The aim of the present study is to estimate the lifetime prevalence of suicidal ideation, plans, and attempts in a regional representative sample and the association of these outcomes with sociodemographic factors, prior mental disorders, and childhood adversities.
Material and methodsThe PEGASUS-Murcia project is a cross-sectional survey of a representative sample of adults in Murcia that is part of the WHO World Mental Health Survey Initiative. The Composite International Diagnostic Interview (CIDI 3.0) was administered face-to-face to 2621 participants (67.4% response rate). The main outcomes were suicidal ideation, plans, and attempts. Lifetime prevalence, age of onset, and risk factors (sociodemographic variables, mental disorders, and childhood adversities) were examined using multiple discrete-time survival models.
ResultsLifetime prevalence of suicidal ideation, plans and attempts were 8.0% (standard error, SE: 1.1), 2.1% (SE: 0.3), and 1.2% (SE: 1.1), respectively. Prevalence of any childhood adversities was 22.1% (SE: 1.3) in the total sample and, even higher, among those with suicide related outcomes (ranging between 36.8% and 53.7%). Female sex, younger age, prior (to onset of the outcome) lifetime prevalence of mood disorders, number of mental disorders, and exposure to childhood adversity were associated with significantly increased odds of suicidal ideation and plans.
ConclusionsLifetime prevalence estimates of suicidality are similar to those in community epidemiological surveys. Childhood adversities and mental disorders, especially mood disorders, are important risk factors for suicidality. Early detection of these adversities and disorders should be targeted in suicide prevention programs.
Suicide is one of the leading causes of death, the second in those people between 15 and 29 years and the 15th within general causes of death worldwide.1 Although the prevalence and characteristics of suicidal thoughts and behavior vary widely over time and between regions of the world, more than 800,000 suicide deaths are reported each year, which represents an global age-standardized suicide rate of 11.4 per 100,000 person-years (15.0 for males and 8.0 for females).1 In Spain, age-adjusted rates of suicide vary from 6.76 to 7.02 per 100,000 inhabitants depending on the restrictive vs. broad definition of suicide used2 and time periods considered.3 Suicide attempts and ideation are relatively common in the general population4 and a prior suicide attempt is considered the single most important predictor of subsequent suicide deaths as well as other non-fatal suicidal behaviors.1
The WHO World Mental Health (WMH) Survey Initiative was initially designed to carry out comparable epidemiological surveys on mental disorders in different countries all over the world with similar design and diagnostic instruments.5 This initiative overcomes an important factor of heterogeneity and limitation among studies focused on suicidal behavior due to different designs, populations, and instruments used. In a sample of 17 countries from different continents, the cross-national lifetime prevalence of suicidal ideation, plans, and attempts was 9.2% (standard error, SE: 0.1), 3.1% (SE: 0.1), and 2.7% (SE: 0.1), respectively.6 Data from the Spanish portion of the European Study on the Epidemiology of Mental Disorders (ESEMED) carried out between 2001 and 2002 yielded lower estimated (4.4% (SE: 0.3), 1.4% (SE: 0.2), and 1.5% (SE: 0.2), respectively).7 Despite significant cross-national variability in prevalence of suicidal behavior, consistency in some related sociodemographic characteristics have been described (e.g., being female, younger age, fewer years of education, and unmarried).6 The risk of transition from suicidal ideation to plan and attempt seems to be higher within the first year of onset of ideation.6-9 Other described risk factors to increase the risk of suicidal behavior are the presence of prior mental disorders consistently increased the risk of suicidal behaviors4,7,10,11 and different types of childhood adversities, especially sexual and physical abuse.12,13
The prevalence and risk factors related to suicidal behavior may vary over time and across regions,14 so that, replication of prior studies with similar designs and survey instruments in different samples representative of general population is justified.1 For example, a nationally representative Spanish sample was surveyed between 2011 and 2012, ten years after the ESEMED Study, in the context of the Collaborative Research on Ageing in Europe project (the COURAGE project).10 The latter study estimated the lifetime prevalence of suicidal ideation, plans, and attempts at 3.6%, 1.92%, and 1.46% across all regions of Spain. However, substantial geographical variations has been reported among Spanish provinces with regard to suicide rates.2 National estimates should therefore be interpreted with caution and new epidemiological surveys focused on smaller regional units which independently govern mental health care and policy should be performed.15 This is the case of Autonomous Communities in Spain, as they are responsible of health care in their territories.16
The PEGASUS-Murcia (Psychiatric Enquiry to General Population in Southeast Spain-Murcia) project is a cross-sectional survey based on a representative sample of the adult non-institutionalized general population of Murcia Region, one of the 17 Autonomous Communities of Spain, conducted between 2010 and 2012.17 It was designed to study the prevalence, protective, and risk factors of mental disorders in the context of the WMH-Survey Initiative. This project represents an opportunity to analyze the consistency of previous results on the prevalence of suicidal behavior and risk factors, including sociodemographic factors, childhood adversities and prior mental disorders, in an independent sample of general population of the South-East of Spain, with a special attention on those factors related to transition from suicidal ideation to plan or attempts. The aims of the current study were to estimate the lifetime prevalence of suicidal thoughts and behaviors in the general population of Murcia, and the association between suicidality, sociodemographic characteristics, mental disorders, and childhood adversities.
Material and methodsThis cross-sectional study has been written according the STROBE (Strengthening The Reporting of Observational Studies in Epidemiology) statement guideline.18 The protocol was approved by the Clinical Research Ethics Committee of the University Hospital Virgen de la Arrixaca of Murcia. All participating respondents provided written informed consent. No financial incentive was given for respondents’ participation.
SamplingThe PEGASUS-Murcia (“Psychiatric Enquiry to General Population in Southeast Spain-Murcia”) project is a cross-sectional population-based survey on a representative sample of the adult non-institutionalized general population of the Murcia Region (Spain) and was carried out between 2010 and 2012 as part of the World Mental Health (WMH) Survey Initiative (http://www.hcp.med.harvard.edu/wmh/).19 The protocol with further description of the sampling frame, selection and weighting procedures and a general description of participants has been described in more details elsewhere.17,19 Briefly, a total of 2621 participants, with an overall response rate of 67.4% (ranging from 62 to 70% across different health areas), were interviewed in person. Respondents were 50.5% male, mean age 48.6 years, 44.0% completed 12 or more years of education while 56.0% completed less, 76.2% were living in urban settings (>10,000 inhabitants) and 71.1% were married or cohabitating.
Diagnostic assessmentThe WHO Composite International Diagnostic Interview (CIDI 3.0, hereafter referred to as CIDI) is a comprehensive, highly-structured interview applied by lay examiners in face-to-face interviews and generates diagnoses based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).20 The instrument is divided into two parts to optimize the duration of the interview and to reduce respondent burden. Part I was administered to all respondents and Part II was only administered to a subsample of individuals consisting of all those with Part I lifetime core disorders and a probability sub-sample of the remaining Part I respondents. The CAPI (Computer-Assisted Personal Interviewing) version of the, specifically adapted for use in Spain,21 was used as it was originally designed to facilitate the skips and randomization patterns of questionnaire pathways into both parts (I and II) of the instrument (described in 19).
Assessment of suicidal thoughts and behaviorsThe suicidality module of the CIDI was used to assess the lifetime occurrence and AOO of suicide ideation, plan and attempt. The specific question asked was: “Have any of these experiences happened to you?” First the interview questioned: “You seriously thought about committing suicide”, “You made a plan for committing suicide” and after “You attempted suicide”. These 3 questions were printed in a booklet and referred to by an alphabetic letter (A, B, or C, respectively) with the aim of ensuring participants the greatest freedom of response in an effort to diminish the likelihood of the social desirability response bias frequently associated with interviewer's administration of potentially sensitive questions. In the present study, three lifetime history suicide outcomes were considered: suicide ideation, plan and attempt considered both in the total sample and among ideators.
Risk factors for suicide-related outcomesFour sets of risk factors for suicide-related outcomes were examined: (i) sociodemographic factors; (ii) presence of suicide plan and attempt since onset of suicide ideation; (iii) prior mental disorders; and, (iv) childhood adversities. The sociodemographic data were all categorized and included sex, age/cohort, family income at the time of interview (four-category income scale calculated as the ratio of family income in the past 12 months divided by the median income for Spain: low, low average, high average and high income), ever married, education level (categorized in none or primary – 0–7 years of education-, basic – 8–11 years-, secondary – 12–15 years- and college – 16 or more years of education-), and employment status (before or after first employment). Lifetime presence and age-of-onset (AOO) of each outcome were assessed by interview. Early onset we defined if AOO was prior to the age of 21 years, middle if AOO was between 21 and 33 years of age, and late if AOO was after 33 years of age in coherence with previous publications.6,7
Childhood adversities, defined as those occurring prior to age 18, were assessed with retrospective self-reports22 used in a number of international general population epidemiological studies.13,23 Twelve dichotomous variables (yes/no) were investigated: four adversities related to parental maladjustment (mental illness, substance misuse, criminality and domestic violence), three adversities depicting maltreatment (physical abuse, sexual abuse, and neglect), and other adversities covering parental death, parental divorce, other parental loss, serious physical illness and family economic adversity.
The mental disorders assessed included: Mood Disorders (major depression, bipolar disorder and dysthymia), Anxiety Disorders (generalized anxiety disorder, social phobia, specific phobia, post-traumatic stress disorder, agoraphobia without panic, panic disorder, obsessive compulsive disorder and adult separation anxiety disorder), Substance Disorders (alcohol and drug abuse and/or dependence), and Impulsive Disorders (oppositional-defiant, conduct and attention deficit disorders). For substance use disorders, abuse was defined with or without dependence in recognition of abuse being a stage in the progression to dependence. Prevalence estimates of mental disorders were determined based on whether respondents’ past or current symptomatology met the lifetime diagnostic criteria for a DSM-IV disorder prior the AOO of any suicidal behavior. Lifetime prevalence and retrospectively reported age-of-onset (AOO) were assessed for each disorder.
Statistical analysisCross-tabulations were used to estimate the lifetime prevalence of suicide ideation, plans, and attempts by sex, as well as prevalence of childhood adversities among those with suicidal thoughts and behaviors. Discrete-time survival analyses with time-varying covariates using logistic regression with person-years as the unit of analysis were used to study retrospectively assessed sociodemographic (sex, age, family income, ever married, years of education and employment status), diagnostic and childhood adversities correlates of each outcome (ideation, plan, attempt, and plan and attempt among ideators).24 Childhood adversities were assumed to have occurred prior to the outcomes, whereas the mental disorders were included as predictors only if their reported AOO was prior to the AOO of the outcome. Coefficients were converted to odds ratios (ORs) for ease of interpretation and 95% confidence intervals (95%CI) were also reported.
Weighting procedures are described in more details elsewhere.19 Briefly, part 1 weights were used to adjust for differential probabilities of selection, and an additional part 2 weight was applied to adjust for oversampling of high-risk individuals was used to restore distribution of the general population in terms of sex, age and health-care area within Murcia. All analyses were weighted with part 2 weights, and standard errors, confidence intervals and inference tests were obtained using the Taylor series linearization method25 implemented in the STATA software Version 14.2, using the “svy” command with weights specified as “probability weights” to adjust for the effects of sampling weighting and clustering on the precision of estimates.26
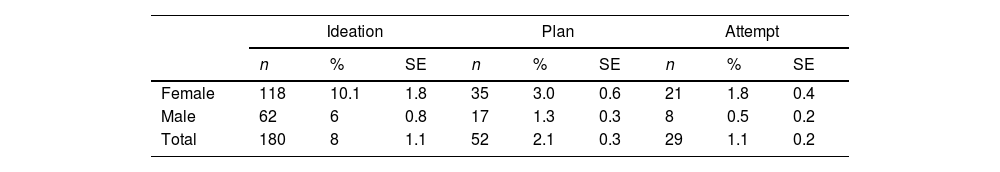
ResultsLifetime prevalence of suicidal behavioursThe lifetime prevalence estimates of suicidal ideation, plans, and attempts were 8.0%, 2.1%, and 1.2%, respectively (Table 1). Females had higher lifetime prevalence than males for all three outcomes. Among ideators (n=180), the conditional probability of ever making a plan or an attempt was 26.3% and 14.3%, respectively. The conditional probability of ever making an attempt was higher among ideators with a plan (49.6%) than those without a plan (1.7%).
Lifetime prevalence of non-fatal suicide behavior (ideation, plan and attempts) in Murcia (Spain). (Total sample n=1459).
| Ideation | Plan | Attempt | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | SE | n | % | SE | n | % | SE | |
| Female | 118 | 10.1 | 1.8 | 35 | 3.0 | 0.6 | 21 | 1.8 | 0.4 |
| Male | 62 | 6 | 0.8 | 17 | 1.3 | 0.3 | 8 | 0.5 | 0.2 |
| Total | 180 | 8 | 1.1 | 52 | 2.1 | 0.3 | 29 | 1.1 | 0.2 |
| Among ideators | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Plan | Attempt | Unplanned attempt | Planned attempt | |||||||||
| n | % | SE | n | % | SE | n | % | SE | n | % | SE | |
| Female | 35 | 29.5 | 5.3 | 21 | 18.1 | 5.0 | 1 | 0.3 | 0.2 | 20 | 60.8 | 9.8 |
| Male | 17 | 21.0 | 5.0 | 8 | 8.0 | 3.6 | 2 | 3.8 | 3.3 | 6 | 23.7 | 12.5 |
| Total | 52 | 26.3 | 2.8 | 29 | 14.3 | 3.5 | 3 | 1.7 | 1.6 | 26 | 49.6 | 9.8 |
SE: standard error.
Weighted percentages.
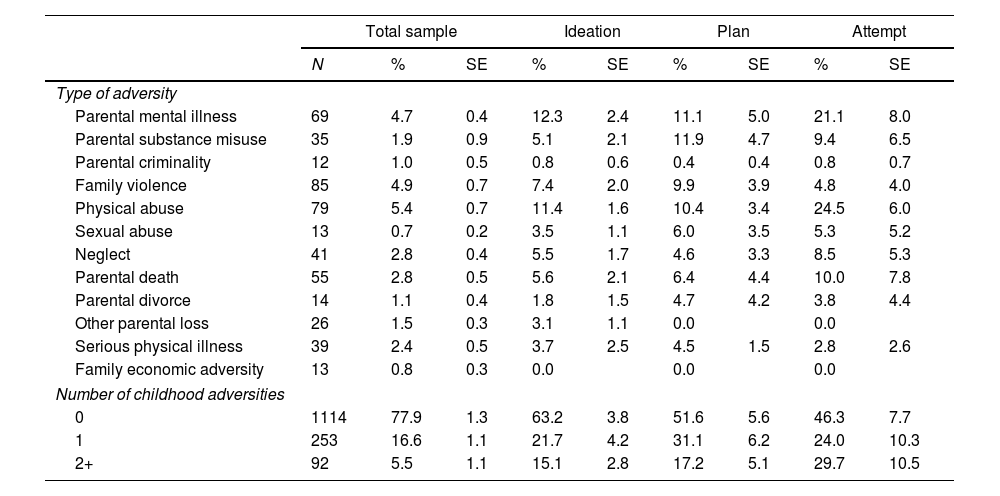
Childhood adversities were common (Table 2). The prevalence of any childhood adversity was 22.1% in the total sample and 5.5% reported two or more CAs. Prevalence was higher among individual with lifetime suicidal behaviors, ranging from 36.8% to 53.7%. The prevalence of individual childhood adversities ranged between 0.7% (sexual abuse) and 5.4% (physical abuse). The two most prevalent childhood adversities (over 10%) among non-fatal suicide behaviors were parental mental illness and physical abuse.
Prevalence of childhood adversities among participants with suicidal behaviors.
| Total sample | Ideation | Plan | Attempt | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | SE | % | SE | % | SE | % | SE | |
| Type of adversity | |||||||||
| Parental mental illness | 69 | 4.7 | 0.4 | 12.3 | 2.4 | 11.1 | 5.0 | 21.1 | 8.0 |
| Parental substance misuse | 35 | 1.9 | 0.9 | 5.1 | 2.1 | 11.9 | 4.7 | 9.4 | 6.5 |
| Parental criminality | 12 | 1.0 | 0.5 | 0.8 | 0.6 | 0.4 | 0.4 | 0.8 | 0.7 |
| Family violence | 85 | 4.9 | 0.7 | 7.4 | 2.0 | 9.9 | 3.9 | 4.8 | 4.0 |
| Physical abuse | 79 | 5.4 | 0.7 | 11.4 | 1.6 | 10.4 | 3.4 | 24.5 | 6.0 |
| Sexual abuse | 13 | 0.7 | 0.2 | 3.5 | 1.1 | 6.0 | 3.5 | 5.3 | 5.2 |
| Neglect | 41 | 2.8 | 0.4 | 5.5 | 1.7 | 4.6 | 3.3 | 8.5 | 5.3 |
| Parental death | 55 | 2.8 | 0.5 | 5.6 | 2.1 | 6.4 | 4.4 | 10.0 | 7.8 |
| Parental divorce | 14 | 1.1 | 0.4 | 1.8 | 1.5 | 4.7 | 4.2 | 3.8 | 4.4 |
| Other parental loss | 26 | 1.5 | 0.3 | 3.1 | 1.1 | 0.0 | 0.0 | ||
| Serious physical illness | 39 | 2.4 | 0.5 | 3.7 | 2.5 | 4.5 | 1.5 | 2.8 | 2.6 |
| Family economic adversity | 13 | 0.8 | 0.3 | 0.0 | 0.0 | 0.0 | |||
| Number of childhood adversities | |||||||||
| 0 | 1114 | 77.9 | 1.3 | 63.2 | 3.8 | 51.6 | 5.6 | 46.3 | 7.7 |
| 1 | 253 | 16.6 | 1.1 | 21.7 | 4.2 | 31.1 | 6.2 | 24.0 | 10.3 |
| 2+ | 92 | 5.5 | 1.1 | 15.1 | 2.8 | 17.2 | 5.1 | 29.7 | 10.5 |
| Among ideators | ||||||||
|---|---|---|---|---|---|---|---|---|
| Plan | Attempt | Unplanned attempt | Planned attempt | |||||
| % | SE | % | SE | % | SE | % | SE | |
| Type of adversity | ||||||||
| Parental mental illness | 11.1 | 5.0 | 21.1 | 8.0 | 9.1 | 11.2 | 22.3 | 8.8 |
| Parental Substance misuse | 11.9 | 4.7 | 9.4 | 6.5 | 0.0 | 10.3 | 6.6 | |
| Parental criminality | 0.4 | 0.4 | 0.8 | 0.7 | 0.0 | 0.9 | 0.7 | |
| Family violence | 9.9 | 3.9 | 4.8 | 4.0 | 0.0 | 5.3 | 4.4 | |
| Physical abuse | 10.4 | 3.4 | 24.5 | 6.0 | 100.0 | 17.3 | 6.0 | |
| Sexual abuse | 6.0 | 3.5 | 5.3 | 5.2 | 0.0 | 5.8 | 5.7 | |
| Neglect | 4.6 | 3.3 | 8.5 | 5.3 | 0.0 | 9.3 | 6.1 | |
| Parental death | 6.4 | 4.4 | 10.0 | 7.8 | 0.0 | 10.9 | 8.5 | |
| Parental divorce | 4.7 | 4.2 | 3.8 | 4.4 | 0.0 | 4.2 | 4.9 | |
| Other parental loss | 0.0 | 0.0 | 0.0 | 0.0 | ||||
| Serious physical illness | 4.5 | 1.5 | 2.8 | 2.6 | 0.0 | 3.1 | 2.8 | |
| Family economic adversity | 0.0 | 0.0 | 0.0 | 0.0 | ||||
| Number of childhood adversities | ||||||||
| 0 | 51.6 | 5.6 | 46.3 | 7.7 | 0.0 | 50.7 | 8.3 | |
| 1 | 31.1 | 6.2 | 24.0 | 10.3 | 90.9 | 11.2 | 17.6 | 9.0 |
| 2+ | 17.2 | 5.1 | 29.7 | 10.5 | 9.1 | 11.2 | 31.7 | 10.9 |
SE: standard error.
Weighted percentages.
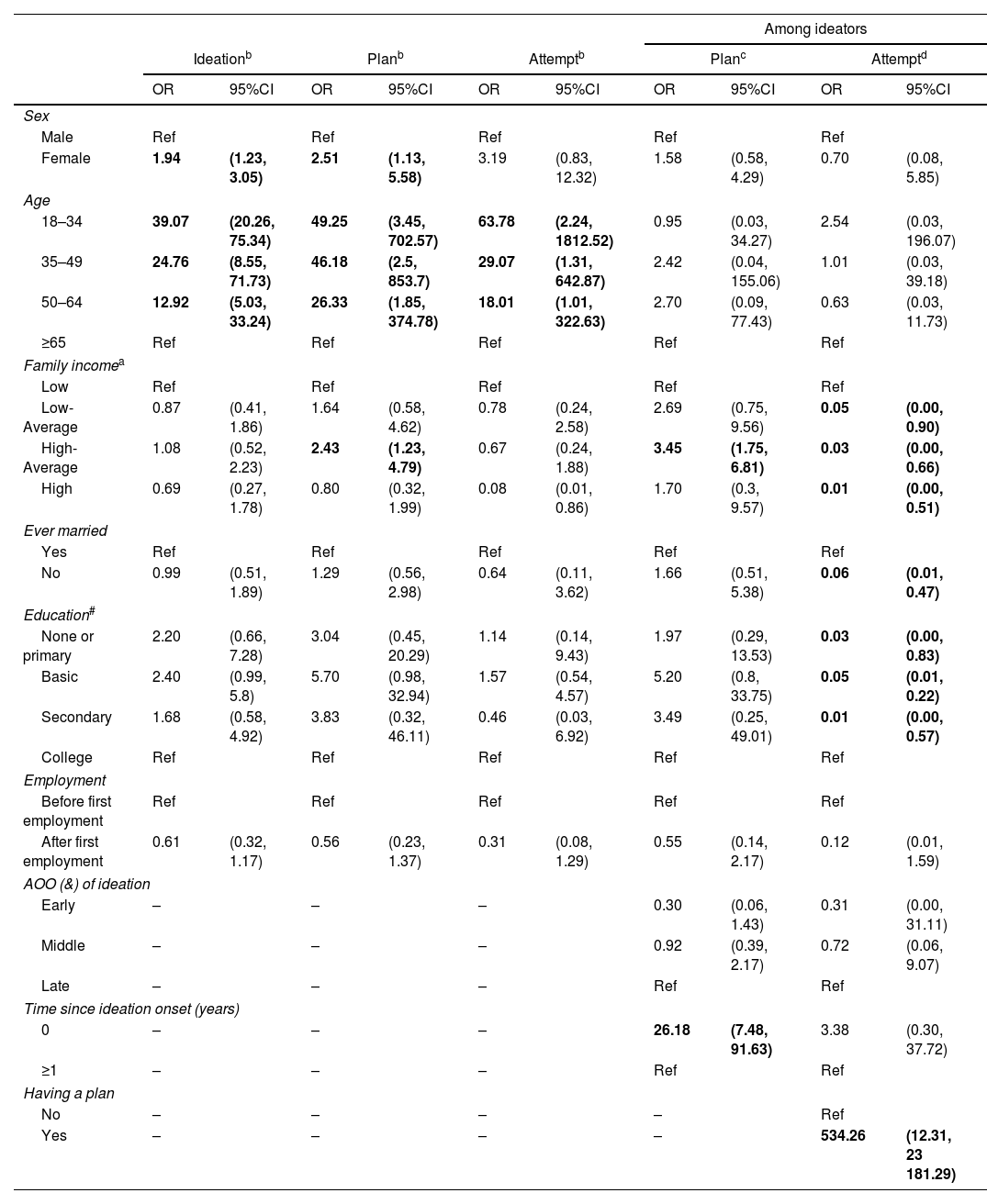
Females had significantly higher odds than males of suicidal ideation and planning, although there were no differences regarding attempts (Table 3). Younger people (aged 18–34 years) had consistently higher odds of ideation, planning, and attempts as compared to those≥65 years. Participants with high-average family income had significant higher risk of suicidal planning than the reference group (low family income). There was no significant association with other sociodemographic variables. Mean (SD) age of onset of suicidal ideation, planning, and attempt was 36.9 (17), 37.1 (13.4) and 37.5 (14.6) years, respectively. Age of onset of ideation was not associated with increased risk of subsequent suicidal plan or attempt. However, the risk of experiencing suicidal planning was found to be higher within the first year after the suicidal ideation onset. Having a plan significantly increased the risk of making a suicide attempt.
Multivariate logistic regression for sociodemographic risk factors for first onset of suicidal behaviors in Murcia (Spain).
| Among ideators | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ideationb | Planb | Attemptb | Planc | Attemptd | ||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Sex | ||||||||||
| Male | Ref | Ref | Ref | Ref | Ref | |||||
| Female | 1.94 | (1.23, 3.05) | 2.51 | (1.13, 5.58) | 3.19 | (0.83, 12.32) | 1.58 | (0.58, 4.29) | 0.70 | (0.08, 5.85) |
| Age | ||||||||||
| 18–34 | 39.07 | (20.26, 75.34) | 49.25 | (3.45, 702.57) | 63.78 | (2.24, 1812.52) | 0.95 | (0.03, 34.27) | 2.54 | (0.03, 196.07) |
| 35–49 | 24.76 | (8.55, 71.73) | 46.18 | (2.5, 853.7) | 29.07 | (1.31, 642.87) | 2.42 | (0.04, 155.06) | 1.01 | (0.03, 39.18) |
| 50–64 | 12.92 | (5.03, 33.24) | 26.33 | (1.85, 374.78) | 18.01 | (1.01, 322.63) | 2.70 | (0.09, 77.43) | 0.63 | (0.03, 11.73) |
| ≥65 | Ref | Ref | Ref | Ref | Ref | |||||
| Family incomea | ||||||||||
| Low | Ref | Ref | Ref | Ref | Ref | |||||
| Low-Average | 0.87 | (0.41, 1.86) | 1.64 | (0.58, 4.62) | 0.78 | (0.24, 2.58) | 2.69 | (0.75, 9.56) | 0.05 | (0.00, 0.90) |
| High-Average | 1.08 | (0.52, 2.23) | 2.43 | (1.23, 4.79) | 0.67 | (0.24, 1.88) | 3.45 | (1.75, 6.81) | 0.03 | (0.00, 0.66) |
| High | 0.69 | (0.27, 1.78) | 0.80 | (0.32, 1.99) | 0.08 | (0.01, 0.86) | 1.70 | (0.3, 9.57) | 0.01 | (0.00, 0.51) |
| Ever married | ||||||||||
| Yes | Ref | Ref | Ref | Ref | Ref | |||||
| No | 0.99 | (0.51, 1.89) | 1.29 | (0.56, 2.98) | 0.64 | (0.11, 3.62) | 1.66 | (0.51, 5.38) | 0.06 | (0.01, 0.47) |
| Education# | ||||||||||
| None or primary | 2.20 | (0.66, 7.28) | 3.04 | (0.45, 20.29) | 1.14 | (0.14, 9.43) | 1.97 | (0.29, 13.53) | 0.03 | (0.00, 0.83) |
| Basic | 2.40 | (0.99, 5.8) | 5.70 | (0.98, 32.94) | 1.57 | (0.54, 4.57) | 5.20 | (0.8, 33.75) | 0.05 | (0.01, 0.22) |
| Secondary | 1.68 | (0.58, 4.92) | 3.83 | (0.32, 46.11) | 0.46 | (0.03, 6.92) | 3.49 | (0.25, 49.01) | 0.01 | (0.00, 0.57) |
| College | Ref | Ref | Ref | Ref | Ref | |||||
| Employment | ||||||||||
| Before first employment | Ref | Ref | Ref | Ref | Ref | |||||
| After first employment | 0.61 | (0.32, 1.17) | 0.56 | (0.23, 1.37) | 0.31 | (0.08, 1.29) | 0.55 | (0.14, 2.17) | 0.12 | (0.01, 1.59) |
| AOO (&) of ideation | ||||||||||
| Early | – | – | – | 0.30 | (0.06, 1.43) | 0.31 | (0.00, 31.11) | |||
| Middle | – | – | – | 0.92 | (0.39, 2.17) | 0.72 | (0.06, 9.07) | |||
| Late | – | – | – | Ref | Ref | |||||
| Time since ideation onset (years) | ||||||||||
| 0 | – | – | – | 26.18 | (7.48, 91.63) | 3.38 | (0.30, 37.72) | |||
| ≥1 | – | – | – | Ref | Ref | |||||
| Having a plan | ||||||||||
| No | – | – | – | – | Ref | |||||
| Yes | – | – | – | – | 534.26 | (12.31, 23 181.29) | ||||
Family income is defined as a four-category income scale calculated as the ratio of family income in the past 12 months divided by the median income for Spain. Low income is defined as less than or equal to 0.5, low average as 0.5–1.0, high average as 1.0–2.0, and high as over 2.0; # Completed years of education (four categories: None or primary: 0–7 years; Basic: 8-11 years; Secondary: 12–15 years and College: 16 or more years of education); & AOO: Age of onset.
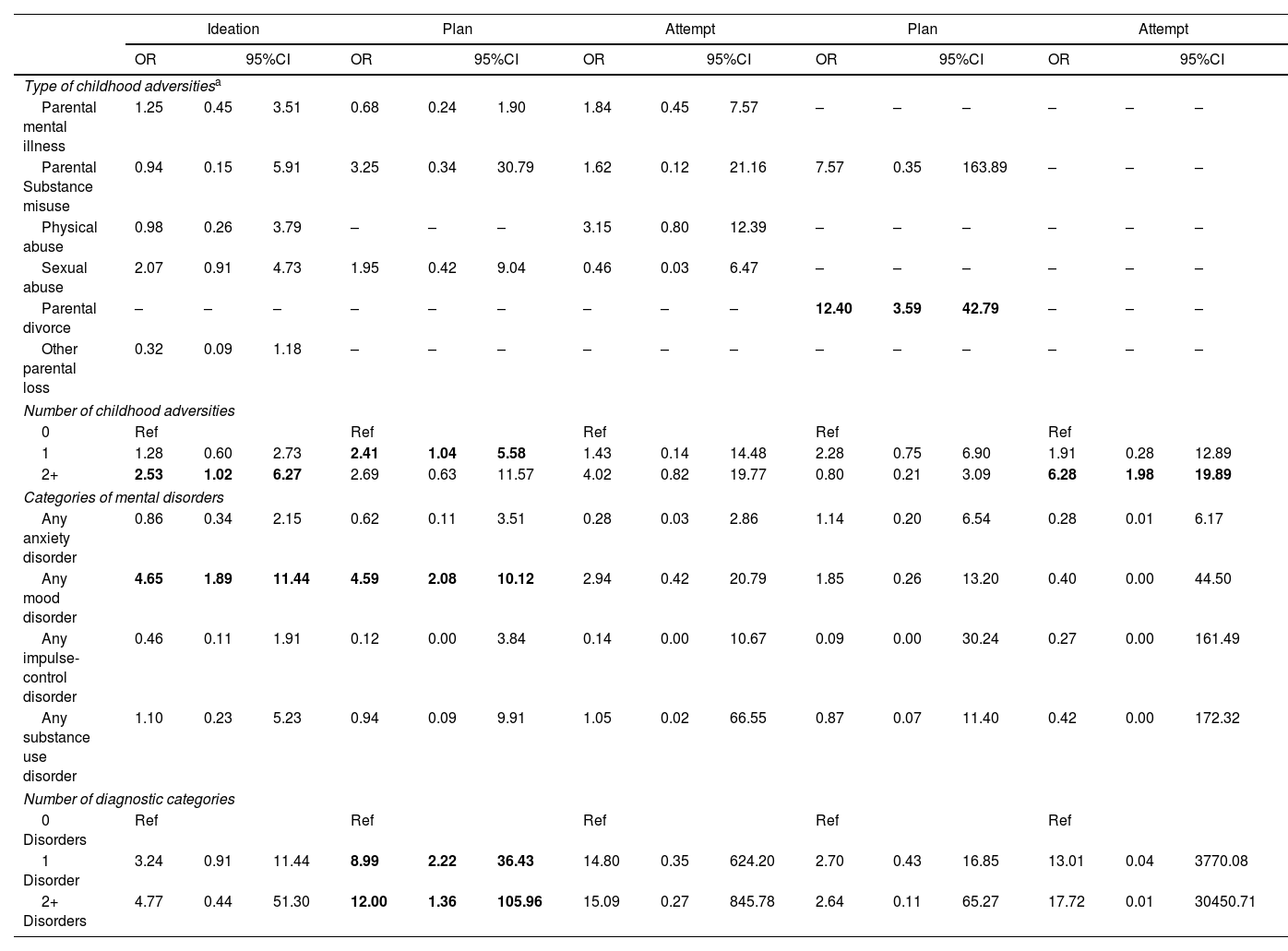
As described in Table 4, any childhood adversity was a risk factor of suicidal planning and in those with an attempt among ideators in the multivariate model. None of the individual childhood adversities were significant except parental divorce as a risk factor of the transition from ideation to suicidal plan. The number of childhood adversities showed a consistent dose-response trend. A similar pattern was found with the precedent of any lifetime mental disorder associated with a significant increased risk of ideation and planning, mainly due to mood disorders. The number of prior mental disorders was associated with ideation and suicidal planning in a dose-response relationship when adjusted to sociodemographic variables (Suppl Table 3).
Childhood adversities and diagnostic categories as risk factors for first onset of suicidal behaviors in Murcia (Spain).
| Ideation | Plan | Attempt | Plan | Attempt | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | ||||||
| Type of childhood adversitiesa | |||||||||||||||
| Parental mental illness | 1.25 | 0.45 | 3.51 | 0.68 | 0.24 | 1.90 | 1.84 | 0.45 | 7.57 | – | – | – | – | – | – |
| Parental Substance misuse | 0.94 | 0.15 | 5.91 | 3.25 | 0.34 | 30.79 | 1.62 | 0.12 | 21.16 | 7.57 | 0.35 | 163.89 | – | – | – |
| Physical abuse | 0.98 | 0.26 | 3.79 | – | – | – | 3.15 | 0.80 | 12.39 | – | – | – | – | – | – |
| Sexual abuse | 2.07 | 0.91 | 4.73 | 1.95 | 0.42 | 9.04 | 0.46 | 0.03 | 6.47 | – | – | – | – | – | – |
| Parental divorce | – | – | – | – | – | – | – | – | – | 12.40 | 3.59 | 42.79 | – | – | – |
| Other parental loss | 0.32 | 0.09 | 1.18 | – | – | – | – | – | – | – | – | – | – | – | – |
| Number of childhood adversities | |||||||||||||||
| 0 | Ref | Ref | Ref | Ref | Ref | ||||||||||
| 1 | 1.28 | 0.60 | 2.73 | 2.41 | 1.04 | 5.58 | 1.43 | 0.14 | 14.48 | 2.28 | 0.75 | 6.90 | 1.91 | 0.28 | 12.89 |
| 2+ | 2.53 | 1.02 | 6.27 | 2.69 | 0.63 | 11.57 | 4.02 | 0.82 | 19.77 | 0.80 | 0.21 | 3.09 | 6.28 | 1.98 | 19.89 |
| Categories of mental disorders | |||||||||||||||
| Any anxiety disorder | 0.86 | 0.34 | 2.15 | 0.62 | 0.11 | 3.51 | 0.28 | 0.03 | 2.86 | 1.14 | 0.20 | 6.54 | 0.28 | 0.01 | 6.17 |
| Any mood disorder | 4.65 | 1.89 | 11.44 | 4.59 | 2.08 | 10.12 | 2.94 | 0.42 | 20.79 | 1.85 | 0.26 | 13.20 | 0.40 | 0.00 | 44.50 |
| Any impulse-control disorder | 0.46 | 0.11 | 1.91 | 0.12 | 0.00 | 3.84 | 0.14 | 0.00 | 10.67 | 0.09 | 0.00 | 30.24 | 0.27 | 0.00 | 161.49 |
| Any substance use disorder | 1.10 | 0.23 | 5.23 | 0.94 | 0.09 | 9.91 | 1.05 | 0.02 | 66.55 | 0.87 | 0.07 | 11.40 | 0.42 | 0.00 | 172.32 |
| Number of diagnostic categories | |||||||||||||||
| 0 Disorders | Ref | Ref | Ref | Ref | Ref | ||||||||||
| 1 Disorder | 3.24 | 0.91 | 11.44 | 8.99 | 2.22 | 36.43 | 14.80 | 0.35 | 624.20 | 2.70 | 0.43 | 16.85 | 13.01 | 0.04 | 3770.08 |
| 2+ Disorders | 4.77 | 0.44 | 51.30 | 12.00 | 1.36 | 105.96 | 15.09 | 0.27 | 845.78 | 2.64 | 0.11 | 65.27 | 17.72 | 0.01 | 30450.71 |
Multivariate logistic regression with suicidal behaviors as the dependent variable and type and number of childhood adversities, number and diagnostic categories adjusted by sociodemographic variables. p<0.05 (in bold text).
Only those type of childhood adversities with a 95%CI not including the value 1 in Suppl Table 2 were entered in the model within each suicidal behavior as the dependent variable in multivariate logistic.
Lifetime prevalence of suicidal ideation in Murcia was higher (8.0%; 95%CI: 5.8, 11.0) than previous Spanish studies (ESEMeD: 4.4%; 3.6, 5.07 and COURAGE: 3.7%; 2.8, 4.510), but similar to other European countries (7.8%; 7.3, 8.3).27 However, lifetime prevalence of suicidal planning (2.1%; 1.5, 3.0) and attempt (1.1%; 0.8, 1.7) were similar to the Spanish studies, with overlapping confidence intervals7,10,27 but suicide attempt was lower than that reported internationally (2.7%; 2.6, 2.9).6 A similar pattern has been described in both previous Spanish surveys.7,10 The PEGASUS-Murcia project was conducted between 2010-12, in the middle of an economic crisis,17 the same period of time (2011–2012) as the latest Spanish survey10 and ten years after other national and international surveys with similar methodology had been carried out.6,7,27 However, differences between Spanish provinces might partially explain the differences described for suicidal behavior, as they have been previously described with regard to suicidal rates.2
Being female and a younger age increased the risk of suicidal behavior consistent with other national and international surveys.6,7,10,27,28 The significant association of family income with suicide plan and with transition among ideators was unexpected as there is a general consensus of the effect of poverty at an individual level.29 However, this result should be interpreted with caution as it did not reflect the income level at the time of the non-fatal suicide behavior but the income level in the previous year when the participant was interviewed. The first year after ideation onset had the highest risk of transition from ideation to a plan and an attempt. This finding is consistent cross-nationally4,6,9,30 and suggests a narrow window of opportunity for preventive intervention programs after the onset of suicidal ideation, especially for those having a plan of suicide.
Childhood adversities increased the risk of a suicidal thoughts and behavior, even when controlling for sociodemographic variables and lifetime mental disorders. These results are consistent with prior studies.12,13,31,32 Parental divorce increased the risk of transition from suicidal ideation to plan in our sample. Parental divorce during childhood has been described as an important risk factor for the onset and persistence of suicidal behaviour,33 specially related to suicide attempt in young adulthood.34 This risk of parental divorce seem to be higher combined with a parent with alcohol abuse.35 It is noteworthy that, in our sample, sexual abuse was not associated with suicidality in our multivariate analysis. Similar results have been described.36,37 However, it has been consistently described as one of the most important predictor.12,13,31,38 The relatively low prevalence of sexual abuse described in our sample (0.7%) might have produced an unreliable result. Results suggest a dose-response relationship with numbers of childhood adversities with suicidal ideation, plan and transition to an attempt among ideators, but low frequencies of exposure to individual childhood adversities limit our statistical power to detect significant associations.
While anxiety and mood disorders were associated to all three suicidal behaviors and substance disorders to suicidal ideation in bivariate analysis, only lifetime prevalence of depressive disorders prior to age of onset of suicidal behavior was associated with suicidal ideation or planning in our sample in the multivariate model controlling for comorbidity. Furthermore, the number of diagnostic categories was significantly associated in a dose-response relationship with suicidal behavior, though only reached statistical significance for suicidal planning. Each mental disorder has been described as a significant predictor of a subsequent suicidal behavior,6,7,10,27 but mood disorders are considered among the strongest.11 A similar pattern has been described where association found in bivariate analyses decreased substantially in multivariate analyses controlling for comorbidity, although remained significant.39 A possible explanation for this pattern might be that comorbidity might explain some of the associations.
Similarities in the main characteristics of the design of the study (e.g. representativeness from general population, the diagnostic instrument and methods of analysis) with other national and international surveys in the context of the WMH surveys6,7,27 enables national and international comparisons overcoming heterogeneity across studies.1,40 Nevertheless, our results should be interpreted within caution in the context of some limitations. First, PEGASUS-Murcia project obtained a response rate of 67.4%. Though not entirely satisfactory, it was above the conventionally 60% considered as a minimum standard,41 was above the overall participation rate of other European countries participating in the previous ESEMeD project,42 and participants in this survey were comparable to census data from the general population of Murcia suggesting the representativeness of the final sample.17 However, it is conceivable that some persons with mental disorders may have refused to participate to a larger extent than the general sample, so that our results may in fact underestimate the actual prevalence of suicidal behaviors in the population. Secondly, suicidal behaviors were assessed by retrospective self-report leading to a possible under-reporting and biased recall. However, several systematic reviews have shown that adults are able to recall past experiences with sufficient accuracy to provide valuable information.43,44 Thirdly, the low prevalence of non-fatal suicide behaviors identified may have underpowered the study to detect associated factors and interactions, so that the 95% range of the CI should have to be interpreted with caution. Fourthly, schizophrenia and other non-affective psychoses were not initially included as a diagnosis in the CIDI as they tended to be overestimated in lay-administered interviews in previous validation studies.45,46 Besides, these studies also suggest that the vast majority of respondents with clinician-diagnosed non-affective psychoses would be captured as cases because they would also meet the criteria for CIDI anxiety, mood, or substance disorders. Finally, the cross-sectional design while allowing association studies, limits the possible causal interpretation of the findings.
This survey adds new evidence highlighting the importance of a careful evaluation of mental disorders and the exposure to childhood adversities to prevent suicidal behavior. Comprehensive suicide prevention programs should not only focus on proximal risk factors, such as detection of mental disorders, but should also include the careful evaluation of distal risk factors, such as having been exposed to adversities during the childhood. The causes of a suicidal behavior are still not fully understood but it is accepted that this behavior is the result of complex interactions between numerous factors that are difficult to address in a unique study.47 Other research strategies have been suggested to go beyond the examination of sociodemographic and psychiatric risk factors, for example, in the context of the Research Domain Criteria (RDoC) framework,48 but it will take time and interdisciplinary approaches between different specialties to clarify the knowledge of the processes involved in suicide in the near future and to improve our ability to predict and prevent suicidal behavior and suicide deaths. Meanwhile additional studies are needed to identify risk and protective factors influencing such behaviors, especially if they are designed in areas where decision makers need epidemiological data to implement mental health care planning.15 This situation is particularly important in Spain16 where there is still no national prevention program against suicide.49
In conclusion, based on the first epidemiological survey on a representative sample of the general population of the region of Murcia, lifetime prevalence of suicide ideation is higher than national estimates while lifetime prevalence of suicidal planning and attempt remains similar to national estimates. Childhood adversities and mental disorders, especially mood disorders, are consistent risk factors for suicidality. Population prevention programs should focus on interventions to prevent adversities during childhood, the early detection of mental disorders, especially mood disorders, and in those individuals with suicidal thoughts.
Data sharing statementPublic access to the diagnostic instrument, including diagnostic algorithms, should be submitted to: http://www.hcp.med.harvard.edu/wmh. However, there are limitations on the availability of raw data due to ethical restrictions related to the signed consent agreements and to the signed agreement with the WHO World Mental Health Survey Initiative to limit comparative analyses to those carried out within the consortium. Requestors wishing to access a de-identified minimal dataset necessary for the purpose of monitoring our published analyses only, can apply to the principal investigator of the PEGASUS-Murcia Project, Fernando Navarro-Mateu (email: Fernando.navarro@carm.es).
Authors’ contributionsConceptualization FNM DS CN SM MH MN RCK JA. Methodology: FNM DS CN SM JH MH MN RCK JA. Analysis: DS GV MB FNM. Funding acquisition: FNM CN and JA. Resources: FNM CN MDC JA SM RCK. Writing and editing: FNM DS JH MH MN RCK JA. All authors reviewed and approved the final manuscript.
Funding sourceThe direct and indirect funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interestRCK has served on advisory boards for Mensante Corporation, Plus One Health Management, Lake Nona Institute and US Preventive Medicine, is a co-owner of DataStat. In the past three years, RCK has been a consultant for Hoffman-La Roche, Johnson & Johnson Wellness and Prevention, and Groupe Sanofi-Aventis. There are no patents, products in development or marketed products to declare. FNM reports punctual non-financial support from Otsuka outside the submitted work in 2019.
The authors wish to thank all participants for their collaboration. The PEGASUS-Murcia Project was supported by the Regional Health Authorities of Murcia (“Servicio Murciano de Salud and Consejería de Sanidad y Política Social”) (Decreto n° 455/2009), and the “Ayudas para proyectos de Investigación en Salud – ISCIII – del Plan Nacional de Investigación Científica, Desarrollo e Innovación Tecnológica” (PI12/00809). The authors thank the WMH Coordinating Center staff at Harvard and Michigan Universities for their assistance with the instrumentation, fieldwork and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884); the John D. and Catherine T. MacArthur Foundation; the Pfizer Foundation, the U.S. Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558); the Fogarty International Center (FIRCA R03-TW006481); the Pan American Health Organization; the Eli Lilly & Company Foundation; Ortho-McNeil Pharmaceutical, Inc.; GlaxoSmithKline; Bristol-Myers Squibb and Shire. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.