1. Running | |
| 1. Unexplained | 1. CAD | 2. Cycling | |||
| 2. ARVC | 2. ILVH | 3. Football | |||
| 3. CAD | 3. ARVC | 4. Handball | |||
| 4. CHD | 4.HCM | 5. Swimming | |||
| 5. VD | 5. Unexplained | ||||
| Chappex 2015 (Switzerland) | General population | <35 years: | ≥35 years: | 1. Hicking | |
| 1. CAD | 1. Unexplained | 1. CAD | 2. Cross-country skiing | ||
| 2. HCM+ILVH | 2. ARVC | 2. HCM | 3. Swimming | ||
| 3. Unexplained | 3. HCM+ILVH | 3. Myocarditis | 4. Cycling | ||
| 4. Myocarditis: | 4. CAD | 4. Unexplained | 5. Downhillsking | ||
| 5. ARVC | 5. CCA | ||||
| Harmon 2015 (USA) | Not available | ≤35 years: | >35 years: | 1. Basketball | |
| 1. Unexplained | Not available | 2. American football | |||
| 2. CCA | 3. Football | ||||
| 3. Myocarditis | 4. Baseball | ||||
| 4. CAD | 5. Running | ||||
| 5. HCM | |||||
| Marijon 2015 (USA) | <35 years | ≥35 years: | <35 years: | ≥35 years: | 1. Running |
| Not available | 1. CAD | Not available | 1. CAD | 2. Basketball | |
| 3. Cycling | |||||
| 4. Gym | |||||
| 5. Golfing | |||||
| Finocchiaro 2016 (UK) | Not available | <35 years: | ≥35 years: | 1. Running | |
| 1. SADS | 1. SADS | 2. Football | |||
| 2. ILVH | 2. ILVH: | 3. Cycling | |||
| 3. ARVC | 3. ARVC | 4. Gym | |||
| 4. HCM | 4. HCM | 5. Swimming | |||
| 5. CCA | |||||
| Bohm 2016 (Germany) | Not available | <35 years: | General population (including <35yrs of age) | 1. Football | |
| 1. Myocarditis | 1. Unresolved | 2. Running | |||
| 2. Unresolved: | 2. CAD | 3. Tennis | |||
| 3. CAD | 3. Considered CAD | 4. Swimming | |||
| 4. Cardiomyopathies | 4. Myocarditis | 5. Cycling | |||
| 5. SUD | 5. Cardiomyopathies | ||||
Arrhythmogenic right ventricular cardiomyopathy (ARVC), congenital heart disease (CHD), congenital coronary arteries anomalies (CCA), coronary artery disease (CAD), disease conduction system (DCS), hypertrophic cardiomyopathy (HMC), idiopathic dilated cardiomyopathy (IDC), idiopathic left ventricular hypertrophy (ILVH), mitral valve prolapse (MVP), sudden unexpected death (SUD), sudden arrhythmic death syndrome (SADS), valve disease (VD), valvular heart disease (VHD).
The most frequent cause of SCD in the general population of all age groups is coronary artery disease (CAD).14,26,28–30 CAD is also the most frequent cause of death in the older athlete (>35).23,29–32
As observed in many scientific reports, the most frequent cause of SR-SCD among young athletes (<35) is “unexplained death” or “blanche autopsy” in which a morphologically normal heart is found in the autopsy.19,23,24,29–34 These studies usually classify these deaths as cardiac, being produced by lethal arrhythmias. The most recent studies have introduced the term sudden arrhythmic death syndrome (SADS) to define this cause of death.34 The relative frequency of the other most frequent causes of death in the young athlete are not clear and they vary from one study to another and depending on the population studied. Arrhythmogenic right ventricular cardiomyopathy (ARVC), idiopathic left ventricular hypertrophy (ILVH), hypertrophic cardiomyopathy (HCM), channelopathies and congenital coronary arteries anomalies (CCA) seem to be the most frequent autopsy results.23,26,30–32,34 CCA are the most frequent cause of SR-SCD among teenagers.34
When we analyze the circumstances surrounding the death, such as which sport is being practiced. Football, basketball, American football, cycling, swimming and running21,26,31,33 are the sports that most frequently appear in the studies’ results. The relative frequency of each sport associated with SR-SCD also varies between studies, nevertheless there is always a clear cultural influence and the most commonly practiced sports of a nation are usually associated with more cases.
Preparticipation cardiovascular screeningThe American Heart Association (AHA) and the European Society of Cardiology (ESC) advocate for the screening of competitive athletes. However, they strategies differ. The AHA recommends screening with medical history and physical examination only,5 whereas the ESC recommends the addition of a 12-lead-ECG.4 The American model is cheap and pragmatic but has poor sensitivity, with values as low as 6%.2 In a meta-analysis, an ECG was 5 times more sensitive than history,10 times more sensitive than physical examination and had a higher positive likelihood ratio, a lower negative likelihood ratio and a lower false positive rate.35
The ECG is more effective in detecting disease,2 however there is debate regarding whether early diagnosis equates to a life saved. Corrado et al. is the best evidence that screening can save lives, whereas Steinvil et al. showed no difference in the prevalence of SR-SCD before and after screening strategies were implemented.36,37
Secondary prevention with AEDActual application of public-access AED to patients with a SR-SCD has been poorly investigated. Largely because dissemination of public-access AED and legalization of non-medical persons use of AED is still something very recent and happening only in very few places.38 The studies published tend to conclude that the application of public-access AED leads to favorable outcomes.39,40 Several studies show that training the general population in Cardiopulmonary Resuscitation (CPR) and Defibrillation is essential to improve survival.38,39
DiscussionEpidemiology of SR-SCDThe epidemiological results of SR-SCD are enormously disperse, therefore it is difficult to know with exactitude the real incidence and public health importance of SR-SCD. This dispersity of results is due to the different methodological approaches used in studies. For example, data collection can be derived from either prospective19,26,41,42 or retrospective registries,43–45 voluntary reporting46 or even from media reports.37 Identifying the cause of death is another differential factor between studies, some studies just include autopsied cases,15,47 while others include non-autopsied cases,19,25 or worse still, some obtain the results from newspapers.37 To calculate the annual incidence of SR-SCD some authors use resuscitated cases,19,42 while others not.15,23 Surprisingly, even systematic reviews show different results for the same article.9,10
Therefore, instead of traying to analyze the exact numbers of studies this work focus on the conclusions they have reached. Almost all authors conclude that regular physical activity has health benefits, including an increase in life-expectancy. There is also consensus that vigorous and competitive physical exercise may be associated with a small risk of SCD. Nevertheless, most of the revised studies conclude that the incidence of SCD in the general population is higher than in athletes and that incidence rates in competitive and recreational athletes do not differ. What is also clear is that the risk of SR-SCD is much higher in older athletes, being the age of 35 the cut-off point. Significantly, authors usually conclude that SR-SCD is not a very important public health issue, because the prevalence and incidence is low compared to other causes of death.
The prevalence of SR-SCD is higher in men than in women. Some authors justify it saying that the participation and intensity of physical activities is higher in men than in women.31,48 However, the incidence is also much higher in men than in women and the reason is not yet completely understood.
Some studies show that black athletes are at higher risk of SR-SCD. Nevertheless, the term “black” can be ambiguous because it comprises different populations (Afro-American, Caribbean, Eastern and Western Africans, etc.). The issue of race is even more complicated as there is a growing number of individuals who are of mixed ethnicity.3
Causes and circumstances of SR-SCD: victim's profileFrom a clinical perspective, it would be interesting to know who is at higher risk of SR-SCD. There is a general consensus that the most common victims profile would be that of a man, over 35 years of age with cardiovascular risk factors doing recreational sports, such as running or cycling. The cause of death would be CAD.
The other typical victims profile, although representing a much smaller group, would be that of a young recreational or competitive athlete, dying of SADS, ILVH, HCM or ARVC. However, we would like to stress that the risk of SCD and SR-SCD in the young individuals is extremely low and that they should not fear the practice of sport.
A relatively high number of the victims of SR-SCD have had previous symptoms or have family antecedents making it very important to raise awareness about of the need to consult a doctor in these cases. But also, SR-SCD too often appears as the first manifestation of the disease specially in young athletes.14
Preparticipation cardiovascular screeningPreparticipation screening aims to identify those affected by cardiovascular diseases who may be at higher risk of SCD during sports participation.49 There is a lot of debate concerning preparticipation cardiovascular screening because, as already stated the public health impact of SR-SCD is not well understood. Moreover, there are conflicting recommendations from the AHA and ESC.
The results of this study show that there are two tendencies. First, some authors defend that preparticipation screening is not necessary because the incidence of SR-SCD is very low and specially because it is significantly lower than the risk of SCD in the general population.22,23 Second, most of the authors and scientific societies influenced by the dramatic reality of SR-SCD in young individuals are more conservative and recommend screening of young competitive athletes.2,4,5
Something remarkable is that the actual screening strategies of the AHA and ESC focus only on competitive athletes and ignore the much larger group of recreational athletes, who collectively represent a population in which a much larger number of SCD can be predicted to occur. Several authors suggest that if preparticipation screening should include all athletes, especially those older than 35.14,23,30 The ESC, AHA and American College of Sports Medicine (ACSM) have addressed this issue and introduced some recommendations for older athletes, focusing especially on the detection of CAD. However, this strategy has not been rigorously evaluated.50 Moreover, there are no recommendations for young recreational athletes. Although, the incidence in this group does not differ from young competitive-athletes.
All of this aside, the screening process is expensive. Data suggest that 33,000 athletes should be screened to save 1 life at a cost per life saved of $10.5 million in USA and $1,320,000 in Italy. In this way, universal screening poses logistic and financial challenges and only two countries in the world (Italy and Israel) practice state sponsored screening of competitive athletes.2,49
Therefore, any recommended preparticipation screening program should have an appropriate balance between the lives saved, the number of athletes tested, the associated psychological, ethical and legal issues of false-positive results and the cost.3
Secondary prevention with AEDThe cost of public dissemination of AED is enormous. There is considerable debate toward which is the best cost-benefit strategy to improve SR-SCD survival. There are very few articles published about secondary prevention of SR-SCD with AED. What is clear is that training athletes, trainers, etc. in CPR and AED use and placing AED in areas were sports are practiced can save lives.19
What is more cost-effective, preparticipation cardiovascular screening or training in CPR and public distribution of AED? One complements the other for, no screening program provides absolute protection against SCD and access to AED is essential to improve outcomes from SCA in athletes.10
Conclusions- 1.
The incidence and public health importance of SR-SCD is not well determined. However, most authors conclude that it is very low and lower than the incidence of SCD in the general population. Therefore, the regular practice of sport is beneficial and safe. The incidence of SR-SCD does not differ between competitive and recreational athletes and it increases with age.
- 2.
CAD is the most frequent cause of SR-SCD among older athletes. SADS, ARVC, ILVH, HCM and CCA are the most frequent causes of death among young athletes.
- 3.
Preparticipation cardiovascular screening and dissemination of automatic external defibrillators (AED) are used to prevent SR-SCD. Both are complementary and indispensable. No screening program can provide absolute protection against SCD and AED are essential to improve morbidity and survival after SCA.
Preparticipation cardiovascular screening should be recommended to both competitive and recreational athletes. It should include medical history and physical examination. Further knowledge is needed to establish whether the incorporation of a 12-lead-ECG is required or not.
- 4.
A multidisciplinary approach, standardized autopsy protocols and a comprehensive enrollment and characterization of all cases, including the successfully resuscitated, are essential to better understand the epidemiology of SR-SCD.
The authors declare that they have no conflict of interest.