During the initial COVID-19 outbreak, health systems faced unprecedented organizational stress. Meanwhile, reports of episodes of discrimination and violence towards healthcare workers increased globally. This study explores the association between perceived discrimination and mental health outcomes in a large sample of healthcare workers in Spain.
Materials and methodsHealthcare workers from inpatient and outpatient facilities (N=2,053) filled an on-line questionnaire in May or June 2020. Mental health outcomes included depression symptoms (Patient Health Questionnaire [PHQ-9]), psychological distress (General Health Questionnaire [GHQ-12]) and death thoughts (Columbia Suicide Severity Rating Scale [C-SSRS]). We also measured perceived discrimination and/or stigmatization due to being a healthcare worker since pandemic onset. Regression models adjusted for potential confounding sources (age, sex, history of a mental health diagnosis and type of job) were fitted.
ResultsThirty percent of the respondents reported discrimination and/or stigmatization. Perceived discrimination was associated with higher depression (B=2.4, 95 percent CI: 1.8, 2.9) and psychological distress (B=1.1, 95 percent CI: 0.7, 1.4) scores, and with a 2-fold increase in risk of reporting death thoughts (OR=2.0, 95 percent CI: 1.4, 3.1).
ConclusionsPerceived discrimination is a modifiable driver of mental health problems among healthcare workers. Mass media, legislators, and healthcare institutions must put in place prevention and restoration strategies to limit discrimination towards healthcare workers and reduce its mental health impact.
Health systems faced unprecedented organizational stress during the initial COVID-19 pandemic outbreak. Increases in emergency care requirements drove generalized shortages in clinical staffing and suboptimal access to diagnostic and therapeutic resources and personal protective equipment. Healthcare workers (HCWs), especially those from initial COVID-19 hotspots, reported having to work during extended hours, often following redeployment to frontline positions, and experienced remarkable infection risk. For instance, in Spain, a nationwide seroprevalence study estimated a 25% infection rate among HCWs.1 Accordingly, HCWs are considered a particularly vulnerable group to psychological distress during the COVID-19 pandemic, and substantial attention has been directed towards HCWs’ mental health outcomes.2
The initial outbreak of the COVID-19 pandemic generated global manifestations of popular support in favor of HCWs, such as the “Thank you NHS” (United Kingdom) “Aplauso Sanitario” (Spain) or “On Applaudit” (France) movements. Mounting evidence, however, indicates that the pandemic also brought about increases in discrimination, stigma, and violence towards HCWs across the globe,3 mostly because HCWs are perceived as at higher risk of transmission,4 leading to growing calls for the enactment of governmental measures to protect HCWs.5
It seems plausible that discrimination may be a salient actionable driver of psychological distress and negative mental health outcomes among HCWs. Yet evidence of an association between perceived discrimination and negative mental health outcomes during the COVID-19 pandemic is scarce and comes from studies where important potential sources of confounding, such as personal history of a mental disorder or socioeconomic status, could not be ascertained and controlled for.6,7
Here, we used a large sample of Spanish HCWs to (1) explore the frequency of perceived discrimination during the initial outbreak of the pandemic and (2) examine the association between perceived discrimination and depression symptoms, psychological distress, and death thoughts.
Materials and methodsStudy design and participantsThis cross-sectional study is part of a prospective multi-national survey. Baseline procedures were conducted in three Spanish regions (Madrid, Andalusia, and Murcia) between April 24th and June 22nd, 2020.
The sample consists of HCWs from different outpatient and inpatient health facilities. We used the following sampling method: we contacted key stakeholders (e.g., hospital managers, clinical units’ supervisors, heads of worker unions) in each region and asked them to forward the survey link to every worker from the facility. A list of the facilities contacted is provided in the Appendix. To enhance response rates, we also asked workers to forward the survey to their peers. Respondents were considered eligible only if they were aged≥18 years and employed in a healthcare facility. Participants provided informed consent by signing an online form before starting the online survey.
All procedures contributing to this work comply with the Helsinki Declaration of 1975, as revised in 2013, and received approval from the Hospital La Paz Ethics Committee (Madrid, Spain).
VariablesAll information was self-reported. We included the following sociodemographic variables: age, gender, personal history of a mental disorder (assessed with the dichotomous item: “before the pandemic, did you have a mental health diagnosis?”), and type of job. We collapsed job types into the following categories: physicians, nurses, health technicians (e.g., nurse, X-ray, and laboratory technicians), ancillary workers (e.g., security staff, drivers, administrative staff, and cleaning staff), and other healthcare workers (e.g., clinical psychologists, physiotherapists, and biologists). To measure perceived discrimination, we included the following dichotomized item “As a healthcare worker, I have felt stigmatized and/or discriminated against due to COVID-19” (agree vs. disagree). Mental health outcomes included depression symptoms as measured by the Spanish version of the 9-item Patient Health Questionnaire (PHQ-9),8 psychological stress as measured by the Spanish version of the 12-item General Health Questionnaire,9 and death thoughts as measured by the Spanish version of the Columbia Suicide Severity Rating Scale (C-SSRS).10 Cronbach's alphas were 0.86 (95 percent CI: 0.85, 0.87) for the GHQ-12 and 0.88 (95 percent CI: 0.87, 0.89) for the PHQ-9.
Statistical analysesFirst, we removed respondents who provided informed consent but did not go on to initiate the survey (n=95), reported working at residential facilities where no healthcare is provided (n=96), or did not report job position (n=221).
Then, we reported categorical variables as frequencies and valid percentages and continuous variables as mean/median and standard deviations for the whole sample and stratified by perceived discrimination. Last, we explored the association between perceived discrimination and three mental health outcomes: depressive symptoms, psychological distress, and death wishes. To that end, we fitted three multivariable regression models where perceived discrimination was entered as the independent variable: two linear regression models (for depression and psychological distress) and one logistic regression model (for presence of death thoughts). Further, we repeated all analyses using screening positive to the PHQ-9 and GHQ-12 tests as the outcome, adopting cutoffs based on previous studies,11,12 using logistic regression models. All models were adjusted for the following potential sources of confounding: age, gender, personal history of a mental disorder, and type of job.
All analyses were conducted using R Studio for Mac (Version 1.2.5042).
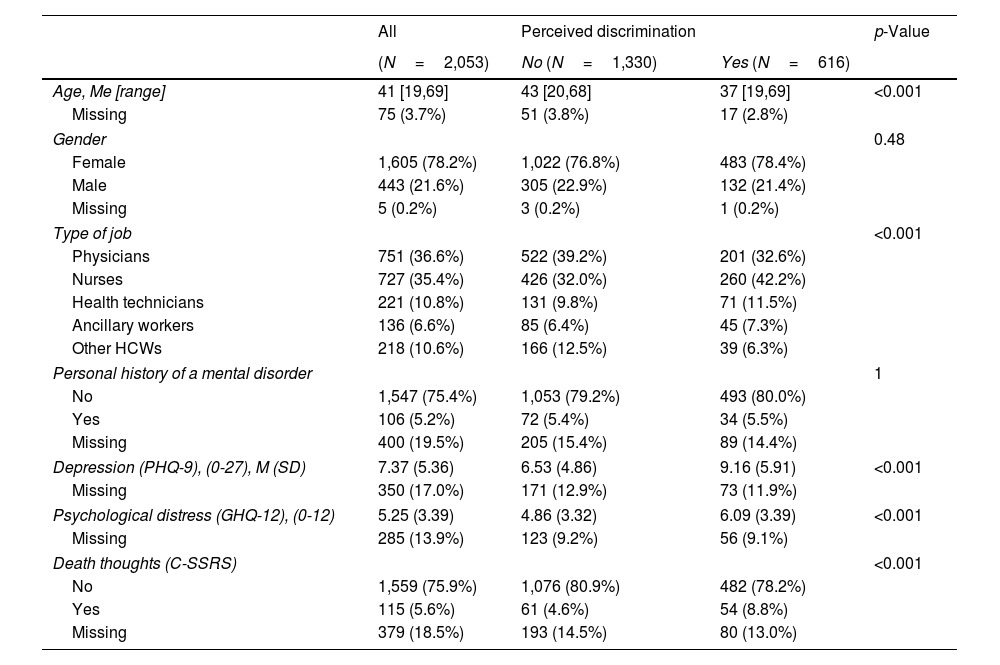
ResultsOur study sample includes 2.053 participants who completed the survey between April and June 2020. Table 1 summarizes respondents’ characteristics. Roughly one out of three reported stigmatization and/or discrimination due to being HCWs during the first peak of the pandemic in Spain.
Characteristics of the respondents stratified by perceived discrimination.
| All | Perceived discrimination | p-Value | ||
|---|---|---|---|---|
| (N=2,053) | No (N=1,330) | Yes (N=616) | ||
| Age, Me [range] | 41 [19,69] | 43 [20,68] | 37 [19,69] | <0.001 |
| Missing | 75 (3.7%) | 51 (3.8%) | 17 (2.8%) | |
| Gender | 0.48 | |||
| Female | 1,605 (78.2%) | 1,022 (76.8%) | 483 (78.4%) | |
| Male | 443 (21.6%) | 305 (22.9%) | 132 (21.4%) | |
| Missing | 5 (0.2%) | 3 (0.2%) | 1 (0.2%) | |
| Type of job | <0.001 | |||
| Physicians | 751 (36.6%) | 522 (39.2%) | 201 (32.6%) | |
| Nurses | 727 (35.4%) | 426 (32.0%) | 260 (42.2%) | |
| Health technicians | 221 (10.8%) | 131 (9.8%) | 71 (11.5%) | |
| Ancillary workers | 136 (6.6%) | 85 (6.4%) | 45 (7.3%) | |
| Other HCWs | 218 (10.6%) | 166 (12.5%) | 39 (6.3%) | |
| Personal history of a mental disorder | 1 | |||
| No | 1,547 (75.4%) | 1,053 (79.2%) | 493 (80.0%) | |
| Yes | 106 (5.2%) | 72 (5.4%) | 34 (5.5%) | |
| Missing | 400 (19.5%) | 205 (15.4%) | 89 (14.4%) | |
| Depression (PHQ-9), (0-27), M (SD) | 7.37 (5.36) | 6.53 (4.86) | 9.16 (5.91) | <0.001 |
| Missing | 350 (17.0%) | 171 (12.9%) | 73 (11.9%) | |
| Psychological distress (GHQ-12), (0-12) | 5.25 (3.39) | 4.86 (3.32) | 6.09 (3.39) | <0.001 |
| Missing | 285 (13.9%) | 123 (9.2%) | 56 (9.1%) | |
| Death thoughts (C-SSRS) | <0.001 | |||
| No | 1,559 (75.9%) | 1,076 (80.9%) | 482 (78.2%) | |
| Yes | 115 (5.6%) | 61 (4.6%) | 54 (8.8%) | |
| Missing | 379 (18.5%) | 193 (14.5%) | 80 (13.0%) | |
Note. PHQ-9=Patient Health Questionnaire – 9 items, GHQ-12=General Health Questionnaire – 12 items, C-SSRS=Columbia – Suicide Severity Rating Scale. p-Values from Wilcoxon Rank Sum Test (Age, Depression, and Psychological Distress), Fisher's Exact Test (Gender, Personal history of a mental disorder, and Death thoughts), and Pearson's chi-squared test (Type of job).
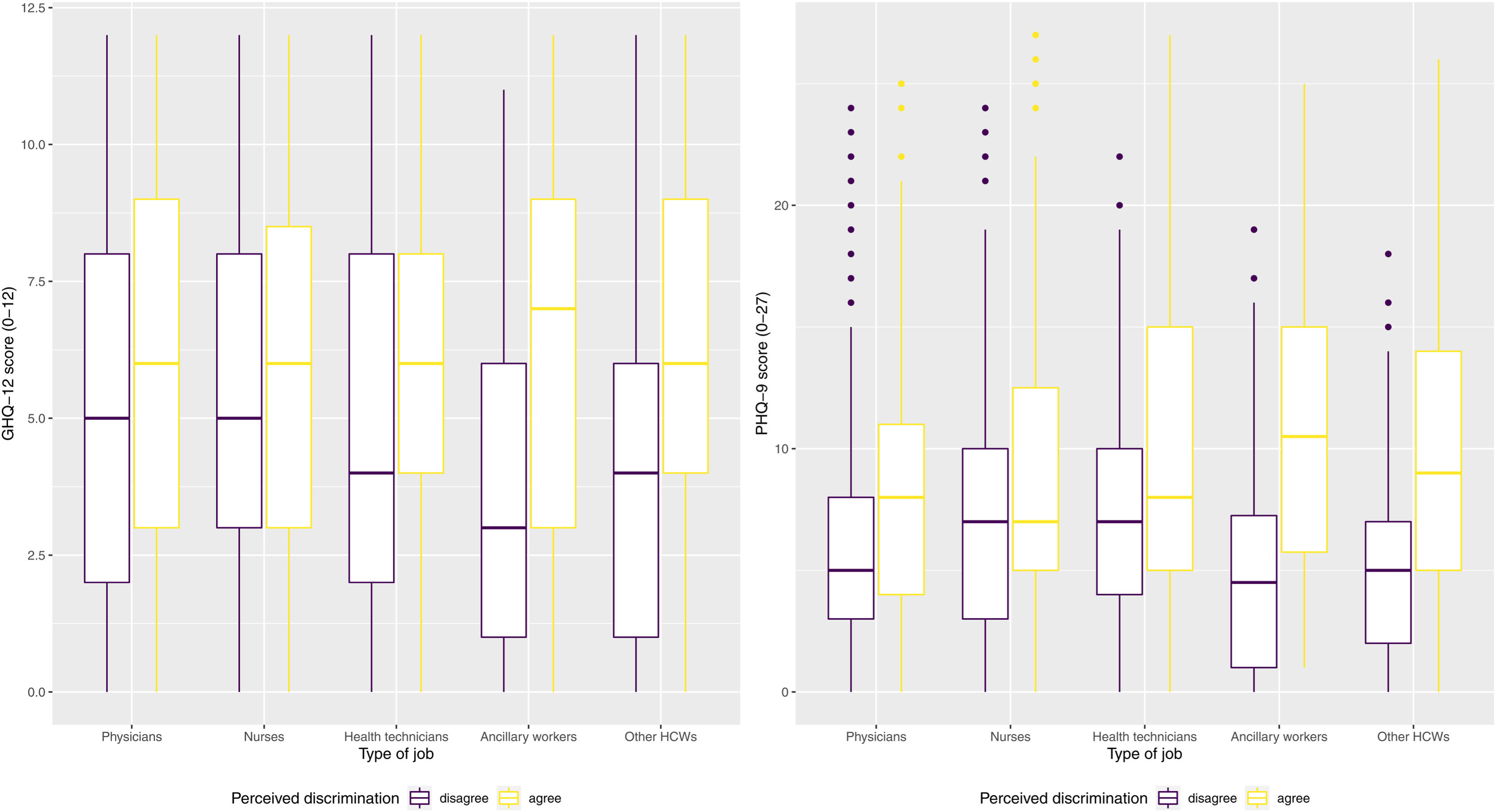
After adjusting for potential sources of confounding, on average, reporting perceived discrimination was associated with higher scores of depressive symptoms, as measured by the PHQ-9 (B=2.4, 95 percent CI: 1.8, 2.9), and psychological distress, as measured by the GHQ-12 (B=1.1, 95 percent CI: 0.7, 1.4) scores, and with a 2-fold increase in risk of reporting death thoughts (OR=2.0, 95 percent CI: 1.4, 3.1). Reporting discrimination also increased the risk of screening positive both in PHQ-9 (OR=1.6, 95 percent CI: 1.4, 1.9) and GHQ-12 (OR=1.4, 95 percent CI: 1.1, 1.6). A sensitivity analysis including parental education level as a proxy of childhood socioeconomic status did not modify results. Fig. 1 shows the association between mental health outcomes and type of job, stratified by presence of reported discrimination and/or stigmatization.
DiscussionIn a large sample of Spanish HCWs surveyed during the initial COVID-19 outbreak, we found that feelings of discrimination were frequent and positively associated with poor mental health outcomes, as measured by a variety of instruments. These results entail important implications, especially given the current global climate of violence towards HCWs: verbal and physical assaults against HCWs, long considered an important public health and social justice problem, seemingly increased during the first half of 2020, according to the International Committee of the Red Cross.13
Roughly in line with estimates reported elsewhere,14 we found that one in three respondents felt stigmatized and/or discriminated against since the beginning of the pandemic. Our finding of an association between reported experiences of discrimination and poor mental health is in keeping with previous evidence from the general population15 and enhances our understanding of one of the ways the pandemic may have impacted HCWs’ wellbeing. It seems plausible that the association between perceived discrimination and poor mental health outcomes may be causal, and discrimination against HCWs may be a salient actionable factor to enhance their mental health.
Our study is subject to limitations. Because we are reporting observational, cross-sectional associations, residual reverse causation and certain degree of residual confounding cannot be ruled out. Also, we measured perceived discrimination using an ad-hoc designed instrument, instead of including a standardized scale, due to limitations in survey space. Of note, this approach to measurement of discrimination is considered valid and has been widely used.16 Last, because we allowed participants to forward the survey to their peers, we could not accurately estimate response rates or describe the characteristics of HCWs who declined study participation, somewhat hindering generalizability of findings.
These results should generate attention and debate, as they highlight the importance of adopting and expanding recommendations to reduce discrimination and stigmatization against HCWs. According to the ICRC's Health Care in Danger strategy,13 such recommendations can be summarized as follows: (1) generalization of transparent protocols to guide clinical decision-making in contexts of limited access to resources – including clear communication of these protocols to the general public through responsible and accurate media reporting; (2) scheduled breaks and meals and a tight control to avoid HCWs’ overworking, and careful monitoring of HCWs’ mental health burden due to psychosocial stressors within or outside of the workplace – including access to individual and group interventions to promote wellbeing (e.g., low-intensity psychological interventions) if needed; and (3) enactment and enforcement of laws protecting HCWs against verbal and physical violence – including provision of adequate legal advice to HCWs who have experienced discrimination or violence.
Conflict of interestNone.
We thank all the people who took the time to fill the questionnaire.
The COVID-19 HEalth caRe wOrkErS – Spain (HEROES-SPA) Working Group is composed by Irene Martínez-Morata, Fabiola Jaramillo, Sergio Minué, Mario Rivera-Izquierdo, Cristina García Román, José Guzmán-Parra, Pablo Lorenzo Herrero, Ernesto Cañada, Matilde Blanco Venzalá, Agustín Sánchez, Eulalio Valmisa, Juan José Macheño, Marta Cañadilla Ferreira, Isabel López Tovar, M. Pilar Campos Navarro, Alicia Ibáñez Ros, Domingo A. Sánchez Martínez, Pablo Madrigal, José A. Guardiola, Santiago Serrano, M. Korina Bethencourt, Pedro A. López Romero, Eduardo Estrella and Elisabeth González Gómez.