Bipolar disorder causes a significant burden on the lives of patients and their families. The family is one of the targets for therapeutic intervention, related to the prognosis in patients with bipolar disorder.
AimTo assess the effectiveness of a multifamily psychoeducational program for people with bipolar disorder, in the family burden: objective and subjective and in the variables related to the course of the patients with bipolar disorder (symptoms, adherence, functionality, hospitalizations), comparing it with a control group (CG).
Materials and methodsA total of 148 relatives of bipolar patients and 148 bipolar patients were recruited. The sample was randomized (experimental group [EG] and CG) and with single-blind evaluations (baseline, at 5 months and one year). Clinical and sociodemographic variables were collected from families and patients (family burden self-report scale, Strauss-Carpenter Scale, Global Assessment of Functioning, Morisky Green adherence Scale). Both, EG and CG received 8 multifamily sessions, applied exclusively on the relatives of patients with bipolar disorder, but in the EG a psychoeducational treatment was carried out and in the CG only playful and current topics were discussed. Bivariate and logistic regression models were used, among others.
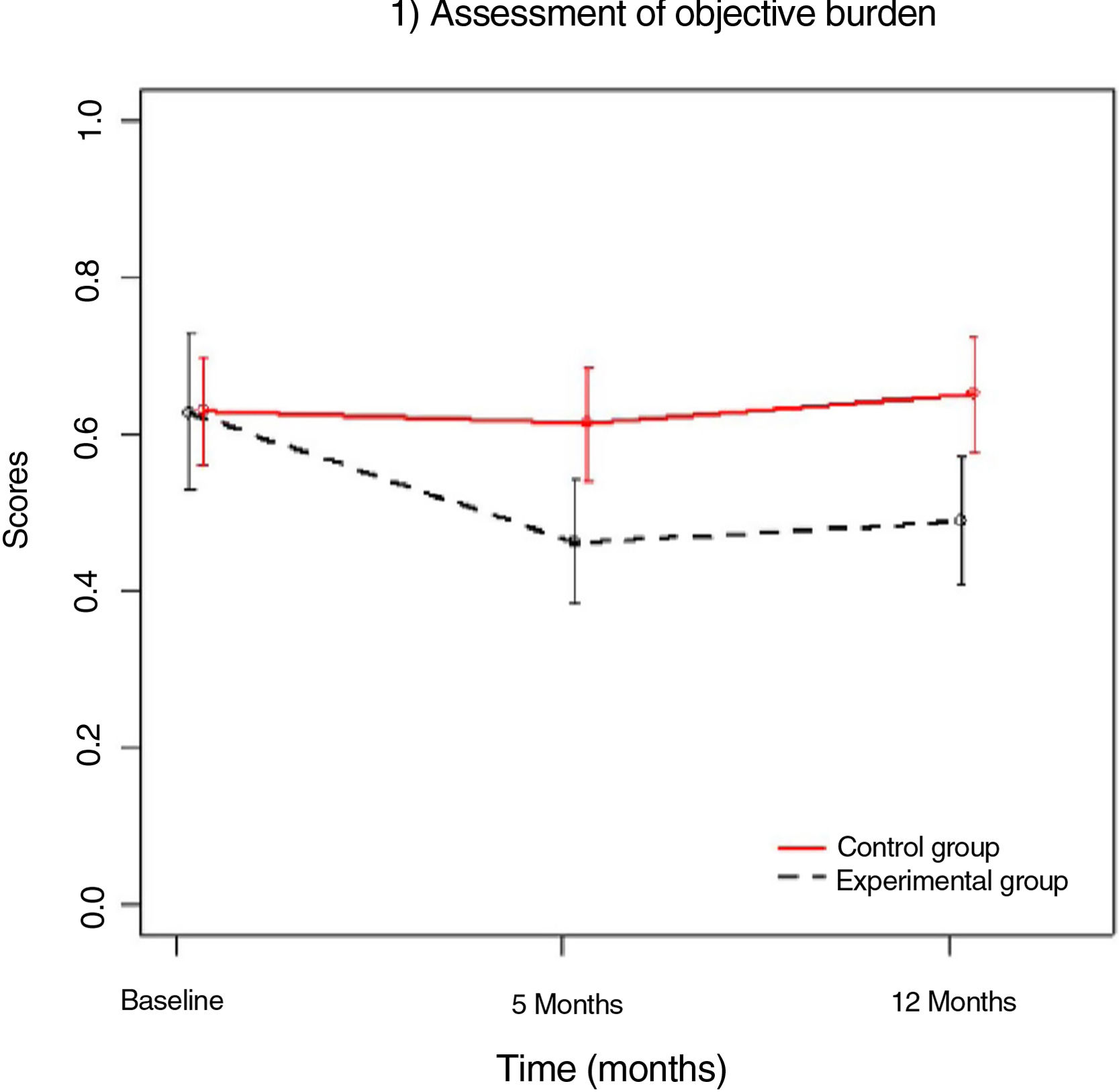
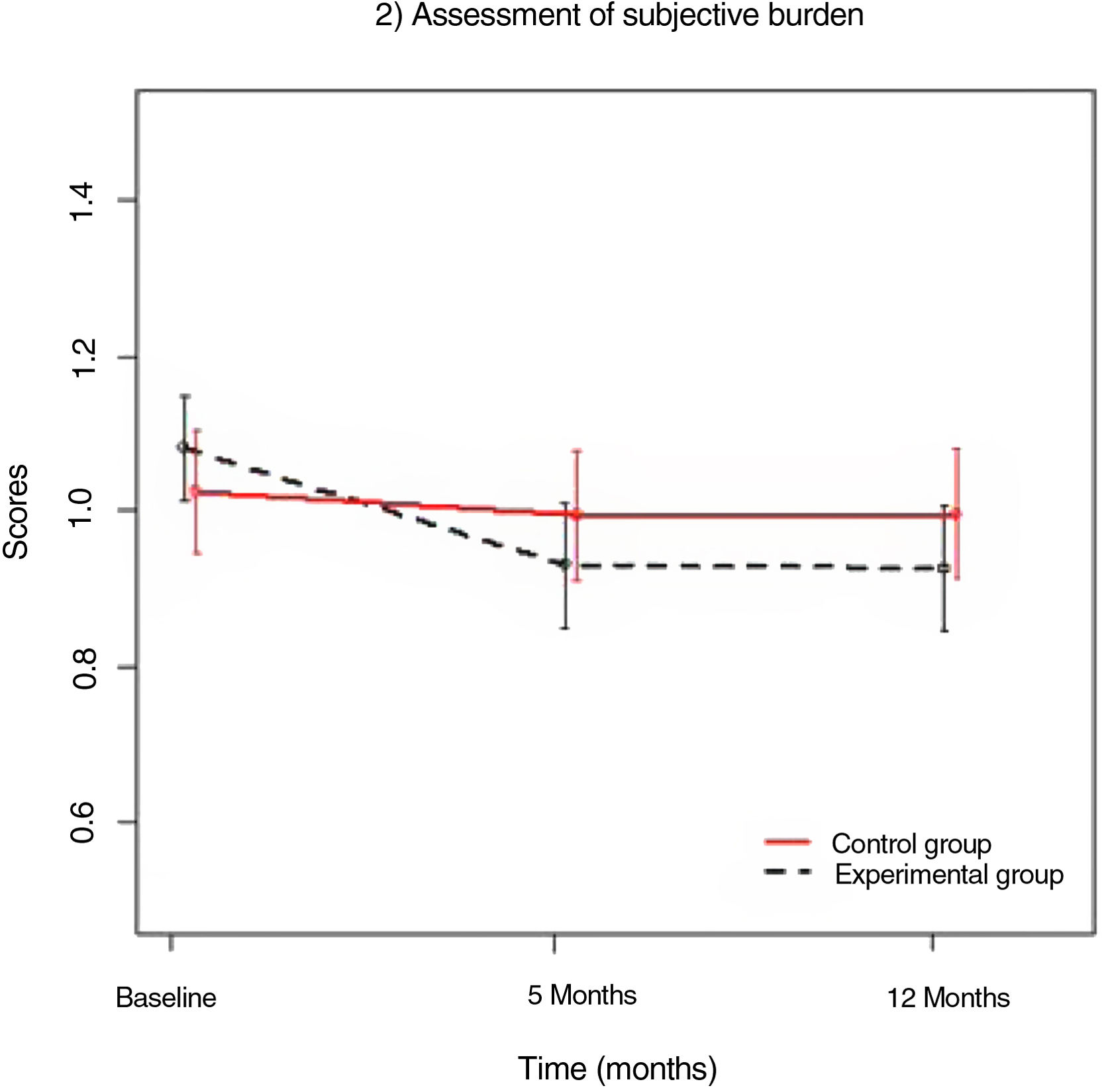
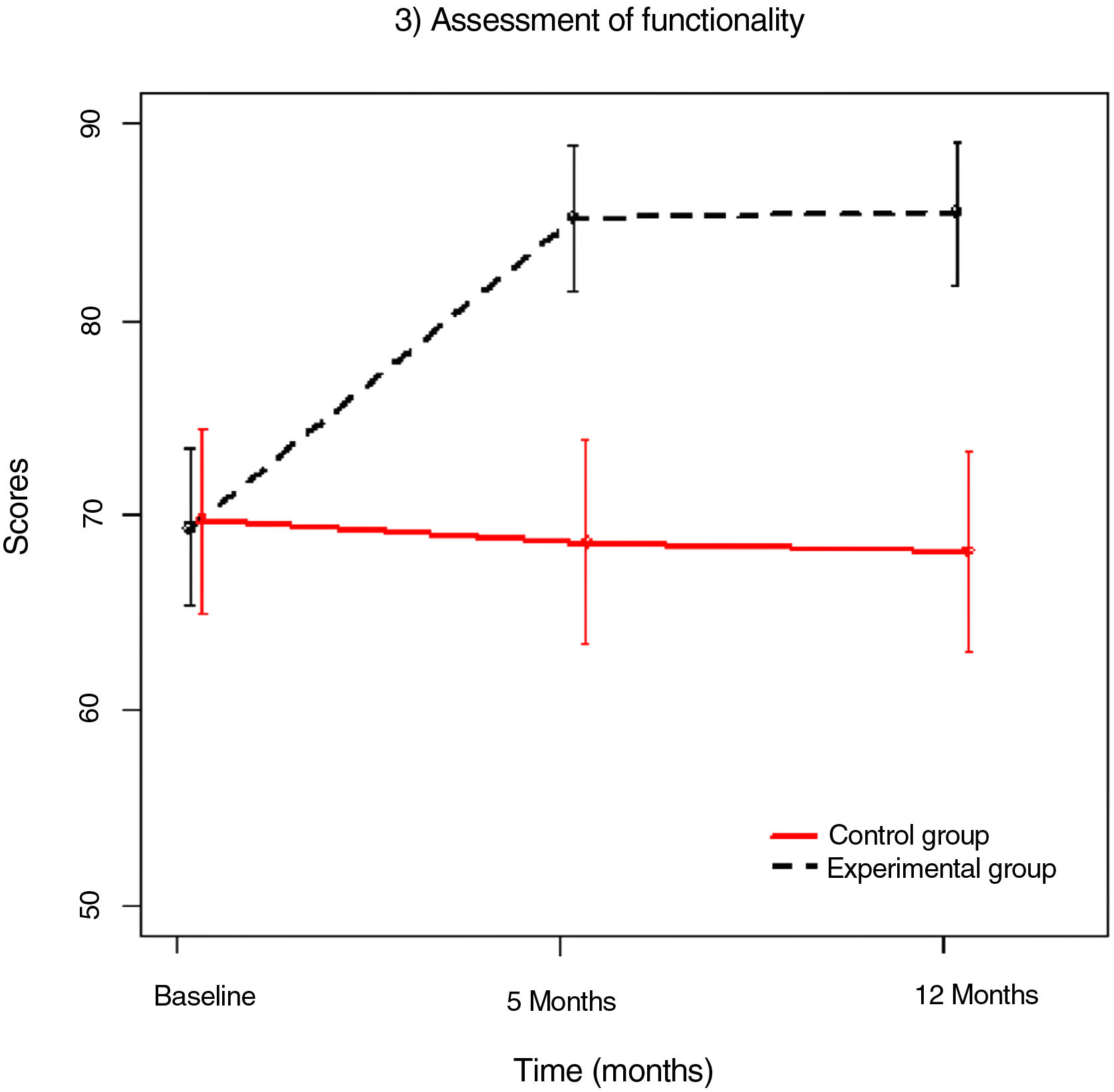
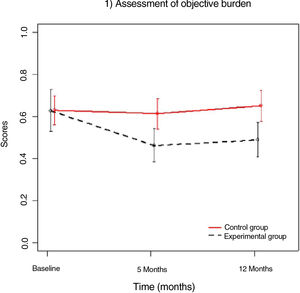
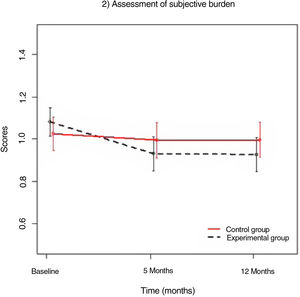
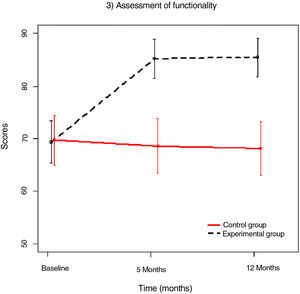
ResultsThe caregivers and patients of the EG and CG did not differ in any of the baseline variables (sociodemographic and clinical) (P>.001). In the total sample, the baseline objective burden was light (mean 0.6±0.4) and the subjective ones was medium-moderate (mean 1.1±0.3). During the follow-up, in relation to the variables of the caregivers, there was a greater reduction in the objective burden in the EG compared to the CG (5 months P=.006; one year P=.002). It was found that the objective burden (P=.006) and the subjective burden (P=.003) were significantly reduced over a year in EG but not in the CG. During the follow-up, the patients whose caregivers belonged to the EG showed a greater increase in the frequency of social activity (P=.008), in the work activity (P=.002), and global functioning (P=.002), and reduced their symptoms (P≤.001). Longitudinal analyses, over a year, showed that patients in the EG had a greater improvement in functionality compared to patients in the CG (P=.001). After the intervention, adherence to pharmacological treatment improved more in EG than in the CG (P≤.001). Regarding hospitalizations, any patients in the CG were hospitalized during the 5 months after the intervention, while 27.8% of the patients in the CG were hospitalized (P≤.001); the difference between groups remained significant in the long term (one year: P≤.001; 2 years: P≤.001). There were no significant differences between groups in the pharmacological treatment of the patients in any of the evaluations.
ConclusionsThe multifamily psychoeducational intervention group improved the family burden after the intervention. Likewise, bipolar patients, whose families attended the EG, improved significantly, over a year, the functionality, the frequency of social contacts, the work status, the adherence to treatment, and reduced their symptoms. In addition, in the EG, the percentage of hospitalizations during the 2 years of follow-up was significantly reduced.
Bipolar disorder (BD) is a chronic illness that causes functional decline in all areas of patients’ lives. It is among the diseases that cause the greatest family burden, and in Europe it ranks third.1,2 In 2008, the World Health Organisation ranked BD as the seventh leading cause of disability in men and the eighth in women.3 The consequences of BD have also been found to affect family members; in fact, they often experience a significant objective and subjective burden from their family member's illness.4 Family burden is described as the presence of problems, difficulties, or negative events that affect the lives of people important to patients, e.g., members of their household and/or their families.5 More than 90% of family members of BD patients report burden related to the disorder.4,6 It has been found that family members of people with BD continue to suffer moderate family burden even if they are in a prolonged euthymic state.7
However, the impact was found to be bidirectional. It was found that higher levels of baseline caregivers’ burden would predict an affective episode at 7 and 15 months follow-up in bipolar patients.8 Furthermore, caregivers’ expectations about the patient's ability to control symptoms were found to reflect greater burden on family members and a worse prognosis for the patient.6 Thus, it was found that the ability of relatives to recognise that the patient's behaviour is caused by their illness and not by their character results in a decrease in the burden they experience.9
Several authors point out that a very high percentage of bipolar patients (30%-50%) abandon their medication despite their doctor's advice and prescription.10–12 Controlled clinical trials demonstrate a consistent advantage of evidence-based psychotherapies (psychoeducation, cognitive behavioural therapy, family-centred therapy, social and interpersonal rhythm therapy, and peer support programmes) combined with pharmacological treatment, over the sole use of pharmacotherapy for this type of population.13 The inclusion of psychoeducation as an adjunct to pharmacological treatment in BD patients improves their outcome and prognosis,14,15 reducing hospitalisations and manic relapses.16,17 It has also been shown to be effective in improving patients’ functionality.18 Several authors have reported that treatments with relatives of BD patients have improved the burden experienced by these families19,20 and the symptoms and functional impairment of bipolar patients.19–21 In addition, most family members were able to detect early warning signs of relapse more easily, had improved quality of life, felt more involved, and perceived a higher quality of caregiving activities. Patients found that psychoeducation had helped with crises, increasing the feeling of being understood by relatives and generating positive changes in the whole family.22
However, there are few studies that do not include the patient in therapy.23–27 Intervention exclusively in family members has the flexibility to address barriers to implementation in patients and has sufficient structure to address the chaos associated with BD episodes.28 There is currently insufficient scientific evidence of the effectiveness of these treatments in family members of people with BD, as the studies are not of sufficient quality to draw definitive conclusions.29 Four years ago, the third version of the British Association for Psychopharmacology guidelines noted regarding psychotherapy in BD that future large-scale studies with concrete outcomes (hospital admissions) are needed.30 A recent study on family therapy in bipolar patients has been published which indicates that more research is needed to clarify the relationship between changes in family functioning and changes in the course of these disorders.20
The present study, a single-blind and randomised study, attempts to address these problems. In addition, the psychoeducational sessions were conducted in a standardised and structured manner and were of short duration (8 sessions). An implementation manual was created to ensure that the sessions were applied systematically in all groups. This is a longitudinal study with a large sample of family members and BD patients, in which long-term data were collected from both groups. The aim of this study was to analyse the short-term effect, that is, at the end of treatment (5-month assessment), and the long-term effect (annual and 2-year assessment) of a multifamily psychoeducational programme, applied exclusively to family members of BD patients, on the family burden of caregivers and on the prognosis of BD patients (functionality, adherence, symptoms, and hospitalisations), compared to a control group (CG).
Material and methodSampleA total of 152 caregivers were selected after randomisation to the groups; 4 family members in the CG dropped out at the beginning of the study for socio-demographic reasons (work and family: dependent children), and therefore the final sample comprised 148 family members of BD patients and 148 BD patients. One family member was allowed for each patient. All patients were selected from the area of the Hospital Universitario de Álava, Santiago Apóstol.
The inclusion criteria for BD patients were as follows: 1) age between 18 and 65 years; 2) with a diagnosis of BD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM), fourth edition (revised text)31; 3) to have given informed consent to participate in the study; and 4) within 10 years from diagnosis of the disease.
The inclusion criteria for families of people with BD were: 1) being the primary caregiver; 2) any family member, either first or second degree; 3) living with the family member or maintaining daily contact; 4) having signed the informed consent form; and 5) not having a serious mental disorder.
BD patients with substance-induced psychotic disorders, intellectual disability, or organic brain disorders were excluded. Axis 1 diagnosis of the revised DSM-IV text was made using the structured clinical interview for DSM-IV (SCID-I).32
All the BD patients received the usual individualised pharmacological treatment, primarily mood stabilisers. They also received individualised care at their mental health centre after discharge, usually with one visit per month. If needed, additional care was prescribed, including hospitalisations, regardless of the patient's socio-economic status, because this is a public hospital, and there are no private hospitals with a psychiatric service in the study area. A 24-hour emergency room was available if immediate care was needed.
AssessmentData were collected on the families of patients with a diagnosis of BD, who had to be in the first 10 years following diagnosis of the disorder. Caregivers and patients were then followed for one year after inclusion in the study (2 years for hospitalisations).
At study entry (baseline), families and patients, in each case, were assessed using a protocol that included different scales with good psychometric properties. Specifically, the self-report family burden scale (FBS) was used to assess family burden in families of bipolar patients.33 This scale assesses objective burden, referring to alterations in the daily functioning of those in the patient's environment, and each item can be scored from 0 to 2 (0: no burden; 1: some burden; 2: serious burden); it also assesses the subjective burden, that is, the respondent's stress, and each item in this section is scored from 0 to 2 (0: no stress; 1: moderate stress; 2: severe stress) and the level of attribution, that is, the degree to which the respondent relates the patient to the objective burden experienced (this last section was not included, as it was not the subject of the study). It has been found to be a useful instrument for assessing the effect of psychoeducational interventions on family burden.34 The Strauss-Carpenter prognostic scale35 was used to assess the patient's improved status in different areas (hospitalisations, work, symptoms, social activity, and global functioning). The Morisky-Green medication adherence scale was used for adherence to treatment.36 Patients with a score of 4 were considered to have “high” adherence, while those with a score of 0 to 3 were classified as “low” adherence; finally, the patient's global functioning was assessed with the Global Assessment Scale.37
Relevant clinical, functional, and demographic variables, such as pharmacological treatment and hospitalisations, were also collected for each bipolar patient. The same protocol was applied to all relatives at 5 months and one year after inclusion in the study, and the patients’ hospitalisations were also assessed at 2 years.
The main study variables for the relatives were objective and subjective burden, and hospitalisations and functionality (social activity, work activity, symptoms, global functioning) for the patients, throughout follow-up.
The assessment was masked and made by 2 investigators who had achieved good inter-rater reliability for SCID-I diagnoses (κ: .88). Caregivers and patients were systematically assessed by direct interview using the same methodology before and after the treatment period. Treatment was given by 2 psychologists experienced in group psychological treatments and in BD.
Ethical approvalThe study was conducted in accordance with the ethical principles of the Declaration of Helsinki. All participants received detailed information about the study and gave their written informed consent. The study was approved by the Hospital Ethics Committee of the Hospital Universitario de Álava, Santiago Apóstol, Vitoria, Spain.
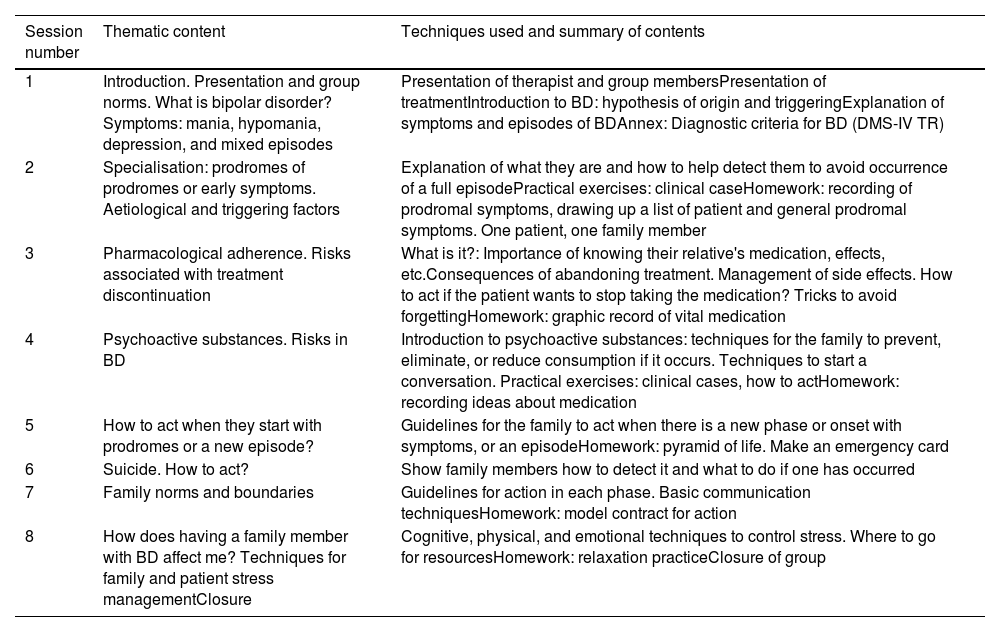
Experimental conditionsExperimental group: PROTEC programmeThe experimental group (EG) underwent the PROTEC programme, consisting of 8 standardised multifamily psychoeducational group sessions with cognitive-behavioural therapy. This programme was designed by our own group, who are very experienced in interventions with families and in the management of BD patients. However, to develop this programme, a review of the main scientific literature on psychoeducation and family therapy was undertaken to create the sessions. The sessions lasted 90min, 2 per month, for a total treatment duration of 4 months. The treatments were given by a psychologist (SB) expert in the field and in research from the psychiatry service of the University Hospital of Álava, Santiago Apóstol, while the assessments were made by another psychologist (PV or SRA) who did not know the experimental condition of the participant. Failure to attend more than 2 sessions was grounds for exclusion from the treatment. Table 1 shows the sessions, contents, and techniques used in the PROTEC programme.
Multi-family psychoeducational programme PROTEC: sessions, contents, and techniques (exclusively for family members of people with bipolar disorder).
| Session number | Thematic content | Techniques used and summary of contents |
|---|---|---|
| 1 | Introduction. Presentation and group norms. What is bipolar disorder? Symptoms: mania, hypomania, depression, and mixed episodes | Presentation of therapist and group membersPresentation of treatmentIntroduction to BD: hypothesis of origin and triggeringExplanation of symptoms and episodes of BDAnnex: Diagnostic criteria for BD (DMS-IV TR) |
| 2 | Specialisation: prodromes of prodromes or early symptoms. Aetiological and triggering factors | Explanation of what they are and how to help detect them to avoid occurrence of a full episodePractical exercises: clinical caseHomework: recording of prodromal symptoms, drawing up a list of patient and general prodromal symptoms. One patient, one family member |
| 3 | Pharmacological adherence. Risks associated with treatment discontinuation | What is it?: Importance of knowing their relative's medication, effects, etc.Consequences of abandoning treatment. Management of side effects. How to act if the patient wants to stop taking the medication? Tricks to avoid forgettingHomework: graphic record of vital medication |
| 4 | Psychoactive substances. Risks in BD | Introduction to psychoactive substances: techniques for the family to prevent, eliminate, or reduce consumption if it occurs. Techniques to start a conversation. Practical exercises: clinical cases, how to actHomework: recording ideas about medication |
| 5 | How to act when they start with prodromes or a new episode? | Guidelines for the family to act when there is a new phase or onset with symptoms, or an episodeHomework: pyramid of life. Make an emergency card |
| 6 | Suicide. How to act? | Show family members how to detect it and what to do if one has occurred |
| 7 | Family norms and boundaries | Guidelines for action in each phase. Basic communication techniquesHomework: model contract for action |
| 8 | How does having a family member with BD affect me? Techniques for family and patient stress managementClosure | Cognitive, physical, and emotional techniques to control stress. Where to go for resourcesHomework: relaxation practiceClosure of group |
BD: bipolar disorder.
The intervention received by the CG consisted of multi-family meetings with the same frequency as the GE format (90min sessions fortnightly for 4 months). In these meetings, recreational topics were discussed: news, books, and radio programmes.
Classification of the experimental groups: randomisationTwo groups were formed: EG and CG. Caregivers were randomly assigned to either group by randomisation software. Seventy-six families were randomly assigned to the EG and 76 to the CG (1:1). After allocation, as mentioned above, 4 family members were lost to the CG.
Statistical analysisQuantitative variables were expressed as mean±SD if they were normally distributed; otherwise, they were expressed as median, 25th percentile, and 75th percentile. Qualitative variables were expressed as absolute (n) and/or relative (%) frequencies.
Comparisons of baseline characteristics of relatives and patients, total, CG and GE were analysed with the Mann-Whitney U-test for quantitative variables and the χ2 test for qualitative variables.
Comparisons of means were performed for variables with 2 categories using Student's t-test, and for variables with 3 or more categories, by analysis of variance. Both tests were used to relate family burden and baseline socio-demographic and clinical variables.
Non-parametric tests, Mann-Whitney U and Kruskal-Wallis H (for more than 2 categories) were used for variables with a normal distribution.
Analysis of covariance was used to compare the family burden of the groups at 2 points in time: baseline and post, adjusting for the covariate at baseline, because it is used for continuous variables. Data were expressed using beta coefficients and their corresponding significance level.
Several regression models were used: multiple linear regression when the dependent variable was quantitative, and logistic when the dependent variable was dichotomous. A main independent variable was used, adjusting the model for variables that had been previously found to be related to the dependent variable. Once they were selected, we checked that they did not influence each other and if they did (collinearity) we removed them from the model. This method was used to analyse the relationship of the type of treatment with different clinical variables (burdens, functionality, relapses, hospitalisations; all of them at 5 months, 1 year, and 2 years). Data were expressed using beta coefficients and OR with p-values.
Mixed models were used to evaluate the evolution of a continuous variable, controlling for different variables, over different time points (minimum 3). This method was used to analyse the evolution of the CG and GE over the course of the study in terms of burdens and functionality. The data were expressed using beta coefficients and p-values.
Finally, each group (CG and EG) was analysed for sociodemographic and clinical variables, of both family members and patients, comparing the different assessments (baseline, 5-month, at 1 year, and at 2 years) with the Mann-Whitney U test for quantitative variables and the χ2 test for qualitative variables.
All data were analysed using SPSS® 24.0, and with the R® statistical programme. All variables were assessed at a significance level of less than .05.
ResultsBaseline characteristicsCaregivers of people with bipolar disorderTotal sample (n=148)A total of 148 family caregivers of patients with BD were finally selected. Of these, 47.30% were male and 52.70% female, with a mean age of 49.96±11.99 years. Of the family members in the sample, 62.2% were married; 40.5% were the patients’ parents and 23% were the patients’ partners; 57.5% lived permanently with the patients and 43.7% gave permanent care to the patient. Of the family members, 80.4% were working at the time of the baseline assessment.
The average objective burden (FBS objective burden) at baseline was .6±.4, corresponding to a mild level of objective burden; the average subjective burden (FBS subjective burden) was 1.1±.3, corresponding to a medium-moderate level. At the start of the study, 97.3% of the relatives had an objective burden, of which 2.8% had very high levels (FBS>1.5). Likewise, 98.6% of relatives had subjective burden, with 8.4% having a very high level (FBS>1.5).
The attendance rate of relatives at the meeting exceeded 85%.
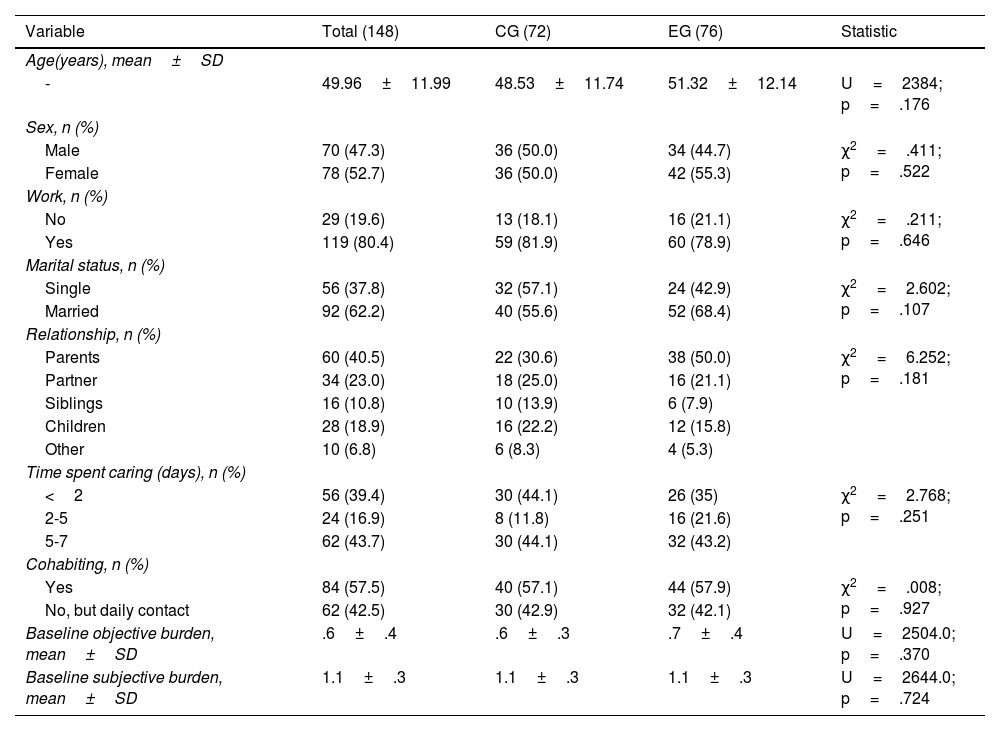
Experimental group (n=76) and control group (n=72)Table 2 summarises the baseline descriptive characteristics of each experimental condition (total, EG and CG). There were no significant differences between these groups in sociodemographic and clinical characteristics; thus, the proportion of women and men was similar, relationship, cohabitation, time spent caring, and level of burden.
Sociodemographic characteristics of caregivers of entire sample (n=148).
| Variable | Total (148) | CG (72) | EG (76) | Statistic |
|---|---|---|---|---|
| Age(years), mean±SD | ||||
| - | 49.96±11.99 | 48.53±11.74 | 51.32±12.14 | U=2384; p=.176 |
| Sex, n (%) | ||||
| Male | 70 (47.3) | 36 (50.0) | 34 (44.7) | χ2=.411; p=.522 |
| Female | 78 (52.7) | 36 (50.0) | 42 (55.3) | |
| Work, n (%) | ||||
| No | 29 (19.6) | 13 (18.1) | 16 (21.1) | χ2=.211; p=.646 |
| Yes | 119 (80.4) | 59 (81.9) | 60 (78.9) | |
| Marital status, n (%) | ||||
| Single | 56 (37.8) | 32 (57.1) | 24 (42.9) | χ2=2.602; p=.107 |
| Married | 92 (62.2) | 40 (55.6) | 52 (68.4) | |
| Relationship, n (%) | ||||
| Parents | 60 (40.5) | 22 (30.6) | 38 (50.0) | χ2=6.252; p=.181 |
| Partner | 34 (23.0) | 18 (25.0) | 16 (21.1) | |
| Siblings | 16 (10.8) | 10 (13.9) | 6 (7.9) | |
| Children | 28 (18.9) | 16 (22.2) | 12 (15.8) | |
| Other | 10 (6.8) | 6 (8.3) | 4 (5.3) | |
| Time spent caring (days), n (%) | ||||
| <2 | 56 (39.4) | 30 (44.1) | 26 (35) | χ2=2.768; p=.251 |
| 2-5 | 24 (16.9) | 8 (11.8) | 16 (21.6) | |
| 5-7 | 62 (43.7) | 30 (44.1) | 32 (43.2) | |
| Cohabiting, n (%) | ||||
| Yes | 84 (57.5) | 40 (57.1) | 44 (57.9) | χ2=.008; p=.927 |
| No, but daily contact | 62 (42.5) | 30 (42.9) | 32 (42.1) | |
| Baseline objective burden, mean±SD | .6±.4 | .6±.3 | .7±.4 | U=2504.0; p=.370 |
| Baseline subjective burden, mean±SD | 1.1±.3 | 1.1±.3 | 1.1±.3 | U=2644.0; p=.724 |
SD: standard deviation; CG: control group; EG: experimental group.
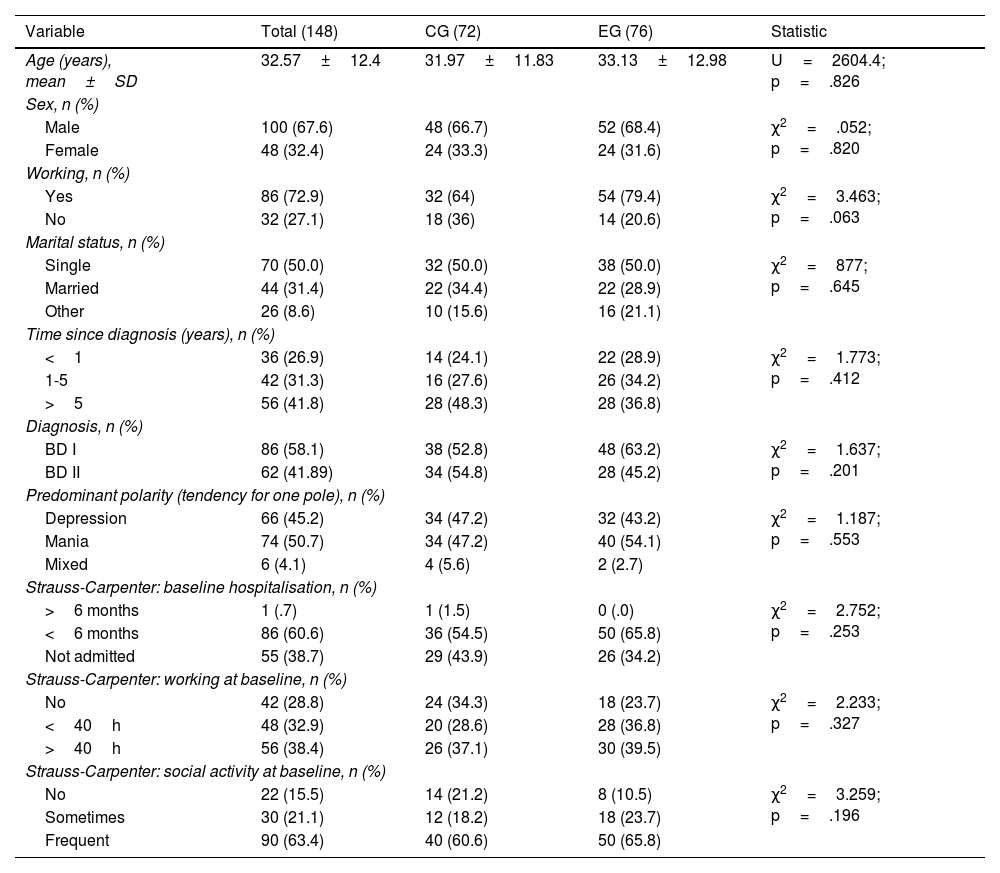
Table 3 shows the baseline results of bipolar patients whose relatives belonged either to the EG (n=76) or CG (n=72).
Baseline sociodemographic characteristics of the patients in the sample (n=148).
| Variable | Total (148) | CG (72) | EG (76) | Statistic |
|---|---|---|---|---|
| Age (years), mean±SD | 32.57±12.4 | 31.97±11.83 | 33.13±12.98 | U=2604.4; p=.826 |
| Sex, n (%) | ||||
| Male | 100 (67.6) | 48 (66.7) | 52 (68.4) | χ2=.052; p=.820 |
| Female | 48 (32.4) | 24 (33.3) | 24 (31.6) | |
| Working, n (%) | ||||
| Yes | 86 (72.9) | 32 (64) | 54 (79.4) | χ2=3.463; p=.063 |
| No | 32 (27.1) | 18 (36) | 14 (20.6) | |
| Marital status, n (%) | ||||
| Single | 70 (50.0) | 32 (50.0) | 38 (50.0) | χ2=877; p=.645 |
| Married | 44 (31.4) | 22 (34.4) | 22 (28.9) | |
| Other | 26 (8.6) | 10 (15.6) | 16 (21.1) | |
| Time since diagnosis (years), n (%) | ||||
| <1 | 36 (26.9) | 14 (24.1) | 22 (28.9) | χ2=1.773; p=.412 |
| 1-5 | 42 (31.3) | 16 (27.6) | 26 (34.2) | |
| >5 | 56 (41.8) | 28 (48.3) | 28 (36.8) | |
| Diagnosis, n (%) | ||||
| BD I | 86 (58.1) | 38 (52.8) | 48 (63.2) | χ2=1.637; p=.201 |
| BD II | 62 (41.89) | 34 (54.8) | 28 (45.2) | |
| Predominant polarity (tendency for one pole), n (%) | ||||
| Depression | 66 (45.2) | 34 (47.2) | 32 (43.2) | χ2=1.187; p=.553 |
| Mania | 74 (50.7) | 34 (47.2) | 40 (54.1) | |
| Mixed | 6 (4.1) | 4 (5.6) | 2 (2.7) | |
| Strauss-Carpenter: baseline hospitalisation, n (%) | ||||
| >6 months | 1 (.7) | 1 (1.5) | 0 (.0) | χ2=2.752; p=.253 |
| <6 months | 86 (60.6) | 36 (54.5) | 50 (65.8) | |
| Not admitted | 55 (38.7) | 29 (43.9) | 26 (34.2) | |
| Strauss-Carpenter: working at baseline, n (%) | ||||
| No | 42 (28.8) | 24 (34.3) | 18 (23.7) | χ2=2.233; p=.327 |
| <40h | 48 (32.9) | 20 (28.6) | 28 (36.8) | |
| >40h | 56 (38.4) | 26 (37.1) | 30 (39.5) | |
| Strauss-Carpenter: social activity at baseline, n (%) | ||||
| No | 22 (15.5) | 14 (21.2) | 8 (10.5) | χ2=3.259; p=.196 |
| Sometimes | 30 (21.1) | 12 (18.2) | 18 (23.7) | |
| Frequent | 90 (63.4) | 40 (60.6) | 50 (65.8) | |
BD: bipolar disorder; CG: control group; EG: experimental group; SD: standard deviation.
Of the total sample, the mean age of the patients was 32 years (SD 12.41). Most were male, single, employed, 58.1% had a diagnosis of type I BD and 41.89% of type II, 50.7% showed a greater tendency towards manic/hypomanic polarity, 45.2% depressive, and 4.1% mixed. Their functionality was acceptable (although slightly below 70), they did not have high pharmacological adherence, and they had been hospitalised during the year prior to inclusion in the study. A total of 41.8% had been diagnosed more than 5 years ago, 31.3% between 1 and 5 years ago, and 26.9% had been diagnosed less than one year ago. Most of the patients, during the month prior to inclusion in the study, presented with mild-moderate symptoms (65.3%). Most of the sample were not drug or alcohol users. The most frequently prescribed pharmacological treatment was second generation antipsychotics, combined with mood stabilisers and anxiolytics.
At baseline, there were no significant differences between the patients whose relatives were in the EG or the CG in any of the variables assessed, and therefore the groups were similar at baseline in terms of the patients’ symptoms and condition.
Assessments at follow-upCaregiversObjective family burdenThe EG had a significant decrease in objective family burden at the different follow-up time points (5 months: t=5.671, p≤.001, and at 1 year: t=5.671, p≤.001). The CG, however, showed no significant differences between baseline and post-treatment assessment (5 months: t=9.070, p=.288, and yearly: t=-1.212, p=.230).
On the other hand, no baseline differences were found within the groups in this variable, but significant differences were found at the 5-month assessment (EG .5±.3; CG .6±.3) (U=2,028.0; p=.006) and at the 1-year assessment (EG .5±.4; CG .6±.3) (U=1948.0; p=.002). The EG showed a significant reduction over the one-year follow-up, but the CG did not.
Objective burden was analysed with multiple linear regression, adjusting for hospitalisations, employment status, social activity, and patient adherence (at 5 months). Family members belonging to the CG had a lower objective burden at 5 months after the assessment than caregivers in the control group (β=−.198, p=.031). The same occurred at the annual assessment, the CG had a higher annual objective burden than relatives belonging to the EG (β=.177, p=.044).
When analysing the objective burden with mixed mathematical models, looking at the longitudinal evolution over one year controlling for different variables: subjective burden, hospitalisation, employment activity, social relations, and assessment of adherence and group type (EG and CG). Significant differences were found in the evolution of each group (EG and CG) in objective burden (β=−.016, p<.001). The CG had no significant change in levels of this type of burden throughout follow-up (β=.002; p=.469), but the EG had decreased objective burden during follow-up (β=−.017; p=.006) (Fig. 1).
Subjective family burdenIn the EG there were significant differences at the 5-month and 1-year assessment in subjective family burden (5-month: t=3.701, p≤.001, and 1-year: p=3.701, p≤.001). In contrast, no significant differences were found in the CG at baseline or at subsequent assessments (5 months and 1 year). There were no significant differences in the results between groups.
Subjective burden was also analysed with a multiple linear regression model, adjusting for several variables: group membership, hospitalisation, work activity, and objective burden. We found that being in the EG or CG did not significantly influence the presence of subjective burden at 5 months (β=0108, p=.193) or at one year from inclusion (β=.102, p=.229).
Subjective burden was analysed with mathematical mixed models, following the longitudinal evolution over one year in each group (EG and CG), controlling for different variables: objective burden, hospitalisation, work activity, social relations, adherence, and assessment and type of group (EG and CG). Significant differences were found in the evolution of each EG and CG group in terms of subjective burden over time (β=−.014, p=.006). The CG showed no significant change in subjective burden scores over follow-up, remaining constant over time (β=−.003, p=.320); however, the EG significantly reduced subjective burden over time (β=−.017, p=.003) (Fig. 2).
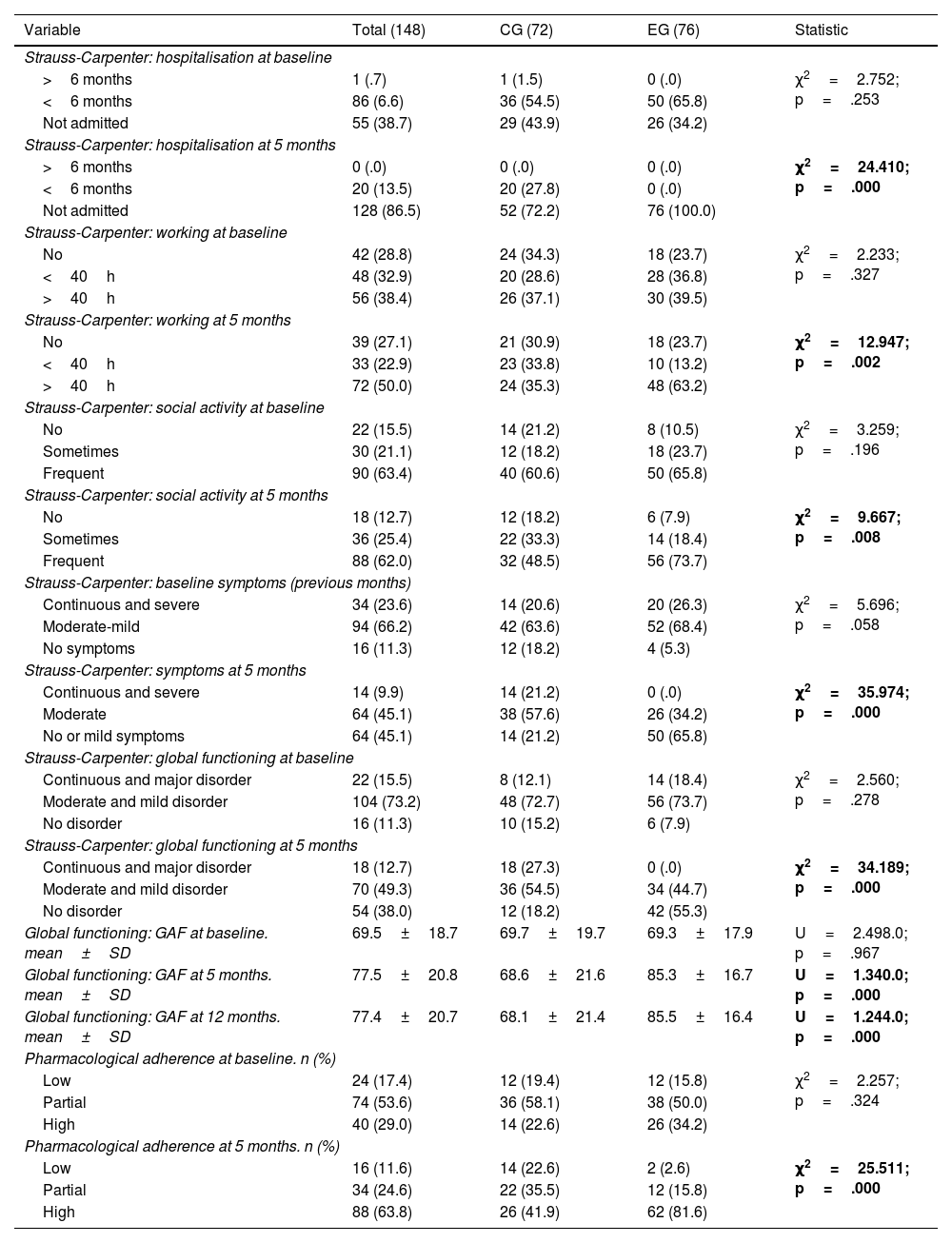
Patients diagnosed with bipolar disorder (n=148)In terms of functionality, adherence, and symptoms, when analysing the post-treatment assessment at 5 months, significant differences were found between the groups (EG and CG). Among the bipolar patients whose relatives belonged to the EG, there was a higher percentage of patients with full-time work activity, with a higher frequency of social relations, a higher percentage of euthymic patients, with less severity of symptoms, with better global functioning, and better adherence to treatment, compared to those in the CG. At the annual assessment, the SG patients were found to have significantly better functionality (EG: 85.3; CG: 68.6).
There were no significant differences between groups in the pharmacological treatment (none, antipsychotics plus stabilisers plus anxiolytics, stabilisers plus anxiolytics, antidepressants) of the patients at any of the assessment points (at baseline, 5 months, 1 and 2 years) (5 months: χ2=.000, p=1.000; annual: χ2=.000, p=1.000; 2 years: χ2=.338, p=.953) (Table 4).
Intergroup differences in functionality and symptomatology of patients in the control and experimental groups: assessments at baseline, 5, and 12 months.
| Variable | Total (148) | CG (72) | EG (76) | Statistic |
|---|---|---|---|---|
| Strauss-Carpenter: hospitalisation at baseline | ||||
| >6 months | 1 (.7) | 1 (1.5) | 0 (.0) | χ2=2.752; p=.253 |
| <6 months | 86 (6.6) | 36 (54.5) | 50 (65.8) | |
| Not admitted | 55 (38.7) | 29 (43.9) | 26 (34.2) | |
| Strauss-Carpenter: hospitalisation at 5 months | ||||
| >6 months | 0 (.0) | 0 (.0) | 0 (.0) | χ2=24.410; p=.000 |
| <6 months | 20 (13.5) | 20 (27.8) | 0 (.0) | |
| Not admitted | 128 (86.5) | 52 (72.2) | 76 (100.0) | |
| Strauss-Carpenter: working at baseline | ||||
| No | 42 (28.8) | 24 (34.3) | 18 (23.7) | χ2=2.233; p=.327 |
| <40h | 48 (32.9) | 20 (28.6) | 28 (36.8) | |
| >40h | 56 (38.4) | 26 (37.1) | 30 (39.5) | |
| Strauss-Carpenter: working at 5 months | ||||
| No | 39 (27.1) | 21 (30.9) | 18 (23.7) | χ2=12.947; p=.002 |
| <40h | 33 (22.9) | 23 (33.8) | 10 (13.2) | |
| >40h | 72 (50.0) | 24 (35.3) | 48 (63.2) | |
| Strauss-Carpenter: social activity at baseline | ||||
| No | 22 (15.5) | 14 (21.2) | 8 (10.5) | χ2=3.259; p=.196 |
| Sometimes | 30 (21.1) | 12 (18.2) | 18 (23.7) | |
| Frequent | 90 (63.4) | 40 (60.6) | 50 (65.8) | |
| Strauss-Carpenter: social activity at 5 months | ||||
| No | 18 (12.7) | 12 (18.2) | 6 (7.9) | χ2=9.667; p=.008 |
| Sometimes | 36 (25.4) | 22 (33.3) | 14 (18.4) | |
| Frequent | 88 (62.0) | 32 (48.5) | 56 (73.7) | |
| Strauss-Carpenter: baseline symptoms (previous months) | ||||
| Continuous and severe | 34 (23.6) | 14 (20.6) | 20 (26.3) | χ2=5.696; p=.058 |
| Moderate-mild | 94 (66.2) | 42 (63.6) | 52 (68.4) | |
| No symptoms | 16 (11.3) | 12 (18.2) | 4 (5.3) | |
| Strauss-Carpenter: symptoms at 5 months | ||||
| Continuous and severe | 14 (9.9) | 14 (21.2) | 0 (.0) | χ2=35.974; p=.000 |
| Moderate | 64 (45.1) | 38 (57.6) | 26 (34.2) | |
| No or mild symptoms | 64 (45.1) | 14 (21.2) | 50 (65.8) | |
| Strauss-Carpenter: global functioning at baseline | ||||
| Continuous and major disorder | 22 (15.5) | 8 (12.1) | 14 (18.4) | χ2=2.560; p=.278 |
| Moderate and mild disorder | 104 (73.2) | 48 (72.7) | 56 (73.7) | |
| No disorder | 16 (11.3) | 10 (15.2) | 6 (7.9) | |
| Strauss-Carpenter: global functioning at 5 months | ||||
| Continuous and major disorder | 18 (12.7) | 18 (27.3) | 0 (.0) | χ2=34.189; p=.000 |
| Moderate and mild disorder | 70 (49.3) | 36 (54.5) | 34 (44.7) | |
| No disorder | 54 (38.0) | 12 (18.2) | 42 (55.3) | |
| Global functioning: GAF at baseline. mean±SD | 69.5±18.7 | 69.7±19.7 | 69.3±17.9 | U=2.498.0; p=.967 |
| Global functioning: GAF at 5 months. mean±SD | 77.5±20.8 | 68.6±21.6 | 85.3±16.7 | U=1.340.0; p=.000 |
| Global functioning: GAF at 12 months. mean±SD | 77.4±20.7 | 68.1±21.4 | 85.5±16.4 | U=1.244.0; p=.000 |
| Pharmacological adherence at baseline. n (%) | ||||
| Low | 24 (17.4) | 12 (19.4) | 12 (15.8) | χ2=2.257; p=.324 |
| Partial | 74 (53.6) | 36 (58.1) | 38 (50.0) | |
| High | 40 (29.0) | 14 (22.6) | 26 (34.2) | |
| Pharmacological adherence at 5 months. n (%) | ||||
| Low | 16 (11.6) | 14 (22.6) | 2 (2.6) | χ2=25.511; p=.000 |
| Partial | 34 (24.6) | 22 (35.5) | 12 (15.8) | |
| High | 88 (63.8) | 26 (41.9) | 62 (81.6) | |
CG: control group; EG: experimental group; GAF: Global Assessment of Functioning scale. Data in bold indicate significance below .05.
When analysing functionality over one year with mathematical mixed models, significant differences were found in the evolution of each group (EG and CG) in terms of functionality over time (β=1.474, p<.001). The CG showed no significant changes in levels of functionality at follow-up, remaining constant over time (β=-.125, p=.383); however, the EG patients significantly increased their scores on the global assessment scale, that is, their functionality improved (β=1.349, p≤.001) (Fig. 3).
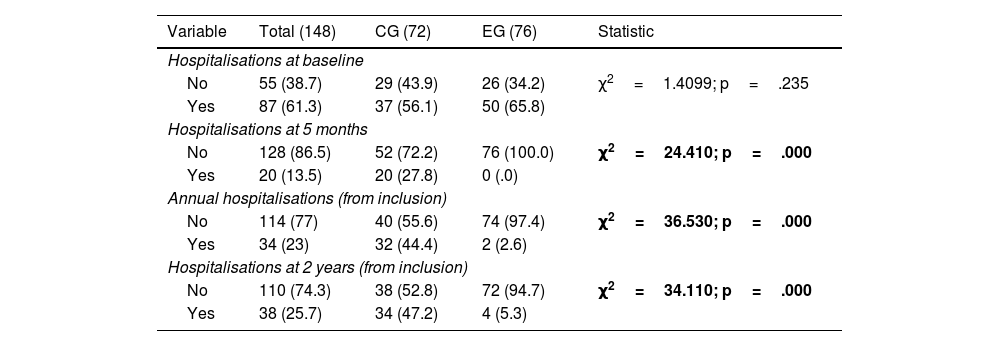
At the 5-month post-treatment assessment, significant differences were found between the groups in terms of hospitalisations (EG patients: 0%; CG: patients 27.8%). At the annual assessment, the EG patients were found to have significantly fewer hospitalisations (EG patients: 2.6%; CG patients: 44.4%). At the 2-year assessment, we found that patients in the EG had significantly fewer hospitalisations than the CG (EG patients: 5.3%; CG patients: 47.2%) (Table 5).
Intergroup differences in patient hospitalisations in the control and experimental groups: assessments at baseline, at 5 months, at 1 year, and at 2 years.
| Variable | Total (148) | CG (72) | EG (76) | Statistic |
|---|---|---|---|---|
| Hospitalisations at baseline | ||||
| No | 55 (38.7) | 29 (43.9) | 26 (34.2) | χ2=1.4099; p=.235 |
| Yes | 87 (61.3) | 37 (56.1) | 50 (65.8) | |
| Hospitalisations at 5 months | ||||
| No | 128 (86.5) | 52 (72.2) | 76 (100.0) | χ2=24.410; p=.000 |
| Yes | 20 (13.5) | 20 (27.8) | 0 (.0) | |
| Annual hospitalisations (from inclusion) | ||||
| No | 114 (77) | 40 (55.6) | 74 (97.4) | χ2=36.530; p=.000 |
| Yes | 34 (23) | 32 (44.4) | 2 (2.6) | |
| Hospitalisations at 2 years (from inclusion) | ||||
| No | 110 (74.3) | 38 (52.8) | 72 (94.7) | χ2=34.110; p=.000 |
| Yes | 38 (25.7) | 34 (47.2) | 4 (5.3) | |
CG: Control group; EG: Experimental group. Data in bold indicate significance below .05.
Long-term hospital admissions were also assessed with a logistic regression model in which the type of treatment (EG or CG) was the independent variable and admission (at 1 year and at 2 years) was the dependent variable, adjusted for several variables (post-treatment adherence, patient diagnosis, annual objective burden, and annual subjective burden), previously related to the type of treatment. At one year, the patients whose relatives belonged to the EG were less likely to be re-hospitalised after one year than the patients whose relatives belonged to the CG (β=4.812; OR=122.958; p≤.001). The model explained 63.2% (R2=.632) of the variability in annual hospitalisations. At 2 years, the patients whose families belonged to the EG were less likely to be re-hospitalised than those belonging to the CG (β=2.493; OR=12.099; p≤.001). The model explained 32.2% (R2=.322) of the variability of hospitalisations at 2 years.
DiscussionTwo main conclusions were drawn from this study. The most important is the improvement in the course of the disease in the BD patients in the EG, compared to the CG, which was assessed by the reduction in the number of hospitalisations over 2 years of follow-up, by the improvement in functionality, the improvement of symptoms, and by the improvement in adherence throughout the follow-up. The second conclusion is the reduction of family burden in the EG, compared to the CG, after application of group psychoeducational treatment, applied exclusively for family members of people with BD.
Specifically, the first of the findings concerns patients with a diagnosis of BD (it should be noted that the psychoeducational intervention was with family members exclusively and not with BD patients), significant differences were found in different areas between the EG and CG throughout follow-up, even though they were equivalent at baseline. These significant differences were found in the number of hospitalisations at 5 months, 1 year, and 2 years; thus, in the EG there were 20% fewer hospitalisations than in the CG, finding a significant reduction in hospitalisations over the entire 2-year follow-up. These findings are consistent with those of other authors.26,38 Bipolar patients were also found to significantly improve after treatment of their caregivers in the EG compared to the CG in symptoms, functionality - specifically at work -, social activity, global functioning, and adherence. Different authors have found an improvement after family treatment in patients’ adherence39,40 and functionality.41 However, it is important to highlight that most of the studies found include both patient and family members in treatments.
The second finding concerns caregivers, who were found to have a medium level of objective caregiver burden and a moderate level of subjective caregiver burden. These levels of burden at baseline are consistent with those reported in previous studies in caregivers of bipolar patients.42 However, other studies have reported higher levels of objective and subjective family burden.4,6 In addition, 97.3% report objective and 98.6% subjective burden symptoms, which is consistent with other authors.4,6 Both groups showed different development over one year, with the objective and subjective burden reducing significantly in the EG but not in the CG. Previous studies have also found a reduction in family burden through group family therapy.27
More specifically, these data are consistent with previous findings, where the burden experienced by caregivers of BD patients was influenced by their beliefs about the disorder6 and their perceptions of it. Gex-Fabry et al. find that positive changes perceived by patients in their family members were associated with improved quality of life for both.23 Indeed, Scott et al.39 state that perceived criticism and misunderstanding of the disorder are important risk factors for hospitalisation in BD. It has even been found that caregivers of bipolar patients with the knowledge of how best to manage these patients’ behaviours results in a reduction in their distress,43 because when caregivers of BD patients experience higher levels of burden, the patient's prognosis is negatively affected.44 Thus, a systematic review finds that the literature supports the conclusion that interventions that focus on family members have a beneficial impact on all family members.45 However, more rigorous studies with larger numbers of subjects are needed to confirm whether family treatments have concrete effects on the prognosis of BD patients.45
This study has a number of limitations; firstly, the sample size was limited (n=148), the number of sessions were short (8), although manualised and structured, with a moderate follow-up (one year for all variables in patients and family members and 2 years for hospitalisations in people with BD). Furthermore, the treatment was applied exclusively to the relatives of bipolar patients, requiring the participation of a relative willing to attend the psychoeducational groups, but as has been shown in this study and others, the attendance rate was high, at above 85%.46 A recent systematic review of patients with severe mental disorder, including BD patients, found that online treatment of family members not only improved family burden, but also reduced the severity of positive symptoms and fewer hospitalisations were recorded in patients compared to the control group.47 Therefore, this type of therapy could make it easier for family members who have greater difficulties to receive treatment. However, the fact that it is a brief treatment means that it can cover different areas that may be affected by BD, and it can easily be integrated into clinical practice.48 Thus, research on evolving pharmacological and psychological strategies in BD is now essential.49
It would be useful to conduct more randomised controlled studies, in a larger population and with longer follow-up, and including other endpoints, such as suicide attempts or comorbidities, and to vary the therapist applying treatments to avoid a possible drift effect. It is important that treatments are applied consistently and manualised. Thus, the effectiveness of family treatments, applied exclusively to caregivers, could be definitively assessed in terms of reducing symptoms, improving functionality, adherence, and hospitalisations in BD patients, and alleviating the family burden, assessing the prognosis and quality of life of both patient and caregiver. Nevertheless, the data from this study indicate that this type of intervention is a promising tool for both BD patients and their families in the short and long term.
ConclusionThis study confirms that there is a high rate of family burden among caregivers of BD patients, but also that this is a modifiable factor with specific therapy for this group, even if brief. It is important to note that this study was conducted exclusively with relatives of bipolar patients at any stage of their illness, which is an important strength of this study. We saw that, after applying a brief psychoeducational treatment aimed exclusively at relatives of people with BD, the prognosis of patients with BD significantly improved in terms of symptomatology, adherence, functionality, and long-term hospitalisations, and the family caregiver burden was reduced. It should be noted that the effectiveness of the treatment continued into the second year of follow-up.
AuthorshipSB wrote the first draft of the manuscript. All authors participated in drafting the manuscript and all approved the final version.
FundingThis study was funded by the Spanish Ministry of Economy and Competitiveness, through the Instituto de Salud Carlos III (ISCIII), and the European Regional Development Fund (ERDF) (PI070639). Funding Agency: Basque Government (2007/04).
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to acknowledge the support of the International University of La Rioja (UNIR). We are grateful to the following institutions: Basque Foundation for Innovation and Research in Health (BIOEF), the Centre for Biomedical Research in Mental Health Network (CIBERSAM), the University of the Basque Country, and the Bioaraba Health Research Institute.