Cognitive models suggest the co-occurrence of cognitive biases and aberrant salience is unique to psychosis, but their interaction is not yet fully understood. Therefore, we aimed to elucidate the relationship between subjective cognitive biases and aberrant salience in individuals with schizophrenia spectrum disorders (SSDs) in this study.
MethodsA sample of 92 subjects with SSDs underwent an assessment using Davos Assessment Cognitive Biases (DACOBS) and the Aberrant Salience Inventory (ASI) in a cross-sectional design. We evaluated psychopathological differences based on ASI scores and conducted a linear regression analysis to examine the variables associated with aberrant salience.
ResultsSubjects with an ASI score ≥14 demonstrated significantly higher scores across all subscales and total score of ASI and DACOBS (p<0.001). ASI subscales were significantly positive correlated with all DACOBS subscales, ranging from 0.250 for Increased Significance and Safety Behavior to 0.679 for Heightened Emotionality and Social cognition problems. The linear regression analysis revealed a positive association between aberrant salience and the DACOBS subscales jumping to conclusions (JTC) (β=0.220), social cognition problems (β=0.442), subjective cognitive problems (β=0.405), and a negative association with the subscale belief inflexibility (β=−0.350).
ConclusionsOur findings suggest that JTC, social cognition problems and subjective cognitive problems may play a central role in the experience of aberrant salience in individuals with SSDs. This work informs about the need of developing prevention and intervention strategies that specifically target cognitive biases and aberrant salience in the treatment of psychosis.
Schizophrenia (SCZ) is a psychiatric disease characterized by positive and negative symptoms, cognitive impairments, disorganized behavior and/or speech, and mostly by social, functional and occupational impairments, with a complex and still not fully understood etiology.1 Prognosis is varied and influenced by a number of factors, and may include recovery in 24.2% of cases.2
Cognitive biases refer to systematic errors in both cognitive content (i.e., meaning) and processing (i.e., processing of meaning) across specific contexts and situations,3 and are considered to play a relevant mediating role in the transition to delusions in individuals affected by schizophrenia spectrum disorders (SSDs).4
Several meta-analyses have found that individuals with psychosis exhibit a greater tendency to make hasty decisions, also known as jumping to conclusions (JTC), more frequently than healthy controls.5 Subjects with SCZ6 often demonstrate rigid beliefs and may confuse internally generated thoughts with external sensory stimuli, a cognitive error referred to as externalizing bias.7 The relationship between cognitive biases and the development and persistence of psychotic symptoms is supported by research.8 According to cognitive models of psychosis, the interaction between psychological mechanisms and biological processes may lead to clinical psychosis. The theorized combination of cognitive biases and aberrant salience would be specific to psychosis.9
Studies have shown that sensitivity to stress, aberrant salience and the cognitive bias of threat anticipation play a crucial role in the development of psychotic experiences, with the salience operating before the onset of psychosis, while threat anticipation occurs during the transition from subclinical psychosis to a psychotic disorder.10 According to this model, cognitive biases lead to an impaired interpretation of aberrant salience experiences, (i.e. those phenomena of anomalous sensory experiences) and negative events that need an explanation.11 Therefore, the clinical manifestation of psychosis would be the consequence of the occurrence of aberrant salience and cognitive biases.12
The aim of the present study was to test the relationship between subjective cognitive biases and aberrant salience as measured by the Aberrant Salience Inventory (ASI).13 To our knowledge indeed, there has been no exploration of the hypothesis linking subjective cognitive biases, as measured by the Davos Assessment of Cognitive Biases Scale (DACOBS) and aberrant salience in persons with SSDs.
Based on previous work on a combination of aberrant salience and cognitive biases in psychosis,9 we assume that (I) individuals with a higher level of aberrant salience may show more severe cognitive biases; (II) there may be an association between aberrant salience and the different cognitive biases assessed. Therefore, the current study purpose is to further clarify the association between cognitive biases and aberrant salience in a real-world clinical setting enrolling a sample of individuals referring to the local unit for an evaluation and subsequent diagnosis of SSDs without selective selections for research purposes.
Materials and methodsParticipants and procedureA total sample of 109 subjects, aged 18–65 years, was enrolled among consecutive individuals referred to the outpatients Psychiatry Unit of the University Hospital of Catanzaro (Italy) for an evaluation and who had received care for SCZ or schizoaffective disorder. A dedicated room within the unit was used to fill in the questionnaires and collect clinical and anamnestic data. Completing the questionnaires took about 20–30min.
Clinical diagnosis was run according to DSM-5 criteria14 and using the Structured Clinical Interview for DSM-5 (SCID-5)15 by experienced psychiatrists trained in administration of neuropsychiatric tests. Participants had been admitted to the unit for at least twelve consecutive months.
Participants were excluded if fulfilling any of the following criteria: (1) diagnosis of neurocognitive disorder, intellectual disability, or other serious medical condition associated with secondary psychiatric symptoms that potentially affect the assessment or lead to missed responses due to poor understanding of the questions asked; (2) diagnosis of substance use disorder within the past six months, as active substance use affects the correct assessment of aberrant salience13; (3) inability to complete the assessment due to conditions such as speech impairments or a lack of knowledge of the Italian language that potentially affect the assessment or lead to missed responses due to poor understanding of the questions asked; and (4) invalid informed consent to the study procedures.
The study was carried out in accordance with the latest version of the Declaration of Helsinki16 and was approved by the Ethics Committee of the University of Catanzaro (ID number 191/2020). All participants signed a written informed consent according to the ethical committee's guidelines before any data was collected.
Out of the 123 subjects initially approached for the study, 14 declined participation in the study or refused to complete the assessment and were therefore excluded from the analysis, and 17 were excluded during the screening phase or enrolment due to the following reasons: eight individuals (7.5%) were not eligible because they received a diagnosis of active substance use disorder after enrolment and previously undiagnosed; five (4.7%) dropped out before the end of the assessment and thus were excluded from the study; and four (3.7%) met the exclusion criteria of intellectual disability. Questionnaires not completed in all items (dropout) were stored in a locked place associated exclusively with a unique ID.
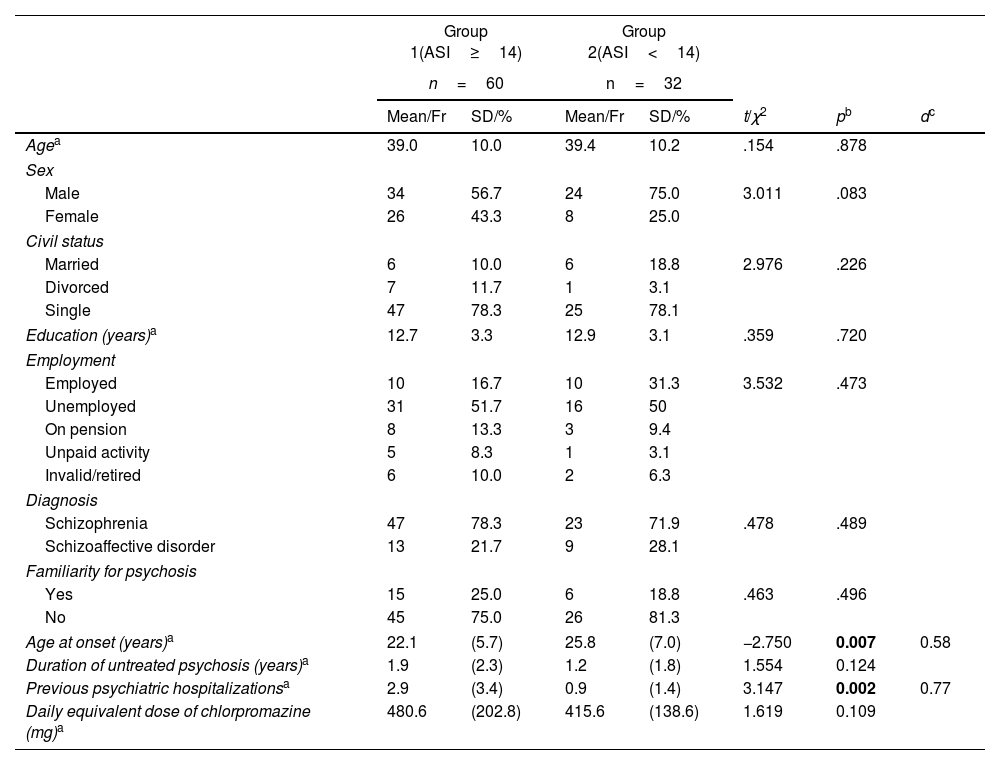
Thus, the final sample consisted of 92 participants (dropout rate 5.2%), 70 diagnosed with SCZ, and 22 diagnosed with schizoaffective disorder. Demographic and clinical characteristics of the sample are presented in Table 1.
Comparisons of socio-demographic and clinical characteristics of the sample according to the aberrant salience.
| Group 1(ASI≥14) | Group 2(ASI<14) | ||||||
|---|---|---|---|---|---|---|---|
| n=60 | n=32 | ||||||
| Mean/Fr | SD/% | Mean/Fr | SD/% | t/χ2 | pb | dc | |
| Agea | 39.0 | 10.0 | 39.4 | 10.2 | .154 | .878 | |
| Sex | |||||||
| Male | 34 | 56.7 | 24 | 75.0 | 3.011 | .083 | |
| Female | 26 | 43.3 | 8 | 25.0 | |||
| Civil status | |||||||
| Married | 6 | 10.0 | 6 | 18.8 | 2.976 | .226 | |
| Divorced | 7 | 11.7 | 1 | 3.1 | |||
| Single | 47 | 78.3 | 25 | 78.1 | |||
| Education (years)a | 12.7 | 3.3 | 12.9 | 3.1 | .359 | .720 | |
| Employment | |||||||
| Employed | 10 | 16.7 | 10 | 31.3 | 3.532 | .473 | |
| Unemployed | 31 | 51.7 | 16 | 50 | |||
| On pension | 8 | 13.3 | 3 | 9.4 | |||
| Unpaid activity | 5 | 8.3 | 1 | 3.1 | |||
| Invalid/retired | 6 | 10.0 | 2 | 6.3 | |||
| Diagnosis | |||||||
| Schizophrenia | 47 | 78.3 | 23 | 71.9 | .478 | .489 | |
| Schizoaffective disorder | 13 | 21.7 | 9 | 28.1 | |||
| Familiarity for psychosis | |||||||
| Yes | 15 | 25.0 | 6 | 18.8 | .463 | .496 | |
| No | 45 | 75.0 | 26 | 81.3 | |||
| Age at onset (years)a | 22.1 | (5.7) | 25.8 | (7.0) | −2.750 | 0.007 | 0.58 |
| Duration of untreated psychosis (years)a | 1.9 | (2.3) | 1.2 | (1.8) | 1.554 | 0.124 | |
| Previous psychiatric hospitalizationsa | 2.9 | (3.4) | 0.9 | (1.4) | 3.147 | 0.002 | 0.77 |
| Daily equivalent dose of chlorpromazine (mg)a | 480.6 | (202.8) | 415.6 | (138.6) | 1.619 | 0.109 | |
ASI: Aberrant Salience Inventory; DACOBS: Davos Assessment of Cognitive Biases Scale; SD: standard deviation.
An ad hoc schedule was administered in order to assess the demographic and clinical characteristics of the sample. Collected data included ethnicity, civil status, level of education, employment, psychiatric familiarity, age at onset of illness, duration of untreated psychosis (DUP), previous psychiatric hospitalizations and antipsychotic therapy. The daily dose of prescribed antipsychotic drugs was converted to the equivalent daily dose of chlorpromazine, based on the international consensus.17
AssessmentThe Aberrant Salience Inventory (ASI)13 is a self-administered test, consisting of 29 items with a dichotomous yes/no response, that assesses individual aberrant salience and psychotic proneness. Aberrant salience is defined as an over-assignation of salient information to neutral or familiar stimuli.13 The scale investigates the presence of five factors correlated with each other and in line with Kapur's conceptualization: feelings of increased significance (7 items), sense sharpening (5 items), impending understanding (5 items), heightened emotionality (6 items) and heightened cognition (6 items). The experience of aberrant salience is a common experience within the general population; however, a total ASI score of 14 or higher is considered as the cut-off point.13 The Italian version of the ASI18 used in this study confirmed the good psychometric properties of the scale, with gold standard values of internal coherence and stability at retest.
The Davos Assessment Cognitive Biases (DACOBS)19 is made up of 42 Likert type items ranging from 7 (strongly agree) to 1 (strongly disagree) and refers to the last two weeks. The self-report questionnaire specifically aims to measure seven different indexes, namely four cognitive biases: JTC (making hasty decisions without considering alternative explanations), belief inflexibility bias (BIB: difficulty in the capacity of reflecting and modifying own beliefs in the light of reflection), attention to threat bias (ATB: excessive perception of others’ behavior as threatening), and external attribution bias (EAB: tendency to make external attributions of personal failures or negative events to the external world). DACOBS also measures two cognitive limitations: social cognition problems and subjective cognitive problems (i.e., problems in understanding the motives, feelings and thoughts of other people and deficits in attention, memory and executive function), and the avoidance behavior (safety behaviors: actions carried out with the intention of reducing perceived threat).19 The Italian version of DACOBS20 has a good reliability ranged from 0.75 for JTC to 0.89 for safety behavior and discriminating satisfactorily psychosis from healthy controls.
Statistical analysisThe data analysis was performed with the Statistical Package for the Social Science, version 22.0 (SPSS Inc., Chicago, IL) and the data presented as means, standard deviations, frequencies, and percentages. The sample was divided into two groups according to the ASI score 13T-test and chi-square test were used to compare the groups, as appropriate. Additionally, effect size d was calculated for significant results. Values of 0.2, 0.5 and >0.8 can be categorized into small, moderate and large effect size, respectively.21
To identify potential predictors of aberrant salience, a stepwise linear regression model was employed. In our model the independent predictors of the aberrant salience were those variables with significant differences according to ASI cut-off. The independent variables analyzed encompassed cognitive bias, including JTC, BIB, ATB, and EAB, as well as cognitive limitations such as social cognition problems and subjective cognitive problems, and safety behaviors of DACOBS. Additionally, clinical features that were significantly different according to ASI cut-off were put in the regression model. The entry and exit criteria for the model were 0.2 and 0.4, respectively, while the statistical significance level was set at p<0.05.
ResultsAll participants were Caucasian, 64% male and 36% female. Regarding socio-economic status, most were single (78%), with a level of education corresponding to high school (12.7 years) and unemployed (51%).
The sample was divided into two groups according to their ASI score setting the cut-off at 14: Group 1 (ASI≥14; n=60) and Group 2 (ASI<14; n=32). The two groups were homogenous for age, sex, diagnosis, civil status, level of education, employment, and familiarity for psychosis. Significant differences emerged regarding age of onset and psychiatric hospitalizations (Table 1). In fact, Group 1 had a lower age of onset (p=0.007) and a higher number of previous psychiatric hospitalizations (p=0.002). No differences emerged regarding DUP and daily equivalent dose of chlorpromazine.
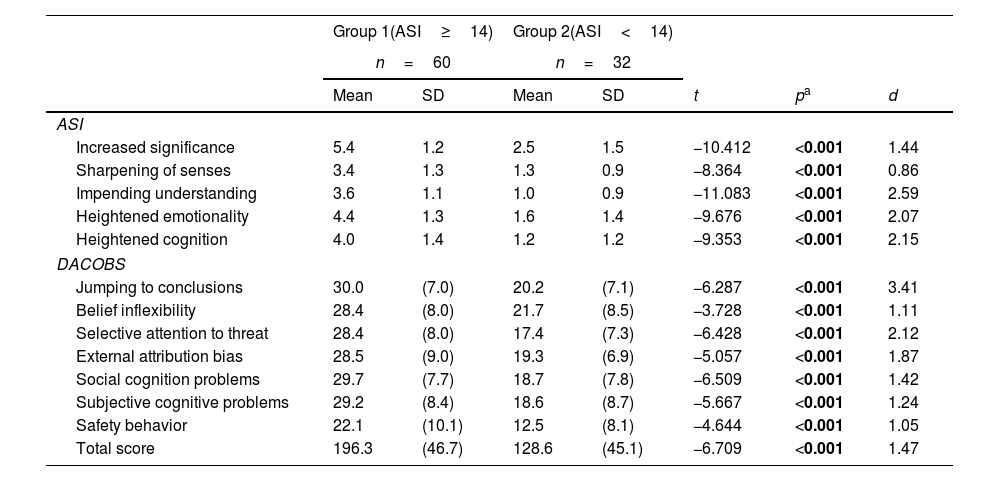
Further, Group 1 showed higher values in all subscales and total score of ASI and DACOBS (p<0.001) (Table 2).
Comparison of clinical characteristics and scores obtained at DACOBS and ASI according to the aberrant salience.
| Group 1(ASI≥14) | Group 2(ASI<14) | ||||||
|---|---|---|---|---|---|---|---|
| n=60 | n=32 | ||||||
| Mean | SD | Mean | SD | t | pa | d | |
| ASI | |||||||
| Increased significance | 5.4 | 1.2 | 2.5 | 1.5 | −10.412 | <0.001 | 1.44 |
| Sharpening of senses | 3.4 | 1.3 | 1.3 | 0.9 | −8.364 | <0.001 | 0.86 |
| Impending understanding | 3.6 | 1.1 | 1.0 | 0.9 | −11.083 | <0.001 | 2.59 |
| Heightened emotionality | 4.4 | 1.3 | 1.6 | 1.4 | −9.676 | <0.001 | 2.07 |
| Heightened cognition | 4.0 | 1.4 | 1.2 | 1.2 | −9.353 | <0.001 | 2.15 |
| DACOBS | |||||||
| Jumping to conclusions | 30.0 | (7.0) | 20.2 | (7.1) | −6.287 | <0.001 | 3.41 |
| Belief inflexibility | 28.4 | (8.0) | 21.7 | (8.5) | −3.728 | <0.001 | 1.11 |
| Selective attention to threat | 28.4 | (8.0) | 17.4 | (7.3) | −6.428 | <0.001 | 2.12 |
| External attribution bias | 28.5 | (9.0) | 19.3 | (6.9) | −5.057 | <0.001 | 1.87 |
| Social cognition problems | 29.7 | (7.7) | 18.7 | (7.8) | −6.509 | <0.001 | 1.42 |
| Subjective cognitive problems | 29.2 | (8.4) | 18.6 | (8.7) | −5.667 | <0.001 | 1.24 |
| Safety behavior | 22.1 | (10.1) | 12.5 | (8.1) | −4.644 | <0.001 | 1.05 |
| Total score | 196.3 | (46.7) | 128.6 | (45.1) | −6.709 | <0.001 | 1.47 |
ASI: Aberrant Salience Inventory; DACOBS: Davos Assessment of Cognitive Biases Scale; SD: standard deviation.
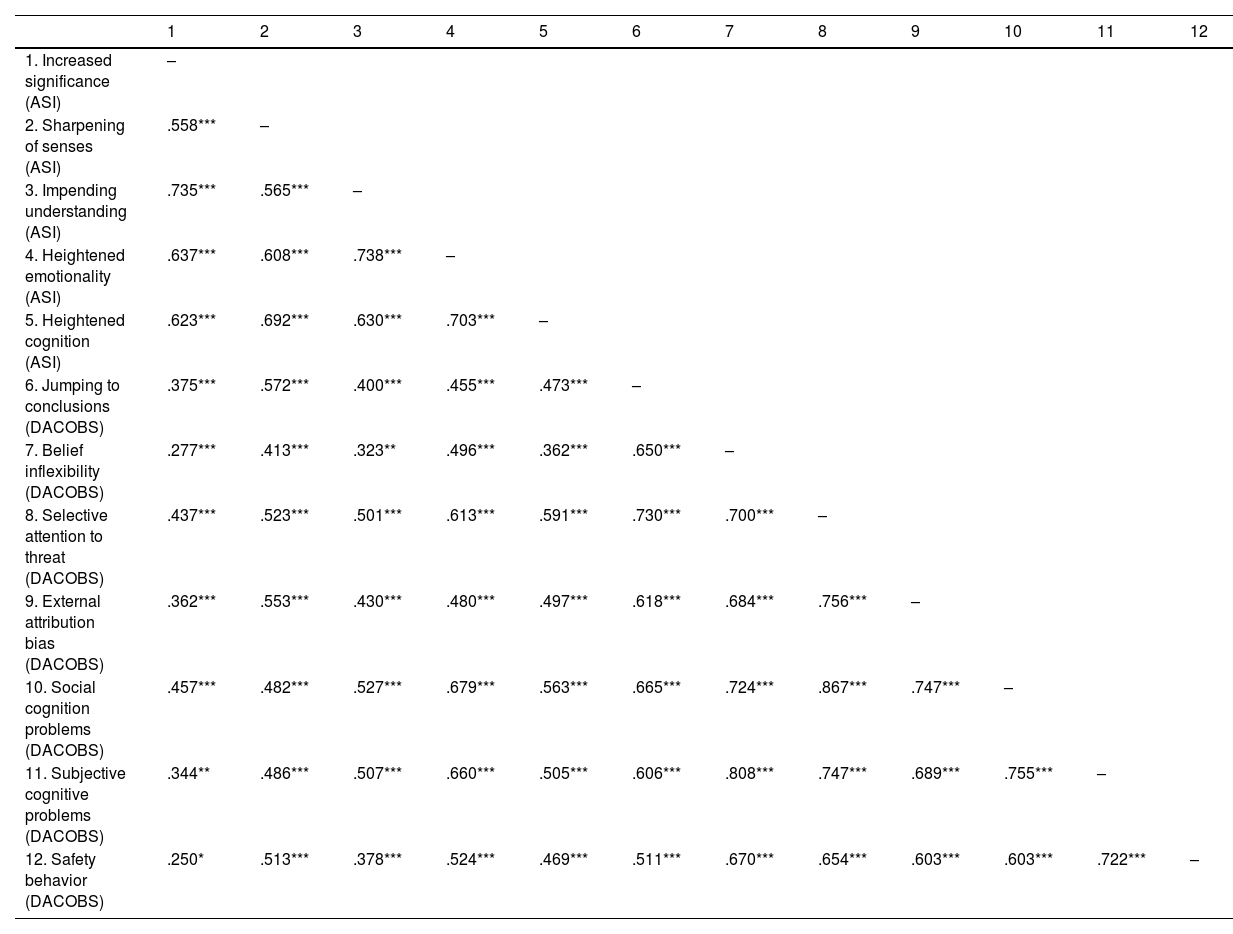
As displayed in Table 3, all ASI subscales were significantly positive correlated with all DACOBS subscales, ranging from 0.250 for Increased Significance and Safety Behavior to 0.679 for Heightened Emotionality and Social cognition problems.
Correlations between ASI and DACOBS scores.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Increased significance (ASI) | – | |||||||||||
| 2. Sharpening of senses (ASI) | .558*** | – | ||||||||||
| 3. Impending understanding (ASI) | .735*** | .565*** | – | |||||||||
| 4. Heightened emotionality (ASI) | .637*** | .608*** | .738*** | – | ||||||||
| 5. Heightened cognition (ASI) | .623*** | .692*** | .630*** | .703*** | – | |||||||
| 6. Jumping to conclusions (DACOBS) | .375*** | .572*** | .400*** | .455*** | .473*** | – | ||||||
| 7. Belief inflexibility (DACOBS) | .277*** | .413*** | .323** | .496*** | .362*** | .650*** | – | |||||
| 8. Selective attention to threat (DACOBS) | .437*** | .523*** | .501*** | .613*** | .591*** | .730*** | .700*** | – | ||||
| 9. External attribution bias (DACOBS) | .362*** | .553*** | .430*** | .480*** | .497*** | .618*** | .684*** | .756*** | – | |||
| 10. Social cognition problems (DACOBS) | .457*** | .482*** | .527*** | .679*** | .563*** | .665*** | .724*** | .867*** | .747*** | – | ||
| 11. Subjective cognitive problems (DACOBS) | .344** | .486*** | .507*** | .660*** | .505*** | .606*** | .808*** | .747*** | .689*** | .755*** | – | |
| 12. Safety behavior (DACOBS) | .250* | .513*** | .378*** | .524*** | .469*** | .511*** | .670*** | .654*** | .603*** | .603*** | .722*** | – |
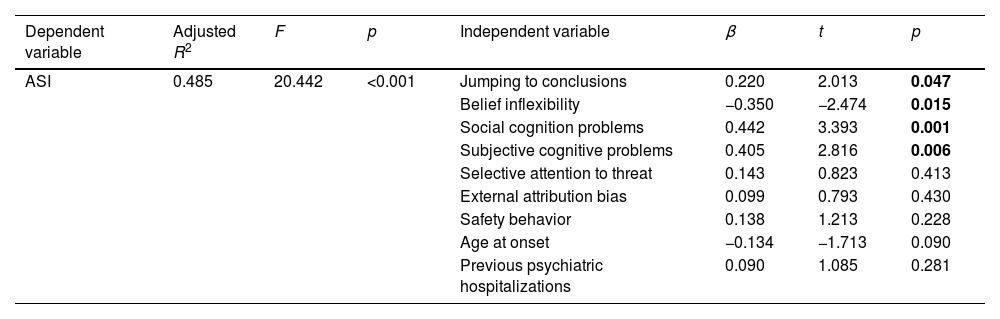
Table 4 shows the results of the linear regression model. Forty-eight percent of the variance of ASI total score was explained by the DACOBS subscales. More in detail, aberrant salience was positively associated with DACOBS subscales JTC (β=0.220), social cognition problems (β=0.442), subjective cognitive problems (β=0.405) and negatively associated with subscale BIB (β=−0.350).
Results of linear regression analysis.
| Dependent variable | Adjusted R2 | F | p | Independent variable | β | t | p |
|---|---|---|---|---|---|---|---|
| ASI | 0.485 | 20.442 | <0.001 | Jumping to conclusions | 0.220 | 2.013 | 0.047 |
| Belief inflexibility | −0.350 | −2.474 | 0.015 | ||||
| Social cognition problems | 0.442 | 3.393 | 0.001 | ||||
| Subjective cognitive problems | 0.405 | 2.816 | 0.006 | ||||
| Selective attention to threat | 0.143 | 0.823 | 0.413 | ||||
| External attribution bias | 0.099 | 0.793 | 0.430 | ||||
| Safety behavior | 0.138 | 1.213 | 0.228 | ||||
| Age at onset | −0.134 | −1.713 | 0.090 | ||||
| Previous psychiatric hospitalizations | 0.090 | 1.085 | 0.281 |
ASI: Aberrant Salience Inventory.
The bold p values indicated the statistical significance.
The goal of our study was to explore the relationship between ASI and DACOBS. As assumed individuals with a higher level of aberrant salience show more severe cognitive biases and ASI dimensions correlated with DACOBS subscales. Furthermore, ASI was positively associated with DACOBS subscales JTC, social cognition problems and subjective cognitive problems. Unexpectedly a negative association emerged between ASI and BIB.
DiscussionOur findings indicate that JTC bias and cognitive limitations – social cognition problems, subjective cognitive problems – were associated with a more severe level of aberrant salience in a sample of individuals with SSDs. Conversely, BIB displayed a negative association with aberrant salience.
Excess striatal dopamine has been proposed as the cause of an abnormal attribution of significance to irrelevant or harmless stimuli, which can lead to the emergence of psychotic experiences as a “top-down” cognitive attempt to make sense of these aberrantly salient experiences.22 Certain cognitive models propose that the presence of reasoning bias is essential for anomalous experiences of aberrant salience to turn into frank psychotic symptoms.11 In line with these models, we found an association between some cognitive biases and aberrant salience.
One of the most extensively studied cognitive biases is the JTC bias, which has been consistently linked to both subclinical and clinical psychosis,23 as well as contributing to the progression and persistence of psychosis.24 Moreover, the JTC bias has been found not only in non-delusional and recovered persons with psychosis, but also in individuals at a clinical high-risk and first-degree relatives of subjects with psychosis.25 Thus, it has been identified as a potential intermediary phenotype.26
Interestingly, one study found that individuals with lifetime affective dysregulation were more likely to progress from low/moderate psychosis levels (i.e., state of aberrant salience) to high psychosis levels (i.e., frank psychosis) if the JTC bias was present.24 Indeed, individuals experiencing adverse interpersonal experiences may perceive otherwise irrelevant stimuli as overly salient and consequently, in search of an explanation, develop threatening beliefs about the environment and others.27 The JTC bias may play a fundamental role in this process: individuals’ inclination to make hasty decisions without considering alternative explanations might correspond in daily life in the form of more hurried conclusions about others’ negative intentions, which may subsequently result in more entrenched delusional beliefs.27 Therefore, the presence of JTC bias may impact the processes of appraisal linked to salient experiences and their threatening interpretation resulting in a vicious cycle of increasing severity of psychosis and distress.28 These data corroborate our findings about the association between JTC and aberrant salience.
Belief flexibility is a reasoning skill that implies reflecting on individual's beliefs, modifying them in the light of consistent facts, and generating and considering alternatives.29 The delusional belief is maintained when the individual jumps to conclusions and fails to consider the possibility that his own beliefs are wrong.30 Studies have found that lower belief flexibility predicted stronger delusional conviction over time. Unexpectedly, our study revealed a negative association between BIB and aberrant salience. This inverse correlation may be explained by theories proposing that delusions originate from a preference for explanatory adequacy.31 According to this perspective, an individual's beliefs are primarily grounded on perceptual information rather than previous beliefs, thereby supporting the negative correlation between BIB and aberrant salience.31
In addition, the concept of aberrant salience has been analyzed using a computational method that focuses on learning in dynamic surroundings. This approach suggests that when significant information stands out, it indicates a likely change in the environment that necessitates quick adjustments to one's beliefs.32 Based on these findings, it is possible to understand aberrant salience as arising from an unusually high estimation of the rate at which the environment is shifting, resulting in faster belief updates when faced with changes.32 This understanding of the aberrant salience theory aligns with the idea that there is an inverse relationship between aberrant salience and BIB in individuals with SSDs.
Impairments in neurocognitive and social cognitive abilities in individuals with SCZ are associated with reduced functional capacity and poor real-world functioning.33 Social cognition was defined as the ability to perceive, interpret, and process social information in real-world contexts, as well as being able to build representations of the relationship between self and others and use them flexibly to guide social behavior.34 Evidence indicates substantial impairments in emotion processing (particularly facial affective perception), perception of social cues, attributional and mentalizing style (i.e., the “Theory of Mind”)35 in people with SCZ. A unified model proposing abnormal dopaminergic firing and social cognitive impairment suggests that individuals diagnosticated with SCZ are prone to attribute negative emotions and intentions to neutral social stimuli. According to this explanation chaotic dopaminergic signaling in the ventral striatal areas can give rise to the emergence of aberrant salience when exposed to such stimuli, while reduced prefrontal activation and connectivity with the limbic system would result in diminished cognitive regulation over the emotional processing of these stimuli.36 Consistent with previous findings, our study revealed an association between social cognition deficits and aberrant salience.37
Several lines of evidence suggest that cognitive impairments, spanning from attention and memory to executive functions, occur early in the progression of SCZ and worsens over the course of the disease.35 The evidence supporting the association between cognitive deficits and aberrant salience found in our study is corroborated by research indicating a connection disrupted connectivity in the salience network and cognitive deficits in subjects with psychosis.38
Overall, our findings should be interpretated in the light of various limitations. Firstly, our cross-sectional design fails to consider the longitudinal progression of psychosis and the complex course of illness, which suggests that different mechanisms may come into play at different stages of SSDs.10 Second, the reliance on self-reported measures of cognitive biases and aberrant salience in our study precludes the possibility of replicating our results using experimental tasks assessing aberrant salience and cognitive biases. Nonetheless, other studies have reported the validity of the DACOBS,19,20 which we used in our study, also included meaningful relations with performance-based tasks.19 ASI has also shown excellent psychometric properties13 and moreover, in line with Kapur's39 conception according to which aberrant salience drives the phenomenological experience of psychosis, is correlated to other measures of psychotic experiences, such as magical ideation, dissociation and absorption,12 as opposed to task measurements (e.g., the Salience Attribution Test – SAT).40
Moreover, we did not conduct an a priori sample size power analysis, since the sample was mainly based on a naturalistic consecutive enrolment in the psychiatric facility without applying any statistical criteria. Finally, the current study did not establish a correlation between delusional symptoms and aberrant salience or cognitive biases, since the severity of the delusional symptomatology of the participants has not been assessed. Nonetheless, in our previous research,41 we have already shown a connection between aberrant salience and psychotic symptoms in a group of individuals with schizophrenia spectrum disorders. For the present study, our primary objective was to examine the link between aberrant salience and cognitive biases.
ConclusionsAs far as we know, this is the first study that attempts to elucidate the potential link between subjective cognitive biases, as measured by DACOBS, and aberrant salience. Our results suggest that JTC bias, social cognition problems and subjective cognitive problems may be fundamental in the occurrence of anomalous experiences, such as aberrant salience, in individuals with SSDs. These anomalous experiences may stem from a range of neuropsychological abnormalities in perceptual and emotional processing.32 Further research is needed to investigate the causal relationship between cognitive biases and aberrant salience in the development and maintenance of psychosis, as suggested by previous evidence,42 and to develop comprehensive prevention and intervention strategies that specifically target these cognitive biases and aberrant salience.8