Complex diagnostic profiles (i.e., clusters of comorbid disorders) may be present in adolescence with long-lasting effects later in life. Little is known about their developmental transitions to adulthood as well as potential risk factors. This study aimed to identify the diagnostic profiles in adolescence and emerging adulthood, patterns of transitions and risk factors.
Material and methodsA sample of 1062 Mexican adolescents (43.22% men, M=14.19 years at baseline, SD=1.68) was assessed for psychiatric disorders at adolescence and emerging adulthood. Latent class analysis was used to identify diagnostic profiles. Profile transition was studied using multi-state modeling between the life periods. Logistic regression was utilized to study risk factor influence on profile development in adulthood.
ResultsThree diagnostic profiles (i.e., minimal disorder/no-psychopathology; and two clinical profiles: internalizing and externalizing) were identified in both periods. Anxiety disorders were the most frequent psychiatric presentation in adolescence, while depression was the most prevalent disorder in adulthood. More than 15% of participants showed a clinical profile regardless life period. Comorbidity was present in 57% of participants with a clinical psychiatric profile. Finally, common (suicidal behavior) and specific risk factors (sex, parents’ education and income) predicted transitions to profiles from adolescence to emerging adulthood.
ConclusionsPsychiatric disorders are frequently observed adopting a complex diagnostic profile in both adolescence and emerging adulthood. Comorbidity seems to be common in both life periods. Developmental issues and comorbidity should be considered for health service provision and treatment choice.
Adolescence constitutes a critical vulnerability period for psychopathology development, due to the interaction between contextual demands and puberty-driven changes.1–3 Disorder comorbidity is a common phenomenon among adolescents with a psychiatric disorder, observing high proportions of adolescents (between 40 and 70%) suffering from at least two psychiatric conditions at a given moment.4–6 The increased prevalence becomes adolescent comorbidity a critical issue to take into account for treatment choice.
Some studies have aimed at identifying the heterogenous diagnostic profiles (i.e., clusters of mental disorders) among adolescents, from a data-driven approach. However, existing literature provides divergent results in terms of profile enumeration. Moreover, disorder co-occurrence is often overlooked in these studies. In line with previous symptom-based studies among younger children,7,8 McElroy et al.9 found four diagnostic profiles among children aged 7.5 years old: a low-endorsement/normative profile, an internalizing, an externalizing and a high-comorbidity profile. These profiles were also identified at age 13. The authors observed that 41% of participants showed at least two comorbid disorders at age 7.5 and 43% at age 13. Unfortunately, the authors did not provide details on comorbidity within each diagnostic profile. Essau and De la Torre-Luque10 identified three adolescent diagnostic profiles, considering lifetime prevalence of psychiatric disorders: a low-disorder profile, comorbid emotional disorders profile and comorbid behavioral disorders profile. In this study, adolescents from the behavioral psychiatric profile showed a higher number of lifetime diagnoses (6.03 diagnoses on average), in comparison to those from either the emotional psychiatric profile (4.45 diagnoses on average) or the low-disorder profile (less than one disorder on average). In line with the accumulation hypothesis, externalizing symptoms and conduct problems may be more likely to become risk factors for disorder development either concurrently or later in life.7,11 For that reason, it would be reasonable individuals with profiles mainly featured by externalizing disorders to show higher comorbidity levels.
The impact of adolescent psychopathology may have a pivotal impact on emerging adulthood. Unfortunately, there is a paucity of longitudinal studies aimed at depicting diagnostic profile transitions from adolescence to adulthood. In contrast, existing studies have focused on individual disorders,12,13 overlooking paths of interaction between comorbid disorders within profile as well as the interplay of these complex (but common in the real world) diagnostic profiles with contextual risk factors. Adolescent psychopathology in interaction with challenges and daily hassles (e.g., exposure to stressful events, poverty), considered common vulnerability factors, may lead to increasing risk of mental disorder development later in life.14–18 Moreover, the impact of adolescent psychiatric conditions on adult disorder development may be boosted by some individual intermediators (also common vulnerability factors), such as emotional regulation deficits and self-destructive behavior in a more severe extent (e.g., suicidal behavior).19,20
The identification of data-driven diagnostic profiles may inform about variation patterns in disorder comorbidity and transitions across critical life periods, coming from a holistic approach. Moreover, it may contribute to identify pathophysiological paths of development by studying specific interactions between diagnostic profile and contextual factors. This may therefore help improve decision taking on treatment provision (e.g., comorbidity management). This study aimed to identify the heterogeneous diagnostic profiles in a large metropolitan area-representative sample of adolescents and their transition patterns to emerging adulthood. We expected to detect at least two profiles in both adolescence and emerging adulthood: one featured by internalizing disorders and another characterized by externalizing disorders. Comorbidity would be more common in profiles mainly featured by externalizing disorders in comparison to those mainly featured by internalizing disorders, in line with the accumulation hypothesis. On the other hand, we aimed to study the role of risk factors involved in diagnostic profile development in emerging adulthood. We hypothesized that contextual factors (e.g., poverty, family composition, the experience of traumatic events) as well as emotional regulation factors (i.e., suicidal behavior) would have a relevant role in the profile transition from adolescence to emerging adulthood.
MethodsParticipantsThe Mexican Adolescent Mental Health Survey is a prospective two-wave panel study. The wave I survey was a stratified multistage area probability sample representative of the nearly two million adolescents aged 12–17 that resided in the Mexico City Metropolitan Area in 2005. Three thousand and five participants completed the wave I survey (survey during adolescence) with a 71% response rate. Further details of the wave I sample design and procedures have been previously reported.21 The wave II survey (survey during emerging adulthood) was conducted eight years later in 2013 in which 1071 young adults aged 19–26 were re-interviewed. Of the original sample, 2763 provided contact information for future participation, and of those, 2470 households were located for wave II, however in 622 households, no informant had or was willing to provide information on participant whereabouts, 101 had moved to another city, state or country, 12 had died, 2 were in jail and 5 were hospitalized. Thus 1728 were eligible for re-interview; of those, 128 declined participation, 517 were not found at home on any of the visits and 12 had incomplete interviews. Therefore, data was based on the remaining 1071 participants with a response rate of eligible participants of 62% (though this is only 35.60% of the wave I sample). Further details of the wave II sample have been previously reported.22 For this study, participants with a posttraumatic stress disorder at baseline were ruled out due to its very low prevalence (n=9). As a result, the sample in analysis was 1062 individuals (56.78% males, M=14.19 years at baseline, SD=1.68).
ProceduresFace-to-face interviews were conducted in the homes of the participants by trained lay interviewers after providing a verbal and written explanation of the study. Informed consent (and assent from minors) was obtained from parents at wave I and from the young adult participants at wave II. At wave II, all study participants were given a pamphlet of the study findings from wave I and contact information for institutions from which they could seek services should they wish to do so. The Internal Review Board of the National Institute of Psychiatry approved the research.
Diagnostic assessmentThe World Mental Health version of the WHO Composite International Diagnostic Interview 3.0 (WMH-CIDI)23 evaluated psychiatric disorders at both waves. The wave I survey used the adolescent version of the WMH-CIDI while Wave II used the adult version.24 The WMH-CIDI is a fully structured computer-assisted interview that generates diagnoses for DSM-IV mental disorders including depressive disorders (major depression and dysthymia), anxiety disorders (panic disorder, agoraphobia, generalized anxiety, social phobia, specific phobia, obsessive-compulsive disorder and separation anxiety), disruptive behavior disorders (intermittent explosive disorder, oppositional defiant disorder, conduct disorder, attention deficit hyperactivity disorder), substance use disorders (alcohol abuse, alcohol dependence, drug abuse, drug dependence, nicotine dependence), eating disorders (anorexia nervosa, binge disorder, bulimia) and bipolar disorders (type I and type II disorders). For the purpose of the analyses reported here, we included disorders that met diagnostic criteria in the 12 months prior to the interview.
Assessment of predictorsThe CIDI assessed general socio-demographics and other common risk factors of psychiatric disorders. We included the following information from wave I: sex, age, family constellation, educational and employment status of the participant, and the educational attainment and income of their parents. Family constellation was categorized as living with both parents (or not) in 2005. Participants were considered students if enrolled as a student in 2005 (or dropouts if not). Adolescents were asked whether they worked full-time during the school year. The participants were asked about the educational attainment of each of their parents and we classified that variable based on the parent with the highest level. Parental household income was categorized into tertiles. Crude 12-month prevalence of suicide ideation and attempt were also considered. Number of childhood adversities was the sum of having experienced the following 12 chronic adversities as measured by the WMH-CIDI (physical abuse, neglect, sexual abuse, parent with a mental illness, parent with a substance use problem, parent with criminal behavior, witnessing domestic violence, death of a parent, parental divorce, other parental loss, serious physical illness, and economic adversity). Finally, the number of acute traumatic events experienced was considered. This was conceptualized as the sum of the individual events (the 23 listed events in the WMH-CIDI posttraumatic stress disorder traumatic section; these included events like being mugged, being in a life-threatening accident, a natural disaster, etc.) the adolescent has experienced.
Data analysisIdentification of diagnostic profiles was based on a latent class analysis (LCA) approach. LCA allows modeling a discrete latent variable (i.e., profiles of comorbidity) by means of common responses of multiple items or diagnoses.25 In order to improve communication and decision-making at a practical level,26 the 12-month diagnoses of the aforementioned composite diagnostic categories (depressive disorders, anxiety disorders, disruptive behavior disorders, substance use disorders, eating disorders and bipolar disorders) were considered as clustering variables. Anorexia nervosa was excluded from the eating disorder category as no participants fulfilled its criteria within our sample. Moreover, obsessive-compulsive disorder was excluded from the anxiety disorder category as current diagnostic manuals endorse its distinctive nature as an independent disorder.27 Latent class enumeration relied on unconstrained models (class enumeration without covariates) in order to prevent class overestimation.28,29 Diagnostic profile enumeration was estimated separately for baseline and follow-up survey data.
To study the longitudinal patterns between diagnostic profile classes across measurement waves, a multi-state model was fitted.30 The multi-state model relied on Markov chains for finite series of time, considering the profile classes as dynamic statuses. Years from baseline was used as a time variable. Moreover, longitudinal prevalence analysis was conducted by means of estimating crude prevalence to show each diagnostic profile class over time as well as expected prevalence (i.e., number of individuals from each class at a given time, multiplied by the product of the crude prevalence at the initial time and the transition probability matrix in a given time interval). Linear regression was used to study whether the expected estimates evolve over time.
We performed logistic regressions to study the influence of risk factors on diagnostic profile transition in adulthood. We included two types of baseline covariates: sociodemographic (sex, age, parents’ education level, family constellation, household income, whether the participant was enrolled as a student, and whether the participant worked) and psychosocial covariates (suicidal ideation in the prior 12 months, a suicide attempt in the prior 12 months, number of chronic adversities, number of traumatic events in the prior 12 months). Profile class membership at baseline was used as a weighting factor. We compared the following models according to traditional best-fit indices: an unconstrained model (model without covariates), a model with sociodemographic factors and a full model (model with sociodemographic and psychosocial covariates). The AIC statistic and the pseudo-R2 index by Cragg and Uhler were used to evaluate model fit. Relative risk ratio (RRR) coefficients (or odds ratio [OR] for binary logistic regression) were used to indicate the association between outcome category and each covariate.
All the analyses were conducted using STATA v. 14 and R software, packages poLCA and msm.31,32 Further details on the analytical strategy are provided in the Supplementary material.
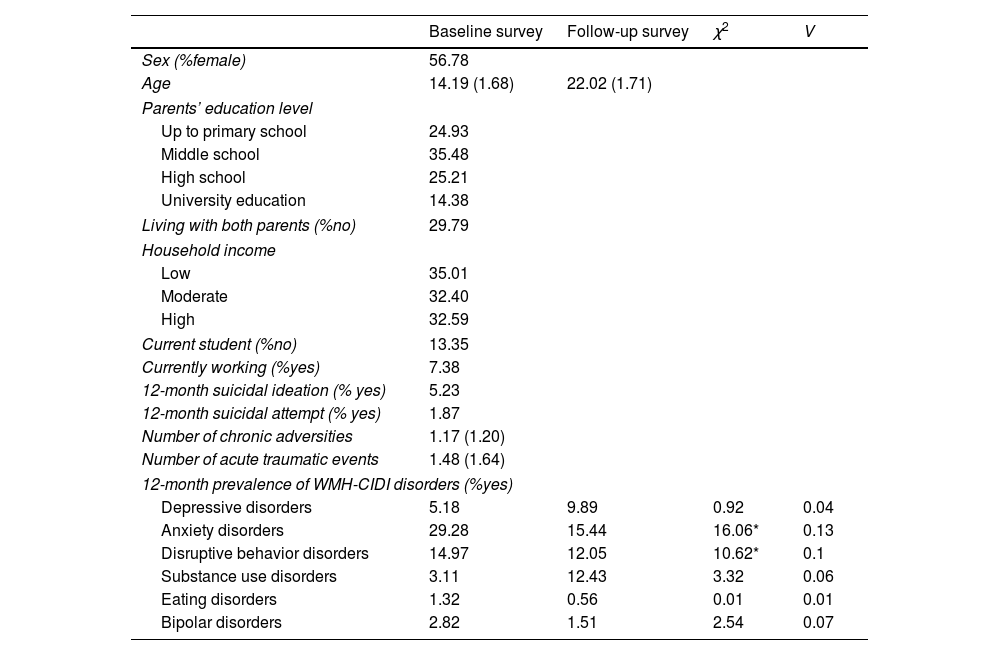
ResultsDescriptive statistics of sample participants are displayed in Table 1. We found a similar proportion of diagnosed 12-month disorders in both measurement occasions, except when considering anxiety disorders and disruptive behavior disorders. In both cases, a lower proportion of diagnoses was observed at the follow-up measurement.
Descriptive statistics. Mexican Adolescent Mental Health Survey follow-up, 2005–2013 (N=1062).
| Baseline survey | Follow-up survey | χ2 | V | |
|---|---|---|---|---|
| Sex (%female) | 56.78 | |||
| Age | 14.19 (1.68) | 22.02 (1.71) | ||
| Parents’ education level | ||||
| Up to primary school | 24.93 | |||
| Middle school | 35.48 | |||
| High school | 25.21 | |||
| University education | 14.38 | |||
| Living with both parents (%no) | 29.79 | |||
| Household income | ||||
| Low | 35.01 | |||
| Moderate | 32.40 | |||
| High | 32.59 | |||
| Current student (%no) | 13.35 | |||
| Currently working (%yes) | 7.38 | |||
| 12-month suicidal ideation (% yes) | 5.23 | |||
| 12-month suicidal attempt (% yes) | 1.87 | |||
| Number of chronic adversities | 1.17 (1.20) | |||
| Number of acute traumatic events | 1.48 (1.64) | |||
| 12-month prevalence of WMH-CIDI disorders (%yes) | ||||
| Depressive disorders | 5.18 | 9.89 | 0.92 | 0.04 |
| Anxiety disorders | 29.28 | 15.44 | 16.06* | 0.13 |
| Disruptive behavior disorders | 14.97 | 12.05 | 10.62* | 0.1 |
| Substance use disorders | 3.11 | 12.43 | 3.32 | 0.06 |
| Eating disorders | 1.32 | 0.56 | 0.01 | 0.01 |
| Bipolar disorders | 2.82 | 1.51 | 2.54 | 0.07 |
Note. Means and standard deviations are displayed for continuous variables. Percentage of cases is displayed for dichotomous/categorical variables. The χ2-based test was used to compare diagnosed cases between measurement occasions. The Cramer‘s V was used as an effect size estimate of comparisons.
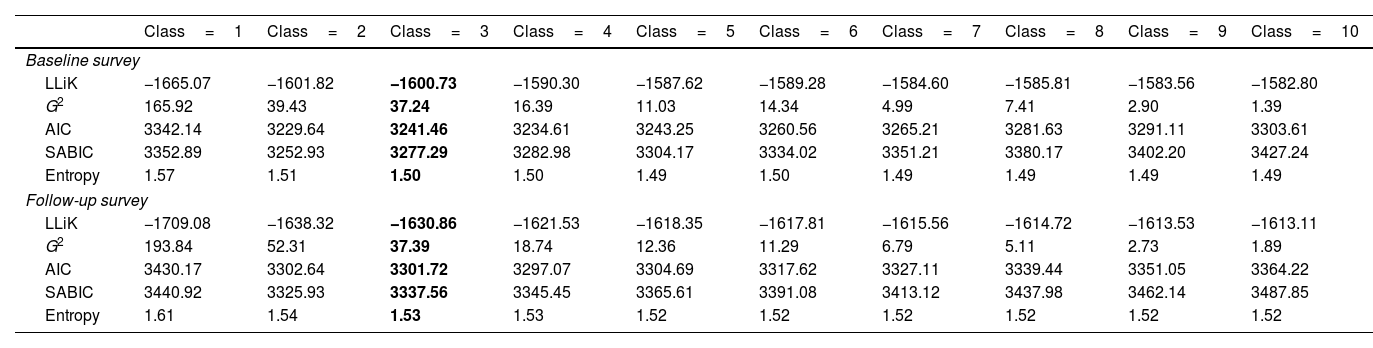
For the wave I adolescent survey, the 3-class model showed a better fit (see Table 2), with low fit indexes (AIC=3241.45, SABIC=3277.29 and entropy=1.50) and adequate means of posterior probabilities of classification (p between .80 to .90, on average). The conditional probabilities of diagnosis endorsement by class are displayed in Table S1 (see the Supplementary material). Class 1 (internalizing class: n=55, 5.18% of sample) was characterized by the highest probability to meet criteria for an anxiety disorder (63.64% of participants within this class) and lower probability for any other disorder (mean number of disorders=1.76, sd=0.51). Within this class, substance use disorder was the second most prevalent (38.18% of participants). Most participants in this class had two co-occurring disorders (69.09% of participants), the most common pairs of disorders being anxiety and depressive disorders (36.84%) and anxiety and bipolar disorders (23.68%). Few participants had more than two co-occurring disorders (3.64%). The second class (normative class: n=848, 79.85% of sample) was characterized by low probability of any disorder (mean number of disorders=0.25, sd=0.43; 22.88% of participants had an anxiety disorder and 1.89% of participants had a depressive disorder). Finally, class 3 (externalizing class, n=159, 14.97% of the sample; mean number of disorders=1.86, sd=0.78) was characterized by having a disruptive behavior disorder (100% of participants within this class) and high probability of an anxiety disorder (51.57% of participants), followed by the probability of showing a depressive disorder (14.47% of participants) Comorbidity of two disorders (disruptive behavior disorder plus other) was shown in 78.64% of participants of this class. On the other hand, 21.36% of individuals from the externalizing class had three or more comorbid conditions, the most common comorbid presentations being anxiety-depression-disruptive disorder (47.06% of individuals with more than two comorbid disorders) and anxiety-bipolar-disruptive behavior disorder (29.41%). The proportion of participants with comorbidity was significantly different between classes, χ2(2)=642.46, p<.01, Cramer's V=.78. The proportion of participants with comorbidity was significantly higher in both the internalizing (χ2(1)=628.25, p<.01, V=.84) and externalizing classes (χ2(1)=518.12, p<.01, V=.77) in comparison to those from the normative class. Finally, participants from the externalizing class showed higher risk of comorbidity than those from the internalizing class, χ2(1)=15.22, p<.01, V=.27; even though the effect size of this difference was moderate.
Latent class model fit for each measurement wave. Model comparison table.
| Class=1 | Class=2 | Class=3 | Class=4 | Class=5 | Class=6 | Class=7 | Class=8 | Class=9 | Class=10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline survey | ||||||||||
| LLiK | −1665.07 | −1601.82 | −1600.73 | −1590.30 | −1587.62 | −1589.28 | −1584.60 | −1585.81 | −1583.56 | −1582.80 |
| G2 | 165.92 | 39.43 | 37.24 | 16.39 | 11.03 | 14.34 | 4.99 | 7.41 | 2.90 | 1.39 |
| AIC | 3342.14 | 3229.64 | 3241.46 | 3234.61 | 3243.25 | 3260.56 | 3265.21 | 3281.63 | 3291.11 | 3303.61 |
| SABIC | 3352.89 | 3252.93 | 3277.29 | 3282.98 | 3304.17 | 3334.02 | 3351.21 | 3380.17 | 3402.20 | 3427.24 |
| Entropy | 1.57 | 1.51 | 1.50 | 1.50 | 1.49 | 1.50 | 1.49 | 1.49 | 1.49 | 1.49 |
| Follow-up survey | ||||||||||
| LLiK | −1709.08 | −1638.32 | −1630.86 | −1621.53 | −1618.35 | −1617.81 | −1615.56 | −1614.72 | −1613.53 | −1613.11 |
| G2 | 193.84 | 52.31 | 37.39 | 18.74 | 12.36 | 11.29 | 6.79 | 5.11 | 2.73 | 1.89 |
| AIC | 3430.17 | 3302.64 | 3301.72 | 3297.07 | 3304.69 | 3317.62 | 3327.11 | 3339.44 | 3351.05 | 3364.22 |
| SABIC | 3440.92 | 3325.93 | 3337.56 | 3345.45 | 3365.61 | 3391.08 | 3413.12 | 3437.98 | 3462.14 | 3487.85 |
| Entropy | 1.61 | 1.54 | 1.53 | 1.53 | 1.52 | 1.52 | 1.52 | 1.52 | 1.52 | 1.52 |
Note. LLik=log-likelihood convergence value; G2=conditional χ2 test statistic; AIC=Akaike information criterion; SABIC=Sample-adjusted Bayesian information criterion.
The selected model is highlighted in bold face.
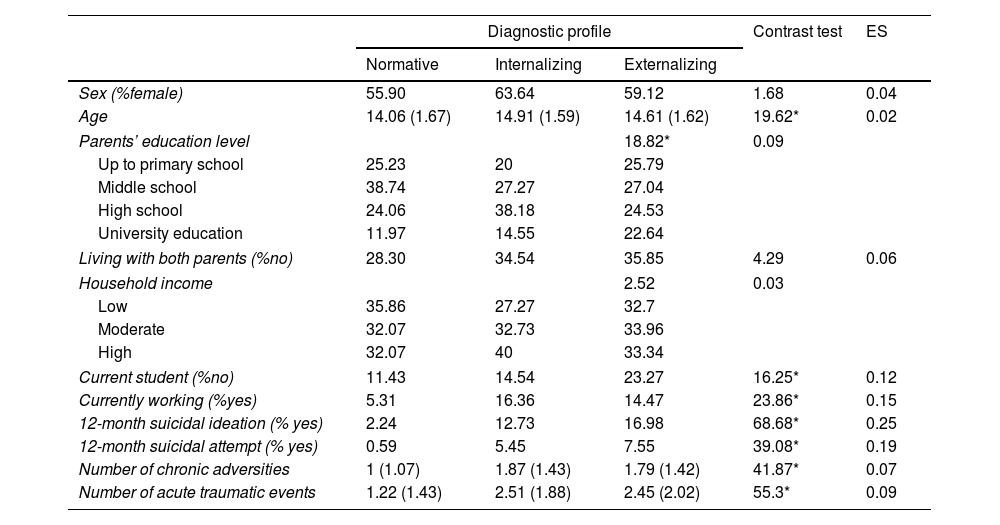
Table 3 displays the main characteristics of participants according to class at wave I. Meaningful between-group differences were found for the number of chronic adversities, F(2, 1059)=41.87, p<.01, η2partial=0.07; and for the number of acute traumatic events, F(2, 1059)=55.3, p<.01, η2partial=0.09. Members in both the internalizing and externalizing classes experienced more chronic adversities as well as traumatic events than members from the normative class. However, no differences were found between both these clinical diagnostic profiles in terms of these factors.
Sociodemographic and clinical characteristics of psychopathology classes at baseline.
| Diagnostic profile | Contrast test | ES | |||
|---|---|---|---|---|---|
| Normative | Internalizing | Externalizing | |||
| Sex (%female) | 55.90 | 63.64 | 59.12 | 1.68 | 0.04 |
| Age | 14.06 (1.67) | 14.91 (1.59) | 14.61 (1.62) | 19.62* | 0.02 |
| Parents’ education level | 18.82* | 0.09 | |||
| Up to primary school | 25.23 | 20 | 25.79 | ||
| Middle school | 38.74 | 27.27 | 27.04 | ||
| High school | 24.06 | 38.18 | 24.53 | ||
| University education | 11.97 | 14.55 | 22.64 | ||
| Living with both parents (%no) | 28.30 | 34.54 | 35.85 | 4.29 | 0.06 |
| Household income | 2.52 | 0.03 | |||
| Low | 35.86 | 27.27 | 32.7 | ||
| Moderate | 32.07 | 32.73 | 33.96 | ||
| High | 32.07 | 40 | 33.34 | ||
| Current student (%no) | 11.43 | 14.54 | 23.27 | 16.25* | 0.12 |
| Currently working (%yes) | 5.31 | 16.36 | 14.47 | 23.86* | 0.15 |
| 12-month suicidal ideation (% yes) | 2.24 | 12.73 | 16.98 | 68.68* | 0.25 |
| 12-month suicidal attempt (% yes) | 0.59 | 5.45 | 7.55 | 39.08* | 0.19 |
| Number of chronic adversities | 1 (1.07) | 1.87 (1.43) | 1.79 (1.42) | 41.87* | 0.07 |
| Number of acute traumatic events | 1.22 (1.43) | 2.51 (1.88) | 2.45 (2.02) | 55.3* | 0.09 |
Note. Means and standard deviations are displayed for continuous variables. Percentage of cases is displayed for dichotomous/categorical variables. The ANOVA-based F test (continuous variables) and χ2 test (dichotomous/categorical variables) were used as contrast test statistics. Effect size (ES) estimates were the η2partial for continuous variables and Cramer's V for non-continuous ones.
Regarding the wave II survey, the 3-class solution also showed a better fit to the data, with AIC=3301.72, SABIC=3337.56 and entropy=1.53 (see Table 2). Means of posterior probabilities of belonging to each class were adequate (p between .84 and .95, on average; see Table S1 in the Supplementary material for disorder probabilities). The first identified class (internalizing class, n=79, 7.44% of the sample; mean number of disorders=1.37, sd=0.58) was characterized by higher probability of depressive disorders (98.73% of participants). Anxiety disorders were the second most prevalent disorder in this class (22.78% of participants). Substance use disorder was present in only 5.06% of participants classified into this class. Over one in three class members (31.64% of participants) showed at least two co-occurring conditions the most common pair being anxiety and depressive disorders (72% of members with comorbid conditions), followed by depression and substance use disorder (16%). Class 2 (normative class: n=900, 84.75% of the sample) was characterized by low probability of any mental disorder (most prevalent disorder=anxiety disorder, 9.67% of participants). Only 1.11% of class members (mean number of disorders=0.25, sd=0.47) showed comorbid disorders (in all cases, anxiety and substance use disorder). Finally, in class 3 (externalizing class: n=83, 7.81% of sample; mean of number of disorders=2.59, sd=0.70) all participants showed at least two co-occurring disorders (48.42% of participants with three or more comorbid conditions). Disruptive behavior (90.36% of participants) was the most common disorder followed by anxiety (71.08% of participants), substance use (50.60% of participants) and depressive disorders (32.53% of participants). The most common comorbid disorder pairs in this class were anxiety and disruptive behavior disorder (62.65% of members with at least two comorbid conditions), followed by disruptive behavior disorder with substance use disorder (42.17%). Class members with three or more comorbid disorders mainly showed either anxiety-substance use-disruptive disorders (37.5%) or anxiety-depression-disruptive disorders (37.5%). The proportion of participants with comorbidity was significantly different between classes, χ2(2)=788.85, p<.01, Cramer's V=.86. The proportion of participants with comorbidity was significantly higher in both the internalizing (χ2(1)=187.67, p<.01, V=.45) and externalizing classes (χ2(1)=856.05, p<.01, V=.94) in comparison to those from the normative class. Additionally, the externalizing class showed significantly more participants with comorbidity than the internalizing class, χ2(1)=82.05, p<.01, V=.72.
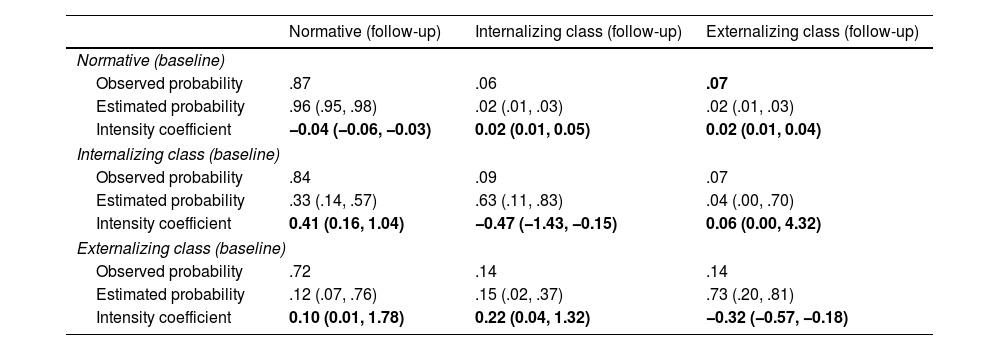
Estimated probabilities of transitioning from wave I classes to wave II classes are displayed in Table 4, according to the multi-state model. This model converged properly, with AIC=1147.29. Probability of remaining in the minimal disorder class (normative class) across waves was p=.96 (CI95=.95, .98). Over 10% of participants (n=109) who did not meet criteria for any disorder at baseline moved to either an internalizing class or an externalizing class at follow-up. On the other hand, probability of moving to a class of minimal psychopathology (normative class) was low when coming from either the internalizing class (p=.33, CI95=.14, .57) or the externalizing class (p=.12, CI95=.07, .76). In terms of continuity, probability of remaining in the internalizing class was p=.63 (CI95=.11, .83); and remaining in the externalizing class was, p=.73 (CI95=.20, .81).
Transition probabilities from the baseline survey (adolescent time point) and to the follow-up survey (emerging adult time point).
| Normative (follow-up) | Internalizing class (follow-up) | Externalizing class (follow-up) | |
|---|---|---|---|
| Normative (baseline) | |||
| Observed probability | .87 | .06 | .07 |
| Estimated probability | .96 (.95, .98) | .02 (.01, .03) | .02 (.01, .03) |
| Intensity coefficient | −0.04 (−0.06, −0.03) | 0.02 (0.01, 0.05) | 0.02 (0.01, 0.04) |
| Internalizing class (baseline) | |||
| Observed probability | .84 | .09 | .07 |
| Estimated probability | .33 (.14, .57) | .63 (.11, .83) | .04 (.00, .70) |
| Intensity coefficient | 0.41 (0.16, 1.04) | −0.47 (−1.43, −0.15) | 0.06 (0.00, 4.32) |
| Externalizing class (baseline) | |||
| Observed probability | .72 | .14 | .14 |
| Estimated probability | .12 (.07, .76) | .15 (.02, .37) | .73 (.20, .81) |
| Intensity coefficient | 0.10 (0.01, 1.78) | 0.22 (0.04, 1.32) | −0.32 (−0.57, −0.18) |
Note. The estimated probability of moving from an initial diagnostic profile class (in rows) to another (in columns) is displayed. First row shows the observed probability. The second row shows the estimated transition probability under the multistate model. Transition intensities are displayed in bold face (third row). For all estimated transition probabilities and intensities, the 95% confidence interval is shown (between brackets).
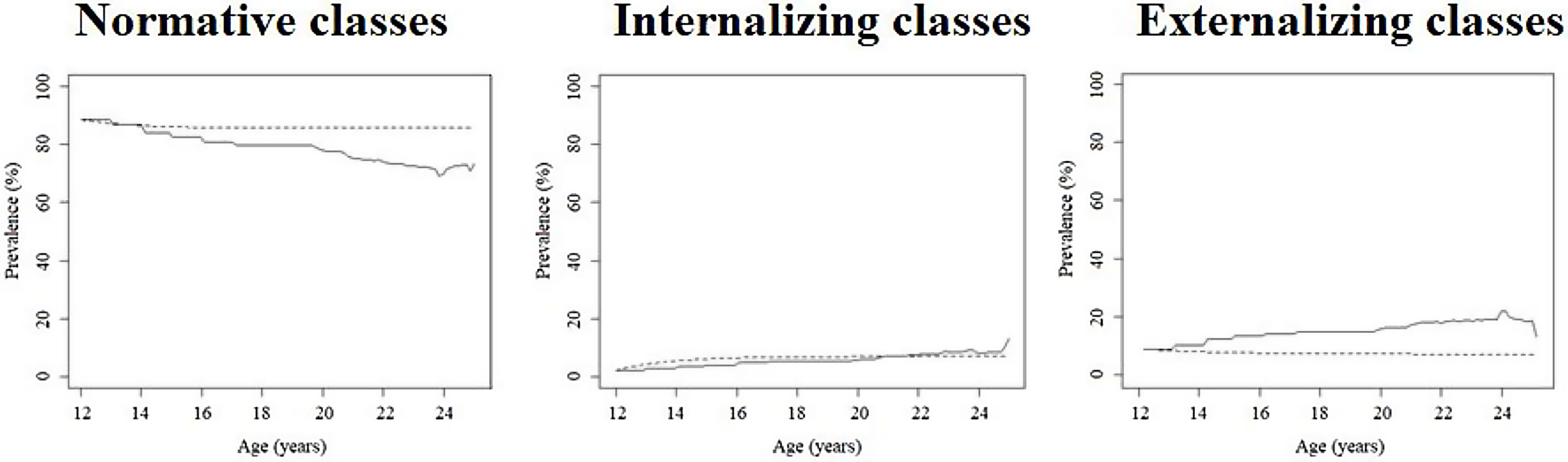
Fig. 1 displays the crude and predicted (expected) prevalence estimates of each class over time. A downward trend (see the predicted prevalence depicted by the dashed line) was found for the prevalence of the normative class over time (B=−0.16, SE=0.07; t=−2.48, p<.05). On the other hand, an increasing trend was observed for individuals with internalizing profiles with age, B=0.28, SE=0.10; t=2.87, p<.05. Finally, a negative slope of age was observed for externalizing class prevalence over time, B=−0.11, SE=0.03; t=−3.66, p<.05. These results point to descending patterns of minimal psychopathology and externalizing classes with age, and ascending prevalence of internalizing disorder classes over time.
Prediction of longitudinal psychiatric profiles from adolescence to emerging adulthoodVery few participants transitioned within internalizing classes across measurement occasions (n=5); or within externalizing classes (n=23). This hindered evaluating transition patterns among comorbidity profiles with the same predominant disorders. Thus, four statuses were considered to study diagnostic profile transitions between measurement occasions: (1) stable low psychopathology (n=739), defined by individuals who were classified into the normative class in both measurement occasions; (2) transition to an internalizing profile (n=74), observed in participants who moved to the internalizing class from any other baseline class (71.62% came from the normative class and 28.38% from the externalizing psychopathology class); (3) transition to an externalizing profile (n=60), defined by participants moving to the externalizing class at follow-up (93.33% of participants came from the normative class); and psychopathology remission (n=161) when transitioning from either the internalizing (28.57% of participants) or externalizing class (71.43% of participants) to the normative class at follow-up.
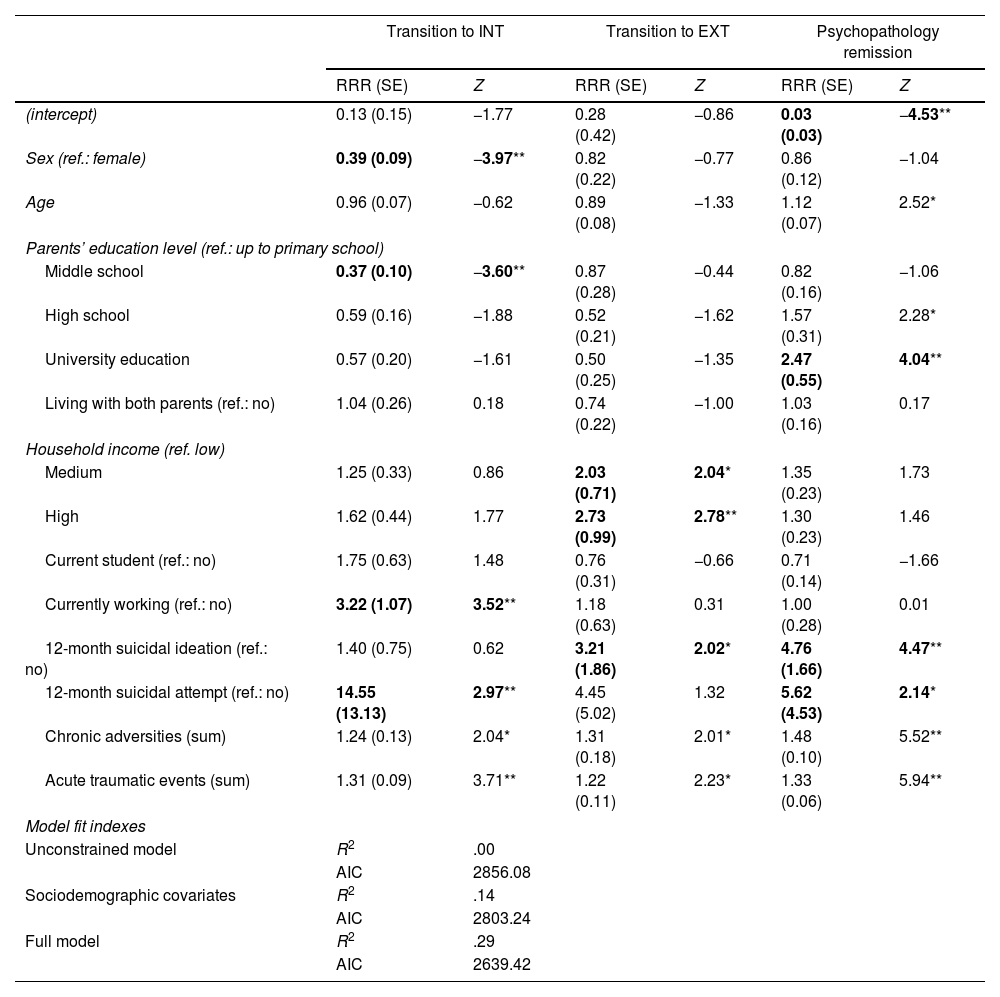
Table 5 displays the relative risk of baseline covariates to predict class membership transitions (in comparison to stable no psychopathology membership) in the multinomial regression model. Firstly, it is important to mention that the model with all the covariates explained better the outcome than both the unconstrained and the sociodemographic covariate models, as shown by its lower AIC. This model showed a Cragg and Uhler's R2=.29. According to this model, the transition to internalizing psychiatric profile at follow-up was predicted by being female and working at baseline, as well as having made a suicide attempt when adolescent (RRR=14.55, SE=13.13, Z=2.97, p<.01). The rest of covariates did not show a meaningful predictive risk (RRR>2 or RRR<0.5). On the other hand, the transition to externalizing psychiatric profile class was predicted by medium (RRR=2.03, SE=0.71, Z=2.04, p<.05) and high household income (RRR=2.73, SE=0.99, Z=2.78, p<.01) and suicidal ideation (RRR=3.21, SE=1.86, Z=2.02, p<.05). Finally, moving to a no-psychopathology class (in comparison with stable no psychopathology) was predicted by the meaningful predictive risk of parents’ university education (RRR=2.47, SE=0.55, Z=4.04, p<.01), suicide ideation in adolescence (RRR=4.76, SE=1.66, Z=4.47, p<.01) and suicide attempt (RRR=5.62, SE=4.53, Z=2.14, p<.05).
Regression coefficients to explain diagnostic profile transitions.
| Transition to INT | Transition to EXT | Psychopathology remission | ||||
|---|---|---|---|---|---|---|
| RRR (SE) | Z | RRR (SE) | Z | RRR (SE) | Z | |
| (intercept) | 0.13 (0.15) | −1.77 | 0.28 (0.42) | −0.86 | 0.03 (0.03) | −4.53** |
| Sex (ref.: female) | 0.39 (0.09) | −3.97** | 0.82 (0.22) | −0.77 | 0.86 (0.12) | −1.04 |
| Age | 0.96 (0.07) | −0.62 | 0.89 (0.08) | −1.33 | 1.12 (0.07) | 2.52* |
| Parents’ education level (ref.: up to primary school) | ||||||
| Middle school | 0.37 (0.10) | −3.60** | 0.87 (0.28) | −0.44 | 0.82 (0.16) | −1.06 |
| High school | 0.59 (0.16) | −1.88 | 0.52 (0.21) | −1.62 | 1.57 (0.31) | 2.28* |
| University education | 0.57 (0.20) | −1.61 | 0.50 (0.25) | −1.35 | 2.47 (0.55) | 4.04** |
| Living with both parents (ref.: no) | 1.04 (0.26) | 0.18 | 0.74 (0.22) | −1.00 | 1.03 (0.16) | 0.17 |
| Household income (ref. low) | ||||||
| Medium | 1.25 (0.33) | 0.86 | 2.03 (0.71) | 2.04* | 1.35 (0.23) | 1.73 |
| High | 1.62 (0.44) | 1.77 | 2.73 (0.99) | 2.78** | 1.30 (0.23) | 1.46 |
| Current student (ref.: no) | 1.75 (0.63) | 1.48 | 0.76 (0.31) | −0.66 | 0.71 (0.14) | −1.66 |
| Currently working (ref.: no) | 3.22 (1.07) | 3.52** | 1.18 (0.63) | 0.31 | 1.00 (0.28) | 0.01 |
| 12-month suicidal ideation (ref.: no) | 1.40 (0.75) | 0.62 | 3.21 (1.86) | 2.02* | 4.76 (1.66) | 4.47** |
| 12-month suicidal attempt (ref.: no) | 14.55 (13.13) | 2.97** | 4.45 (5.02) | 1.32 | 5.62 (4.53) | 2.14* |
| Chronic adversities (sum) | 1.24 (0.13) | 2.04* | 1.31 (0.18) | 2.01* | 1.48 (0.10) | 5.52** |
| Acute traumatic events (sum) | 1.31 (0.09) | 3.71** | 1.22 (0.11) | 2.23* | 1.33 (0.06) | 5.94** |
| Model fit indexes | ||||||
| Unconstrained model | R2 | .00 | ||||
| AIC | 2856.08 | |||||
| Sociodemographic covariates | R2 | .14 | ||||
| AIC | 2803.24 | |||||
| Full model | R2 | .29 | ||||
| AIC | 2639.42 | |||||
Note. Outcome comprises four categories: stable no psychopathology (reference class); transition to INT (moving to internalizing diagnostic profile class at follow-up); transition to EXT (moving to externalizing diagnostic profile class at follow-up); and psychopathology remission (transition from either internalizing or externalizing diagnostic profile class to no psychopathology or normative class).
RRR=Relative risk ratio. SE=Standard error. Z=Z-based statistic for Wald's test. R2=Cragg and Uhler's R2. AIC=Akaike information criterion.
The unconstrained model refers to model without covariates. The sociodemographic covariate model adds sociodemographic covariates to the unconstrained model. The full model adds sociodemographic and psychosocial covariates to the unconstrained model.
RRR with meaningful loadings are highlighted in bold.
To identify potential factors involved in psychopathology remission, we conducted a binary logistic regression in which we compared the psychopathology remission class (those who transitioned from either the internalizing or externalizing profile class at baseline to the no-psychopathology class at follow-up, n=161) to those that either remained or transitioned to any clinical diagnostic profile (internalizing or externalizing) class at follow-up (n=53). This group comprised those individuals who remained within either a similar internalizing (n=5) or externalizing profile classes (n=23) and those who moved to another clinical diagnostic profile class (those who transitioned from the internalizing class to the externalizing one, n=21; or vice versa, n=4). As a result, the model including sociodemographic covariates fitted the data better (AIC=643.50; R2=.20) than either the unconstrained one (AIC=669.23; R2=.00) or the model comprising both sociodemographic and psychosocial covariates (AIC=647.12; R2=.22). The transition from a diagnostic profile class to remission (in comparison with those who were in a psychiatric profile class at follow-up) was predicted by having parents with a high school (OR=2.81, SE=0.29, Z=3.56, p<.01) or university education (OR=3.03, SE=0.32, Z=3.48, p<.01) and not working in adolescence (OR=0.30, SE=0.27, Z=−4.45, p<.01).
DiscussionThis study aimed at gaining insight into the existing diagnostic profiles in adolescence and emerging adulthood. Moreover, it intended to study the role of risk factors in clinical diagnostic profile emergence in adulthood. We found a profile of minimal psychopathology in most participants, followed by a profile of internalizing disorders in which anxiety was the most prevalent disorder in adolescence and depression in emerging adulthood; and finally, a class of externalizing profile with high prevalence of disruptive behavior. Over 20% of participants in adolescence and 15% in adulthood showed a clinical diagnostic profile. Moreover, more than 56% of clinical diagnostic profile members showed comorbid disorders.
Our results are consistent with the hypothesis of adolescence as a critical period for anxiety disorder development mainly due to maturational changes in socioemotional processing systems (e.g., hypothalamus-pituitary-adrenals axis, dorsal medial prefrontal cortex).1,3,33 Moreover, substance use disorders were quite prevalent in the adolescent internalizing class and both clinical diagnostic profile classes (i.e., internalizing and externalizing classes) in adulthood. Heightened reward sensitivity may precipitate the onset and escalation of substance use, leading to a higher probability of dependence disorder development in emerging adulthood.34,35 Depression turned out to be more prominent in the internalizing profile in emerging adulthood than in adolescence. Some evidence suggests that depressive disorders may have a peak of incidence in emerging adulthood.36,37 Finally, the main diagnoses in the externalizing class were disruptive behavior disorders, regardless of measurement occasion. The disruptive behavior typology comprised varying externalizing disorders (i.e., intermittent explosive disorder, oppositional defiant disorder, conduct disorder, attention deficit hyperactivity disorder) highly frequent in adolescence and emerging adulthood probably due to identity and personality formation in these periods.2,38,39
Some discrepancies were observed between our results and those from other studies with regard to profile enumeration. In this sense, several studies identified four diagnostic profiles (i.e., normative, internalizing, externalizing, high comorbidity class) in adolescence and adulthood.9,40,41 A methodological issue may be the main reason for those discrepant results: more stringent criteria were followed in our study to select a model with optimal class enumeration (i.e., means of posterior probabilities of belonging to each class ≥.80; and at least 5% of sample classified into each class). Despite these methodological discrepancies, an overall similar conclusion is found across studies: a diagnostic profile featured by high probability of an internalizing disorder and another class with high probability of showing externalizing disorders. Comorbidity was very frequent in both classes, but especially in the externalizing profiles, in line with the accumulation hypothesis and some studies that have highlighted the role of a history of externalizing problems as a critical risk factors for new disorder development later in life.7,11
Transitions to the internalizing class in adulthood were predicted by being female and working in adolescence. Sex has been widely associated with internalizing disorders.36,42 Working during adolescence may be related to financial difficulties, daily hassles and unfavorable working conditions of adolescents in Mexico. Moreover, we identified profile-specific risk factors: having made a suicide attempt in adolescence (besides being female). On the other hand, high levels of household income and suicidal ideation were related to transitioning into externalizing diagnostic profile in adulthood. Suicidal behavior may be an intermediator in the development of future psychopathology, due to its emotional regulation function.18,43 Briere et al.19 demonstrated that people who engaged in suicide attempting in adolescence showed poorer adjustment and higher use of mental health services. Moreover, suicide attempters were at twofold risk of developing an anxiety disorder in adulthood. On the other hand, suicidal ideation has been associated with antisocial behavior, delinquency and substance use in adulthood, beside internalizing disorders.44 Finally, higher levels of income may be related to substance use in adulthood.45
On the other hand, chronic adversities and traumatic events did not show a meaningful effect on psychopathology development and between-class transition. We speculate that the impact of stressful and traumatic events may be mediated by intermediators related to emotional regulation. A recent study found that young adults with problems in emotional regulation (i.e., profiles featured by self-harm and suicidal behavior) during adolescence showed a poorer mental adjustment to the COVID-19 pandemic impact.17 In a same vein, numerous studies have supported the mediating role of emotional regulation in the relationship between the history of traumatic and stressful event exposure and psychopathology development in emerging adulthood.46,47
We also examined predictors of remission. In other words, we studied factors that predicted transitions from clinical diagnostic profiles in adolescence to the normative class in emerging adulthood, in comparison to those showed a clinical profile in the emerging adulthood (i.e., those who remained in the internalizing or externalizing classes in adulthood, or transitioning between these classes). Remission was associated with higher parental education levels and not working in adolescence (this may entail more time devoted to education). Parents with higher levels of education may help their children to cope with mental health problems more efficiently.48 In addition, higher levels of education in the adolescent may be related with better management of mental health service needs and help adolescents focus on the developmental demands of adolescence.49,50
This study provides some relevant results on psychopathology transitions between two critical period across the lifespan, adopting a real-world approach (i.e., diagnostic profiles) and covering longitudinal dynamics in continuous time (i.e., multi-state analysis) and comorbidity statuses. Another strength of this study is the large metropolitan area-representative cohort of Mexican adolescents followed longitudinally from adolescence to adulthood.
On the other hand, some limitations should be noted. First, LCA constitutes a data-driven analytical technique. For that reason, results from this study should be considered cautiously to provide an overall picture of diagnostic profile dynamics from adolescence to emerging adulthood. Second, the validity of the estimates from this prospective survey may be affected by the large rate of attrition. However, we found no attrition bias for mental disorders (i.e., there was no significant difference in baseline disorder prevalence among those that participated in and did not participate in the follow-up measurement; see Benjet et al.,22 for attrition analysis results). Third, psychotic disorders were not considered for diagnostic class identification. The main reasons were that the structured interview used in this study did not include a module on psychotic disorders; and the lack of consensus for the diagnosis of psychotic disorders in young adolescents.51 Four, additional information on some clinical factors (e.g., subthreshold disorders and history of treatments, social environment) would have further enriched our understanding of transitions between psychiatric profiles and help to disentangle specific psychopathology underpinnings. Finally, we were unable to study risk factors involved in psychiatric profile continuity and transition due to small cell sizes. Some of our estimates showed large standard errors for this reason.
Some clinical implications may be derived from our findings. First, governments should take action to promote community program development to prevent from psychopathology perpetuation from adolescence to adulthood. Second, assessment protocols should be extended for the examination of mental health in community samples. Disorder co-occurrence is quite likely and wide-range assessment allows for diagnostic precision. Additionally, this study stresses the importance of implementing multi-component interventions to deal with diagnostic profiles, due to the high proportion of individuals with comorbid disorders. On the other hand, the inclusion of interventions to target common risk factors may prevent the development of psychiatric comorbidity. Finally, therapeutic choice should be guided by diagnostic profile, the presence of comorbidity and developmental issues to prevent psychiatric conditions becoming chronic.
Conflict of interestThe authors declare that they do not have any conflict of interest.
Wave I of the Mexican Adolescent Mental Health Survey was supported by the National Council on Science and Technology and Ministry of Education (Grant CONACYT-SEPSSEDF-2003-CO1-22). Wave II was supported by the National Council on Science and Technology (Grant CB-2010-01-155221) with supplementary support from Fundación Azteca. The survey was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation and fieldwork.
In addition, this study was supported by the Instituto de Salud Carlos III-FIS under grant number PI20/00229, co-supported by European Regional Development Fund (ERDF)’ a way to build Europe’.