During the COVID-19 pandemic, authorities confined adults, adolescents and children to their homes. Recent articles warn of possible long-term consequences on mental health, especially for those who suffer from underlying psychiatric conditions and for vulnerable sections of the population. The present study explores the psychological impact of the COVID-19 quarantine on outpatients at the Centre of Child and Adolescent Mental Health (CAMHS), which is based in Barcelona.
MethodsA total of 441 caregivers answered an online ad-hoc survey on their sociodemographic and economic situation, perceived stress, and clinical changes and coping strategies observed in their children during lockdown. The Chi-square test was used to compare the response percentages for each behaviour or symptom between age, gender and diagnostic groups. Variance and post-hoc test were also analyzed, as was the Pearson correlation.
ResultsThe use of electronic devices has significantly increased. There has also been an increase in symptoms such as attentional problems, fatigue and irritability, among others. Differences were found between age and gender groups. The diagnostic groups most affected by confinement were Autism Spectrum Disorders and Conduct Disorders. The survey also discovered a relationship between the loss of family income, parental stress and increased symptoms in children.
ConclusionConfinement has increased externalizing symptoms and behaviours as well as COVID-19 related concerns, somatic problems and anxieties. It is important to observe the fluctuation of symptoms and how young people adapt to the pandemic in order to reach a better understanding of the situation and devise new strategies to reduce the psychological impact of the pandemic.
The pandemic of novel coronavirus disease (COVID-19), first reported in Wuhan (China) on 31 December 2019,1 has led to more than 500,000 cases in Catalonia and more than 3 million in all Spain to date.2 The Government declared a state of emergency in order to manage the health crisis3 and confined adults, adolescents and children to their homes by Royal Decree 463/2020, of 14 March 2020.
Once the risk of the collapse of the health system was reduced, around 4 May 2020, the Spanish Government managed the economic, social and mobility recovery through five 2-week phases, depending on the number and location of newly detected cases.
One month after the start of the lockdown, Spain entered phase 0, the preparation phase for a gradual relaxation. Children younger than 14 started to go outside, for an hour a day, accompanied by an adult. They could not interact with peers, go to school or share face-to-face activities with relatives with whom they did not live. Schools were closed for 3 months and little or no social contact by young people has been the norm during these months.
It was an unprecedented situation, and no one knew the psychological impact on the population. Recent articles warn of the possible long-term consequences to mental health, especially those with previous psychiatric pathology, underprivileged environments or in situations of risk.4,5
Children and adolescents are already considered a vulnerable group in emergency situations or health crises. There is a need to determine the mental health status of young people and how the situation described has affected their well-being.6,7 In the adult population, the mid and long-term effects of a lockdown due to health crises have been described, such as, an increase of post-traumatic stress disorders, a lower mood, a higher level of anxiety, poor concentration, insomnia and increased irritability,8 and it has been concluded that these effects can be wide-ranging and long-lasting. However, studies on children and adolescents are still scarce. In a study on the impact on mental health of Chinese students during the COVID-19 pandemic, more than 7000 participants answered an online questionnaire: 0.9% suffered from severe anxiety, 2.7% from moderate anxiety and 21% from mild anxiety.9
A systematic review and meta-analysis10 synthesized fifteen studies which describe the behavioural, emotional and psychological problems of children and adolescents as a result of pandemic and isolation measures. They found that overall, children and adolescents without pre-existing psychopathology were suffering from irritability (42.3%), depression (41.7%), anxiety (34.5%), and inattention (30.8%). The behavioural/psychological state of a total of 79.4% of children in the study were found to be negatively affected. At least 22.5% of the children were found to have a significant fear of COVID-19, and 35.2% and 21.3% of children had boredom and sleep disturbance, respectively. Similarly, 52.3% and 27.4% of caregivers developed anxiety and depression, respectively, while being in isolation with children.
Another systematic review carried out in Italy and Spain11 indicated that 85.7% of the parents reported changes in their children's emotional state and behaviours during the quarantine. The most frequent symptoms reported were: difficulties concentrating (76.6%), boredom (52%), irritability (39%), restlessness (38%), nervousness (38%), feelings of loneliness (31%), and feeling more uneasy and more worried (30%).
Results show that Spanish children were more affected than Italian children on most symptoms, probably due to the fact that differences in restrictions put in place by the Spanish government were more severe than those decreed by the Italian government. In addition, and the fact that there are fewer terraces and gardens in Spanish homes further exacerbates symptoms. characteristics of the homes. Furthermore in general, when the level of stress at home was higher, parents tended to report more emotional problems in their children.
There is little has been published about the psychological impact of the lockdown and restrictions due to COVID-19 in children and adolescents with a pre-existing mental disorders. In a study carried out by the mental health charity Young Minds in the United Kingdom,12 they found that 83% of the respondents (in a total sample of 2111 young people with a history of mental health needs) reported that their mental health was worse or much worse due to the current pandemic and lockdown. Many reported higher levels of anxiety, problems with sleep, panic attacks or more frequent urges to self-harm among those who already self-harmed.
Some studies were carried out during the lockdown in children and adolescents with a specific pre-existing diagnosis of a mental disorder. Specifically, in children with Attention-Deficit/Hyperactivity Disorder (ADHD), a study13 found that 34.71% of children experienced a worsening in well-being, 34.33% showed no significant changes and 30.96% were doing better, according to their parents. The subgroup of children whose condition deteriorated manifested as oppositional/defiant attitudes and emotional outbursts. Their parents also showed cited increased sleep problems and anxiety in this context. They also found an improvement reduction in of their children's level of anxiety as well as improved self-esteem, related to less school-related strain, flexible schedules and a lesser exposure to negative feed-back. In another study,14 a 53.94% of parents reported a worsening in their children's ability to stay keep focused (only children with a previous diagnosis of ADHD), 67.22% reported on increased frequency of anger frequency, and 56.02% on worse daily routine. On the other hand, more than half of the parents reported that children's behaviours in other domains areas improved or maintained the same level.
Studies with children and adolescents with a pre-existing diagnosis of Autism Spectrum Disorder (ASD) showed an increase in the frequency and intensity of behavioural problems, respectively, related with prior or behavioural co-morbidities.15 Another study16 of ASD patients found that 72.1% had negative changes in behaviour, whereas 67.9% of (72.1%), compared with children from the control group, where they mostly found reported no changes (67.9%). The majority of parents of ASD children reported a negative impact in emotion management compared to against those in control group, which reported mostly positive impact or no impact. ASD caregivers reported higher mean scores of anxiety levels in themselves than in their children. ASD children and their parents had higher levels of anxiety than their healthy counterpart ones. In the ASD group with ASD, children that who did not maintain routines had higher mean levels of anxiety than children those that who maintained routines. Another study17 compared 82 parents of children with neurodevelopmental disabilities (NDD) and 82 parents of typically developing children (TD). The results revealed a general increase in parental stress and child externalizing behaviours while self-isolating at home. Parental stress is predicted by externalizing behaviours regardless of the child's clinical status. Specifically, in the NDD group, the reduced therapeutic support produced an increase in children's externalizing behaviours.
In a study of 159 former inpatients with anorexia nervosa (AN),18 aged 13 and above, carried a study the sample consisted of 159 ormer inpatients with an age from 13 years onward. They found that approximately 70% of patients reported concerns about eating, shape and weight concerns, drive obsession for with physical activity, and loneliness, sadness, and inner restlessness increased levels of loneliness, sadness, and inner restlessness during the pandemic. In another study19 with a sample of fifty-five former inpatients with bulimia nervosa (BN), almost half of them (49%) reported a deterioration of their eating disorder symptomatology and 62% reported a reduced quality of life. The frequency of binge eating increased in 47% of patients and self-induced vomiting in 36%. Furthermore, depressive and general psychopathology symptoms increased in up to 80% of patients.
We did not find studies carried out in children with other mental health conditions, such as mood disorders, anxiety disorders or psychotic disorders. Thus, further research into the impact of lockdown and pandemic on the mental health of children and adolescents with previous psychopathology is necessary. This is a crucial concern for clinical settings and may help in the planning of actions to reduce the psychological distress of vulnerable children in the coming months.
Our main objective was to get to know the evolution of various clinical symptoms during lockdown and the coping strategies used by a sample of children and adolescents with pre-existing psychopathology who are being treated at a Child and Adolescent Mental Health Unit (CAMHS). Our first objective was to observe the impact of the lockdown in terms of specific symptoms and behaviours. Our second aim was to analyze the influence of age, gender and differential diagnosis on the psychological state of these patients. Our third objective was to observe the impact of the lockdown on the mental health of the primary caregivers. Finally, our fourth and last objective was to analyze the relation between sociodemographic data (income level, square metres of housing, outside housing spaces) and some increased risk factors for stress (percentage of reduced income, relatives engaged in the frontline fight against COVID-19, relatives at increased medical risk of COVID-19 infection, severity of medical outcome in relatives infected by COVID-19) with the total impact on patient symptoms and use of coping skills by children and adolescents.
In line with these aims, an invitation to complete an online survey was sent in May 2020 to all the families currently being treated at our Child and Adolescent Mental Health Unit (CAMHS).
Based on previous studies and on our clinical observations, we hypothesized a general increase in irritability and anxiety, and a decrease in well-being in our sample. Specifically, an increase in symptoms in anxiety disorders, an increase in irritability, anger frequency and behavioural problems in ADHD, ASD and Conduct Disorders, as well as an increase in body dissatisfaction in adolescents with eating disorders. We also hypothesized an increase in parental stress during lockdown as well as increased stress in families that have experienced loss of income, have had a relative with COVID-19 or were living with someone involved in the frontline fight against COVID.
MethodsSampleThe target population of this present study was the parents or principal caregivers of patients who attended the CAMHS, which is located in the Eixample district of Barcelona, in the year prior to the start of the lockdown (March 2019 to April 2020). The total sample consisted of a total of 1089 families. Of these, 122 were unreachable, since they did not provide their email address to the CAMHS administrative services on the grounds that they did not wish to receive communications by email. All the remaining 967 families were invited to participate. No additional analyses were conducted regarding the characteristics of the aforementioned removed subsample in comparison with the selected sample. Consent for the participation in the study was a mandatory condition for answering the questions and was automatically received online from the families that completed the survey. The final sample was composed of the families of the 441 children and adolescents that attended the CAMHS. No analyses were conducted to compare data between completers and non-completers.
ProceduresThe email sent to families contained information about the study and an invitation to participate. Parents or caregivers signed the informed consent document online, logged into the Lime Survey app and answered the questionnaire. Data was collected during phase 0 of the lockdown relaxation, from 11 May to 14 May 2020, with a focus on any change in problem behaviours during the lockdown period.
Data were encrypted and assigned an anonymous numeric code by the same app, according to the Data Protection Law. The study was approved by the Hospital Review Board.
Measurement instrumentThe research team, with a sum total of more than 75 years of experience and clinical practice in child and adolescent mental health, was composed of four clinical psychologists, one psychiatrist and one mental health nurse. The team met to design and decide by consensus the questions for the ad-hoc survey. The aim of the survey was to gather information on the improvement or impairment of symptoms and behaviours associated with the different child and adolescent mental disorders. The Scale of Confinement and Psychological Impact on Children and Adolescents (Escala de Confinamiento e Impacto Psicológico en Niños y Adolescentes; ECIPNA) was designed to be answered by the caregivers and was formed of 55 questions divided into 4 sub-sections: (a) Fifteen sociodemographic questions on the respondent and his/her family and/or patients (this included information on the person who completed the survey, the socioeconomic status and academic qualifications of the parents, age and gender of the patients, composition of the family, type of housing); this sub-section also contained questions on any possible increased risk of stress, such as income loss due to lockdown measures, family members working in the frontline against COVID-19, family members with increased medical risk in the case of infection, infected family members and outcomes; the principal diagnosis for which the patient attended the CAMHS was also collected from caregivers via ECIPNA in this first section; (b) four questions on parents/caregivers stress (worries about COVID-19, acute stress, familial disturbances and parenting satisfaction); (c) twenty-three questions on the improvement or impairment of clinical symptoms and behaviours during lockdown, such as sadness, irritability, eating and sleep disturbances, motor restlessness, inattention, getting lost in thoughts, worries about infection and fears of going outside, fatigue, somatic complaints, obsessions and compulsive behaviours, repetitive body movements, cognitive inflexibility, self-injury behaviours, social and familial withdrawal, body dissatisfaction, dependence on adults and regressive behaviours, oppositional defiant and aggressive behaviours, and abuse of electronic devices, and (d) ten questions about coping strategies used by the child or adolescent during confinement. Questions about stress in caregivers, symptoms in patients and coping strategies were answered using a Likert scale of 5 response options (much less than before confinement, a little less than before, the same as before, a little more than before, much more than before) assigning a value from 1 to 5. Total scores were calculated by adding up the values of the responses for caregivers’ stress (from 4 to 20), of the patients’ psychological impact (from 23 to 115) and of the lack of adaptive coping strategies (from 10 to 50), with higher scores indicating greater impact.
Analyses of psychometric properties (internal consistency and structure) were conducted using three sections (parents’ stress, patients’ symptoms and behaviours, and patients’ coping skills) and excluding the section on sociodemographic and familial data. The ECIPNA has demonstrated a good internal consistency for the overall survey (Cronbach's alpha=0.85) and for the patients’ symptoms section (Cronbach's alpha=0.84). Meanwhile, internal consistency for parents’ stress (Cronbach's alpha=0.51) and for coping strategies (Cronbach's alpha=0.70) were acceptable. No other standardized and validated measures nor indexes of sensibility/specificity were used on families to calculate the external validity of the survey.
Exploratory factorial analyses were tested according to principal component extraction, Varimax rotation, correlation indexes item-factor >0.30. Analyses were repeated selecting models with eigenvalues >1 or forcing the adjustment of models to 6, 5, 4 and 3 factors. Good conditions for the reduction of data were obtained both for models comprising parents’ stress, patients’ symptoms and behaviours and patients’ coping skills (Kaiser-Meyer-Olkin=0.85; Bartlett=4924.77, p<0.001) and for models limited to patients’ items (Kaiser-Meyer-Olkin=0.86; Bartlett=4806.93, p<0.001). Nevertheless, all models explained variances of up to 58%. Those with the best and most coherent distribution of items – a 4-factor model – only explained variances of up to 41%. Consequently, since the resultant models explained low amounts of variance, the reduction of the items to dimensions were excluded and the statistical analyses were carried out item by item.
Statistical analysesIn respect to the first and third aims, to observe the direction of the impact of the COVID-19 lockdown on patient symptoms and behaviours, patient coping strategies and parents’ mental health, it was necessary to use descriptive analyses that employed frequencies and percentages for each answer option. This was also necessary to clarify the sociodemographic characteristics of the sample.
Regarding the second aim, to compare the percentages of outpatients that improved, remained the same or worsened for each symptom or behaviour between gender group, between age groups (infants: younger than 8, prepubescents: 8–12, pubescents: 12–15, adolescents: 15–18) and between diagnostic groups, cross-tables and Chi-square analyses were carried out to see whether percentages were equally distributed across categories. Principal diagnostic groups were described as Attention Deficit and Hyperactivity Disorder (ADHD), Autism Spectrum Disorders (ASD), Anxiety Disorders (AnxD), Affective Disorders (AffD), Conduct Disorders (CD), Eating Disorders (EatD), Tic Disorders (TicD), Obsessive-Compulsive Disorders (OCD), Psychotic Disorders (PsyD), Trauma-Related Disorders (TrRD), Addictive-Behaviour Disorders (AddD) or Adaptative Disorders (AdD). To optimize the statistical integrity, diagnostic groups selected for cross-tables required a minimum of 20 cases; those diagnostic groups smaller than 20 were excluded for this specific analysis. In the items in which Chi-square was statistically significant (p-value<.05), and to identify the direction of the different distribution of percentages between the groups, analyses of variance (ANOVA) and post hoc tests were conducted, with Bonferroni adjustment for multiple comparisons.
Finally, in relation to the fourth aim, the Pearson's correlation coefficients were calculated. This was necessary to analyze the relation between certain elements of sociodemographic data (income level, square metres of housing, outside outlet), increased risks of stress (percentage of reduced income, relatives in the frontline against COVID-19, relatives at increased medical risk of COVID-19 infection, severity of medical outcome in relatives infected by COVID-19) the overall impact on patient symptoms, and the overall use of coping skills used by children and adolescents.
Statistical analyses were carried out using the SPSS 23 software package (SPSS, Chicago, IL, USA). p-Values lower than 0.05 were considered statistically significant.
ResultsOf the 967 families invited to participate in the survey, the caregivers of a total of 541 (56%) outpatients logged into the app to answer the questionnaire, of whom 441 completed all sections of the ECIPNA (a total of 40.5% of the study participants).
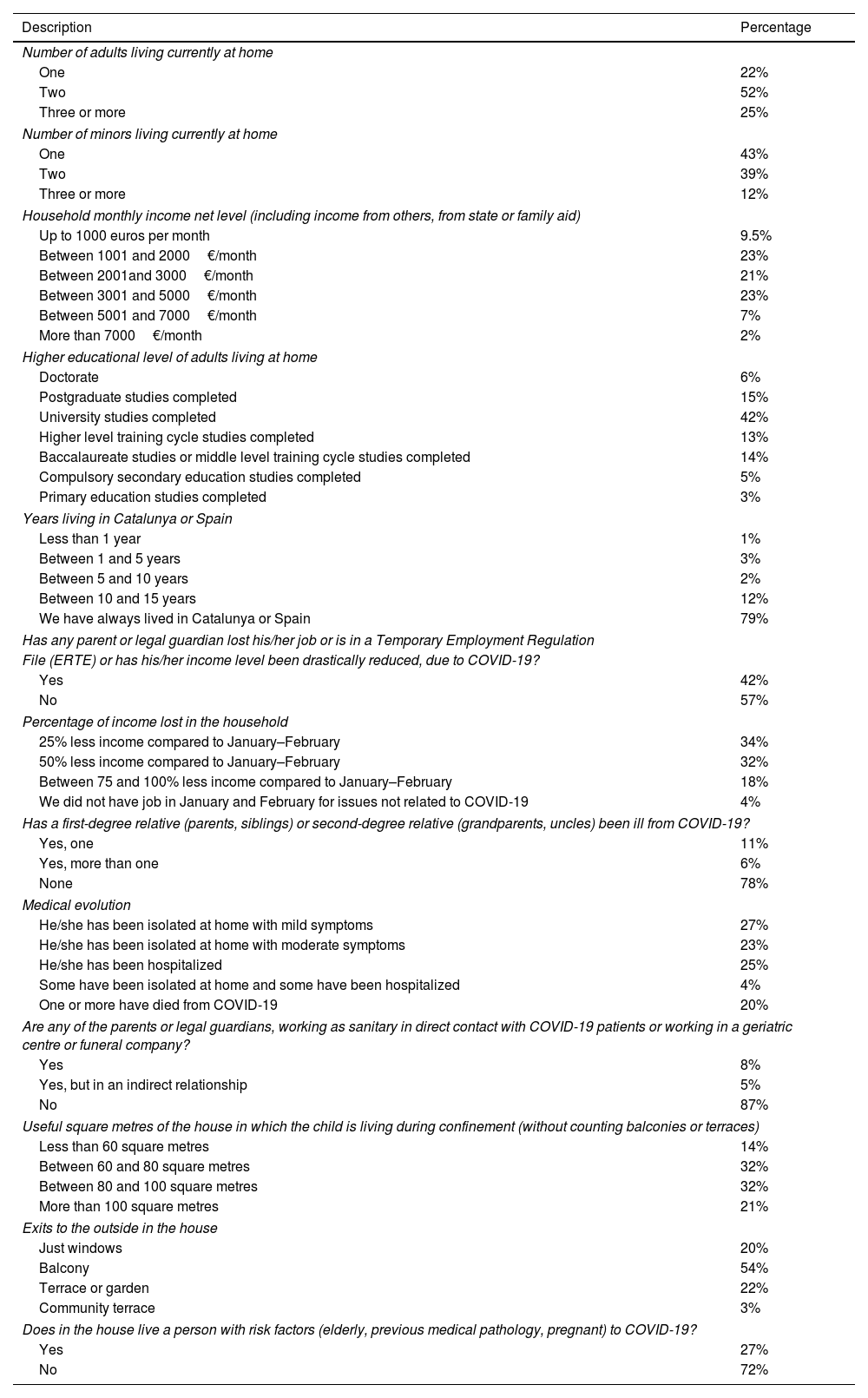
Sociodemographic, economic and medical data of familiesTable 1 shows the sociodemographic data and the composition of the sample of the participants’ families. More than 60% were families from middle or higher socioeconomic backgrounds holding university degrees. 43% had seen their incomes reduced due to COVID-19, and 57% of them reduced by half or more. 18% experienced one or more family members infected with COVID-19 of whom 24% had been hospitalized and 21%, unfortunately, had died. 13% of families had one or more adults working in the front line against COVID-19. Most of the families lived in accommodation that was larger than 60m2 with access to balconies or terraces. Two thirds of the outpatients were males, and the same proportion was older than 12. The diagnostic groups that were more frequently represented in our sample were: ADHD (n=177, 41%), ASD (n=91, 21%), AnxD (n=34, 8%), CD (n=38, 9%), AffD (n=34, 8%) and EatD (n=23, 5%), with more than 20 participants in each group. The other diagnostic categories were smaller than 20 (TicD: n=6, 1.4%; OCD: n=9, 2%; PsyD: n=3, 0.7%; TrRD: n=6, 1.4%; AddD: n=4, 1%; AdD: n=10, 2.3%).
Sociodemographic data.
| Description | Percentage |
|---|---|
| Number of adults living currently at home | |
| One | 22% |
| Two | 52% |
| Three or more | 25% |
| Number of minors living currently at home | |
| One | 43% |
| Two | 39% |
| Three or more | 12% |
| Household monthly income net level (including income from others, from state or family aid) | |
| Up to 1000 euros per month | 9.5% |
| Between 1001 and 2000€/month | 23% |
| Between 2001and 3000€/month | 21% |
| Between 3001 and 5000€/month | 23% |
| Between 5001 and 7000€/month | 7% |
| More than 7000€/month | 2% |
| Higher educational level of adults living at home | |
| Doctorate | 6% |
| Postgraduate studies completed | 15% |
| University studies completed | 42% |
| Higher level training cycle studies completed | 13% |
| Baccalaureate studies or middle level training cycle studies completed | 14% |
| Compulsory secondary education studies completed | 5% |
| Primary education studies completed | 3% |
| Years living in Catalunya or Spain | |
| Less than 1 year | 1% |
| Between 1 and 5 years | 3% |
| Between 5 and 10 years | 2% |
| Between 10 and 15 years | 12% |
| We have always lived in Catalunya or Spain | 79% |
| Has any parent or legal guardian lost his/her job or is in a Temporary Employment Regulation | |
| File (ERTE) or has his/her income level been drastically reduced, due to COVID-19? | |
| Yes | 42% |
| No | 57% |
| Percentage of income lost in the household | |
| 25% less income compared to January–February | 34% |
| 50% less income compared to January–February | 32% |
| Between 75 and 100% less income compared to January–February | 18% |
| We did not have job in January and February for issues not related to COVID-19 | 4% |
| Has a first-degree relative (parents, siblings) or second-degree relative (grandparents, uncles) been ill from COVID-19? | |
| Yes, one | 11% |
| Yes, more than one | 6% |
| None | 78% |
| Medical evolution | |
| He/she has been isolated at home with mild symptoms | 27% |
| He/she has been isolated at home with moderate symptoms | 23% |
| He/she has been hospitalized | 25% |
| Some have been isolated at home and some have been hospitalized | 4% |
| One or more have died from COVID-19 | 20% |
| Are any of the parents or legal guardians, working as sanitary in direct contact with COVID-19 patients or working in a geriatric centre or funeral company? | |
| Yes | 8% |
| Yes, but in an indirect relationship | 5% |
| No | 87% |
| Useful square metres of the house in which the child is living during confinement (without counting balconies or terraces) | |
| Less than 60 square metres | 14% |
| Between 60 and 80 square metres | 32% |
| Between 80 and 100 square metres | 32% |
| More than 100 square metres | 21% |
| Exits to the outside in the house | |
| Just windows | 20% |
| Balcony | 54% |
| Terrace or garden | 22% |
| Community terrace | 3% |
| Does in the house live a person with risk factors (elderly, previous medical pathology, pregnant) to COVID-19? | |
| Yes | 27% |
| No | 72% |
The mean score for the total psychological impact on patients was 73.7 (standard deviation=10.3). Table 2 shows that most of the outpatients remained stable for almost all psychopathological symptoms and behaviours, without changes in comparison to before the pandemic, except for a substantially increased use of electronic devices.
Impact from COVID-19 on caregivers’ stress, clinical symptoms and frequency of coping strategies of patients for the total sample (percentages), subgroups by gender (number of cases) and subgroups by age (number of cases).
| Caregivers’ stress | Much less than before | Little less than before | Similar than before | Little more than before | Much more than before |
|---|---|---|---|---|---|
| Worry about COVID-19 and consequences | 4% | 19% | 30% | 23% | 23% |
| Permanent alert state | 16.2% | 38.5% | 36.2% | 4% | 3% |
| Family tension | 8.4% | 28.6% | 36.4% | 12.6% | 9% |
| Satisfaction with parenting | 4.4% | 9.4% | 46.3% | 19.2% | 16.4% |
| Increase or impairment of SYMPTOMS and BEHAVIORS | Much less than before | Little less than before | Similar than before | Little more than before | Much more than before | Chi2 |
|---|---|---|---|---|---|---|
| Electronic devices use | 5.1% | 1.3% | 7.3% | 28.3% | 58% | |
| Female/male | 9/13 | 2/4 | 18/14 | 47/79 | 81/174 | 8.03* |
| <8/8–12/12–15/15–18 | 1/2/12/8 | 0/1/2/3 | 2/2/5/22 | 18/31/37/41 | 14/56/69/116 | 31.1 |
| Sadness/discouragement | 8.8% | 9.7% | 53.9% | 23.4% | 4.2% | |
| Female/male | 12/27 | 17/25 | 76/162 | 44/59 | 8/11 | 4.85 |
| <8/8–12/12–15/15–18 | 1/3/15/20 | 3/9/10/21 | 23/58/72/85 | 6/20/23/54 | 2/2/5/10 | 18.74* |
| Sleep problems | 3.5% | 4.4% | 50.3% | 26.5% | 15.3% | |
| Female/male | 5/11 | 7/13 | 80/143 | 45/20 | 72/45 | 1.22 |
| <8/8–12/12–15/15–18 | 0/3/7/6 | 1/3/6/10 | 19/45/62/95 | 11/25/33/49 | 4/16/17/30 | 4.95 |
| Eating behaviour problems | 6.6% | 12.1% | 60.1% | 15.5% | 5.7% | |
| Female/male | 8/16 | 25/41 | 91/177 | 28/25 | 5/25 | 12.1 |
| <8/8–12/12–15/15–18 | 3/5/5/12 | 3/12/14/39 | 25/60/72/110 | 4/10/23/16 | 0/5/11/13 | 18.63* |
| Fatigue | 4.9% | 9.5% | 55.9% | 23.4% | 6.2% | |
| Female/male | 10/12 | 17/24 | 82/166 | 38/64 | 10/17 | 2.39 |
| <8/8–12/12–15/15–18 | 3/3/8/7 | 5/15/28/56 | 23/59/68/99 | 5/15/28/56 | 0/3/9/15 | 18.56* |
| Irritability | 7.1% | 8.6% | 38.9% | 30.9% | 14.6% | |
| Female/male | 13/19 | 13/24 | 68/104 | 44/92 | 19/45 | 3.11 |
| <8/8–12/12–15/15–18 | 1/6/10/15 | 4/2/12/19 | 9/31/45/86 | 9/35/41/53 | 12/18/17/17 | 28.81 |
| Anxiety/restlessness | 7.1% | 7.3% | 41.7% | 32.7% | 11.2% | |
| Female/male | 11/21 | 13/18 | 67/117 | 49/95 | 17/33 | 0.83 |
| <8/8–12/12–15/15–18 | 1/4/8/19 | 1/4/11/15 | 11/37/59/77 | 17/35/34/59 | 5/12/13/20 | 14.10 |
| Opposition/defiance | 6.2% | 8.8% | 43.7% | 27.2% | 14.1% | |
| Female/male | 9/18 | 18/19 | 75/121 | 39/80 | 16/46 | 6.42 |
| <8/8–12/12–15/15–18 | 1/4/5/17 | 1/5/11/20 | 12/35/52/95 | 12/30/39/41 | 9/18/18/17 | 24.42 |
| Aggression/violence | 9.1% | 7.3% | 62% | 16.3% | 5.3% | |
| Female/male | 17/23 | 13/18 | 101/173 | 18/54 | 8/16 | 5.15 |
| <8/8–12/12–15/15–18 | 3/7/10/20 | 1/4/9/17 | 20/57/78/120 | 8/16/22/26 | 3/8/6/7 | 9.33 |
| Self-harm | 15% | 2.7% | 77.7% | 2.7% | 0.4% | |
| Female/male | 36/31 | 6/5 | 108/234 | 6/6 | 0/2 | 15.84 |
| <8/8–12/12–15/15–18 | 3/12/18/34 | 1/1/5/5 | 29/73/96/145 | 2/2/3/5 | 0/2/0/0 | 13.04 |
| Regressive behaviours | 13.7% | 2.4% | 77.3% | 4% | 1.3% | |
| Female/male | 29/31 | 7/3 | 113/229 | 5/12 | 2/4 | 10.63 |
| <8/8–12/12–15/15–18 | 5/6/20/30 | 1/4/1/5 | 23/72/96/151 | 5/6/4/2 | 1/3/1/1 | 27.75 |
| Worry/fear about COVID-19 | 9.1% | 5.7% | 55.2% | 25.4% | 4.2% | |
| Female/male | 18/23 | 11/14 | 77/165 | 44/69 | 6/12 | 4.10 |
| <8/8–12/12–15/15–18 | 2/8/11/19 | 0/4/7/14 | 23/49/72/100 | 9/27/30/47 | 1/4/4/9 | 6.25 |
| Be absorbed/isolated from family | 9.3% | 6.2% | 60.7% | 16.1% | 6.8% | |
| Female/male | 18/24 | 11/16 | 96/172 | 18/51 | 12/19 | 4.14 |
| <8/8–12/12–15/15–18 | 6/5/12/19 | 2/5/7/12 | 25/66/73/104 | 0/10/24/37 | 2/4/7/18 | 19.90* |
| Social contact with friends | 33.3% | 25.6% | 24.1% | 11.3% | 5.7% | |
| Female/male | 40/107 | 46/64 | 36/73 | 22/27 | 13/13 | 10.9 |
| <8/8–12/12–15/15–18 | 22/46/33/46 | 6/23/33/52 | 5/13/40/48 | 2/3/15/29 | 0/7/4/15 | 47.67 |
| Dependency on caregivers | 6% | 5.5% | 65.1% | 16.1% | 6.4% | |
| Female/male | 11/16 | 11/14 | 101/188 | 26/43 | 6/21 | 3.37 |
| <8/8–12/12–15/15–18 | 1/1/11/14 | 2/4/9/10 | 16/58/77/138 | 10/19/21/20 | 6/9/5/7 | 31.19 |
| Worry/fear about death | 6% | 1.1% | 78.2% | 11.3% | 2% | |
| Female/male | 11/16 | 3/2 | 116/228 | 23/26 | 2/7 | 5.58 |
| <8/8–12/12–15/15–18 | 3/4/11/9 | 1/0/1/3 | 23/74/99/149 | 6/7/10/27 | 2/5/2/0 | 22.36 |
| Obsessions/rituals | 6.6% | 2.2% | 77.3% | 8.4% | 1.6% | |
| Female/male | 14/16 | 6/4 | 118/223 | 11/24 | 6/12 | 4.64 |
| <8/8–12/12–15/15–18 | 3/3/9/15 | 1/1/4/4 | 26/69/93/154 | 3/12/10/11 | 2/5/6/5 | 9.71 |
| Repeated/stereotyped movements | 6.6% | 1.6% | 77.3% | 10.2% | 3.3% | |
| Female/male | 15/14 | 3/4 | 123/218 | 11/33 | 3/12 | 7.23 |
| <8/8–12/12–15/15–18 | 3/1/10/15 | 1/1/4/1 | 21/67/97/158 | 7/18/8/11 | 3/4/4/4 | 32.53 |
| Attention problems | 5.5% | 5.5% | 42.4% | 33.1% | 13.3% | |
| Female/male | 12/13 | 6/18 | 76/111 | 44/101 | 18/41 | 7.35 |
| <8/8–12/12–15/15–18 | 0/2/9/13 | 4/6/10/4 | 17/27/53/91 | 11/40/33/62 | 3/17/19/20 | 26.94 |
| Cognitive inflexibility | 6.2% | 4.9% | 62% | 19.2% | 1.1% | |
| Female/male | 15/13 | 10/11 | 97/176 | 28/57 | 5/24 | 9.80 |
| <8/8–12/12–15/15–18 | 2/4/8/14 | 1/2/8/10 | 22/50/74/128 | 6/27/26/27 | 4/7/8/10 | 14.69 |
| Body disturbances | 6% | 5.3% | 63.6% | 18.3% | 5.7% | |
| Female/male | 10/17 | 8/14 | 156/280 | 32/49 | 10/15 | 1.02 |
| <8/8–12/12–15/15–18 | 4/7/6/10 | 1/2/4/15 | 23/56/84/118 | 4/20/22/37 | 3/5/7/10 | 10.88 |
| Body dissatisfaction | 4% | 2.7% | 70.2% | 17.4% | 4.4% | |
| Female/male | 6/11 | 6/5 | 97/212 | 39/40 | 8/11 | 10.94 |
| <8/8–12/12–15/15–18 | 3/3/4/7 | 1/0/5/6 | 29/69/87/124 | 1/15/22/41 | 1/3/5/11 | 14.64 |
| Afraid to go outside | 5.5% | 1.3% | 61.2% | 20.3% | 10.6% | |
| Female/male | 14/11 | 3/3 | 91/178 | 31/58 | 16/31 | 5.52 |
| <8/8–12/12–15/15–18 | 1/4/8/12 | 1/1/2/2 | 25/58/68/120 | 4/16/30/38 | 4/12/14/17 | 7.19 |
| Adaptive COPING STRATEGIES | Always | Often | Sometimes | A few times | Never | Chi2 |
|---|---|---|---|---|---|---|
| Games, studies and entertainment | 43.7% | 29.6% | 15.8% | 7% | 3.9% | |
| Female/male | 66/122 | 46/80 | 28/40 | 12/19 | 2/15 | 5.31 |
| <8/8–12/12–15/15–18 | 8/35/60/85 | 15/23/33/56 | 7/12/21/29 | 5/11/7/8 | 0/7/0/10 | 27.54 |
| Questions and interest in COVID-19 | 6.8% | 14.7% | 37.3% | 22.4% | 18.8% | |
| Female/male | 16/13 | 23/41 | 59/103 | 36/59 | 20/60 | 9.00* |
| <8/8–12/12–15/15–18 | 1/7/4/17 | 6/8/13/37 | 16/36/50/60 | 3/20/33/40 | 9/17/21/34 | 19.46* |
| Avoid talking about COVID-19 | 3.6% | 3.4% | 12% | 21.3% | 59.7% | |
| Female/male | 4/12 | 7/7 | 22/27 | 34/58 | 87/172 | 4.40 |
| <8/8–12/12–15/15–18 | 0/3/5/8 | 3/0/3/9 | 2/8/14/26 | 7/24/22/40 | 23/53/77/105 | 13.84 |
| Participation in solidarity acts | 13.1% | 14.2% | 20.8% | 13.4% | 38.5% | |
| Female/male | 29/28 | 22/38 | 35/56 | 19/38 | 49/116 | 8.77* |
| <8/8–12/12–15/15–18 | 7/17/12/20 | 6/15/20/20 | 16/24/22/29 | 3/11/19/23 | 3/21/48/96 | 45.50 |
| Social contact with family and friends | 19.7% | 27.2% | 28.7% | 16.3% | 8.1% | |
| Female/male | 43/43 | 38/77 | 40/83 | 19/51 | 14/22 | 10.93 |
| <8/8–12/12–15/15–18 | 9/14/27/35 | 8/26/32/49 | 12/27/31/56 | 4/13/22/31 | 2/8/9/17 | 4.72 |
| Optimism/positive point of view | 23.3% | 32.1% | 25.4% | 11.3% | 7.9% | |
| Female/male | 30/72 | 44/92 | 49/61 | 15/32 | 16/19 | 7.98* |
| <8/8–12/12–15/15–18 | 8/29/30/33 | 15/24/40/59 | 7/20/31/52 | 4/10/11/24 | 1/5/9/20 | 13.60 |
| Adherence to schedules | 23.3% | 26.9% | 23.3% | 16.8% | 9.7% | |
| Female/male | 41/61 | 39/75 | 36/65 | 28/45 | 10/30 | 3.22 |
| <8/8–12/12–15/15–18 | 7/20/25/49 | 13/28/33/40 | 5/25/33/39 | 10/11/17/36 | 0/4/13/24 | 21.86 |
| Emotional verbal expression | 14.2% | 21.7% | 29% | 20.4% | 14.7% | |
| Female/male | 28/35 | 28/65 | 50/75 | 28/57 | 20/44 | 5.19 |
| <8/8–12/12–15/15–18 | 5/14/17/26 | 9/18/24/41 | 11/29/31/55 | 7/17/29/35 | 3/10/20/31 | 5.03 |
| Physical exercise | 10.2% | 15.2% | 26% | 20.1% | 28.5% | |
| Female/male | 26/18 | 24/43 | 37/71 | 30/58 | 37/86 | 12.36 |
| <8/8–12/12–15/15–18 | 3/7/8/24 | 8/18/13/27 | 16/20/28/47 | 2/26/30/30 | 6/17/42/60 | 30.77 |
| Religion | 0.2% | 1.1% | 3.6% | 5.9% | 89.1% | |
| Female/male | 1/0 | 1/3 | 7/9 | 10/15 | 135/249 | 2.70 |
| <8/8–12/12–15/15–18 | 0/0/0/1 | 0/1/1/2 | 2/7/6/1 | 0/2/9/13 | 33/78/105/171 | 17.30 |
Chi2 in bold means p-value <.05 and indicates statistically significant differences in the distribution of percentages. Indexes with
In the more detailed analysis, we observed deteriorations (a little worse or much worse), especially in attention problems, sadness, fatigue, sleep problems, irritability, anxiety, opposition and defiance, worries about COVID-19, cognitive inflexibility, somatic troubles and fears of going outside. Only two symptoms – self-harm and regressive behaviours – showed higher percentages of improvement.
Influence of age, gender and diagnosis on the psychological impact of the pandemicRegarding the influence of age, there were significant differences in the distribution of the percentages of change, with, in general, greater decreases in infants (younger than 8) and prepubescents (8–12 years) compared to pubescents12–15 and adolescents.15–18 Infants and prepubescents showed higher percentages of incremented oppositional defiant behaviours (chi2=24.4; p=.02), a gradual loss of social contact with peers (greater in the younger children) (chi2=47.7; p<.001), increased irritability (chi2=28.8; p=.004), increased dependence on adults behaviours (chi2=31.2; p=.002) and increased repetitive body movements (chi2=32.5; p=.001). Moreover, higher percentages of increased death-related anxieties were observed in the infants (chi2=22.4; p=.03). Finally, prepubescents showed increased use of electronic devices (chi2=31.1; p=.002), increased regressive behaviours (chi2=27.7; p=.006) and increased attention problems in comparison to the other age groups (chi2=26.4; p=.008).
Significantly, higher percentages were found among girls compared to boys in the following areas: slight improvement in healthy eating habits (chi2=12.1; p=.02), great improvement in self-harm behaviour (chi2=15.8; p=.003), great improvement in regressive behaviours (chi2=10.6; p=.03), slight increase in body dissatisfaction (chi2=10.9; p=.03), great improvement in inflexibility (compared to a large deterioration among boys) (chi2=9.8; p=.04); meanwhile, boys showed a larger decrease of social contact with (chi2=10.9; p=.03).
The diagnostic groups that showed higher scores of overall impact on symptoms were ASD and CD, compared to EatD (F=2.63; p=.023). There were significant differences in the distribution of percentages due to changes in the use of electronic devices (chi2=38.1; p=.009), sadness (chi2=38.4; p=.008), sleep problems (chi2=37.3; p=.011), fatigue (chi2=38.8; p=.007), defiant behaviour (chi2=35.3; p=.02) and aggression (chi2=35.1; p=.02), self-harm (chi2=43; p=.002), regressive behaviours (chi2=34.6; p=.02), being afraid of infection (chi2=31.6; p=.05), social relationships (chi2=32.4; p=.04), obsessions and rituals (chi2=35.8; p=.02), repetitive movements (chi2=47.3; p=.001) and body dissatisfaction (chi2=37.4; p=.01). But post hoc tests showed that ADHD, ASD and AnxD groups recorded significantly higher percentages in the increased frequency of self-harm and regressive behaviours than AffD. Moreover, ASD showed higher scores of augmented obsessive-compulsive symptoms and stereotyped movements than ADHD and EatD.
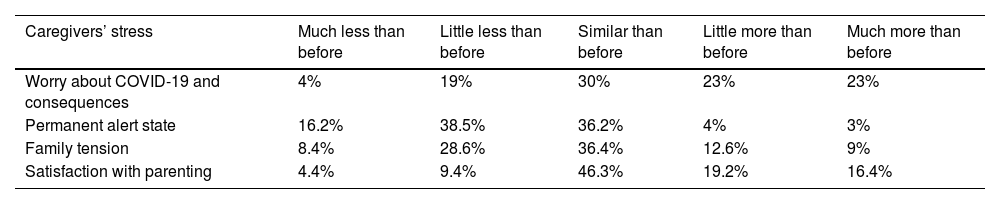
Table 2 (impact from COVID-19 on caregivers’ stress, clinical symptoms and frequency of coping strategies of patients for the total sample (percentages), subgroups by gender (number of cases) and subgroups by age (number of cases)), shows all these results
Caregivers’ stress during lockdownIn a range of scores from 5 to 20, principal caregivers reported a mean score of stress of 12.9 (SD=2.6). Table 2 reflects the percentages in each item. Although the percentages of an increase in worry were higher than those of a decrease in worry, there were low percentages of parents who felt themselves to be in slight or strong states of acute stress. There was generally more improvement than impairment in intra-familial distress during the COVID-19 quarantine; however a not negligible rate of 9% experienced a great worsening. Furthermore, the lockdown provided a little or great increase in satisfaction in paternal-filial relationships.
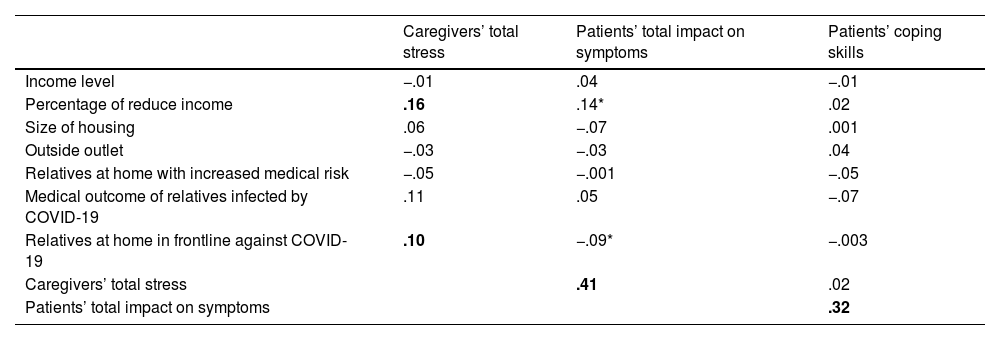
Correlations between familial and outpatient variablesThere was no significant relation between economic income level, housing size or the quality of access to outdoor space and the overall impact score of symptoms in patients or the lack of adaptive coping strategies score. Nor was there a relation between any family-related medical risk and the overall impact on symptoms or the coping strategies of patients. However, having relatives in frontline (r=.10; p=.05) and a greater loss of income (r=.16; p=.04) correlated with a higher level of caregivers’ total stress, which, in turn, correlated with a greater impact on the symptoms of children and adolescents (r=.41; p<.001). Table 3 shows the Pearson correlations between these scores.
Correlations matrix of sociodemographic data, risk factor for familial stress, caregivers’ stress, patients’ symptoms and coping strategies.
| Caregivers’ total stress | Patients’ total impact on symptoms | Patients’ coping skills | |
|---|---|---|---|
| Income level | −.01 | .04 | −.01 |
| Percentage of reduce income | .16 | .14* | .02 |
| Size of housing | .06 | −.07 | .001 |
| Outside outlet | −.03 | −.03 | .04 |
| Relatives at home with increased medical risk | −.05 | −.001 | −.05 |
| Medical outcome of relatives infected by COVID-19 | .11 | .05 | −.07 |
| Relatives at home in frontline against COVID-19 | .10 | −.09* | −.003 |
| Caregivers’ total stress | .41 | .02 | |
| Patients’ total impact on symptoms | .32 |
Pearson's correlation indexes in bold were statistically significant at p<.05. Indexes with
The mean score for a lack of adaptive coping skills was 29.5 (sd=6.3). Higher percentages of girls than boys maintained social contact with peers (chi2=10.9; p=.03) and practised regular physical exercise as coping strategies during lockdown. A significantly higher percentage of boys avoided asking about COVID-19 (chi2=9; p=.06) or participating in acts of social support (chi2=8.8; p=.07); however, boys also tended to show more optimism than girls (chi2=7.8; p=.09).
The oldest outpatients (pubescents and adolescents) coped with COVID-19 better than children younger than 12, focusing on academic tasks and games (chi2=27.5; p=.006) and relaxing their adherence to schedules (chi2=21.9; p=.04). Higher percentages of pubescents did not practise physical exercise during lockdown (chi2=30.8; p=.002) or participate in acts of social support (chi2=45.5; p<.001). Table 2 shows the frequency of coping strategies of patients for the total sample (percentages), subgroups by gender (number of cases) and subgroups by age (number of cases).
AnxD and CD groups asked a little about COVID-19 (chi2=32.5; p=.04). EatD was comparable to ASD and CD was the group most committed to acts of social support (chi2=31.8; p=.05), schedules (chi2=35.7; p=.02), and physical exercise (chi2=33.1; p=.03).
DiscussionThe various COVID-19 lockdown restrictions imposed by governments across the globe have had a psychological impact on the adults, children and adolescents of their respective populations.
There were increases in symptoms such as irritability, attentional problems, oppositional behaviours, fatigue, sleep problems, anxiety, sadness, isolation, cognitive inflexibility, body disturbances and dissatisfaction, and COVID-19- and death-related worries. Younger children showed a tendency to externalizing behaviours and adolescents a tendency to internalize. As for gender, boys were more isolated from their peers and showed greater signs of inflexibility than girls, who tended to have less self-injurious behaviours and better eating habits, albeit with more body dissatisfaction. The diagnostic groups most affected by the confinement were Autism Spectrum Disorders and Conduct Disorders. The survey also demonstrated a relationship between the loss of income of caregivers during the COVID-19 confinement period and higher levels of distress, the latter of which, in turn, had a psychological impact on the children and adolescents of the sample.
Some studies have already shown that the COVID-19 lockdown led to higher rates of symptoms of anxiety, depression, posttraumatic stress disorder, psychological distress, and stress in adults,20 and symptoms of anxiety, irritability, difficulty in concentrating, depression, fear and worry in children and adolescents.9,21
The current study supports the evidence of an additional, but not widespread, emotional impact on top of the underlying psychopathology of the outpatients of the Centre of Child and Adolescent Mental Health (CAMHS), which is located in the Eixample district of Barcelona.
Most of the parents reported an increase in the use of electronic devices in their children, especially among adolescents, without any significant differences between age groups. Indeed, the increase was seen across age groups, with boys using electronic devices more than girls. Our results align with the results of other studies, such as the one carried out in China during the COVID-19 quarantine,22 which reported an increase in excessive internet use among children and adolescents. The results from this study showed that the rates of internet addiction increased with age, with rates higher among males than females. Parents reported a general increase in usage among their children. It is important to keep in mind that school activities were being conducted electronically and that social contact was only possible through electronic devices.
Almost half of the children and adolescents showed increased difficulties in concentration. Children drastically decreased their social contact with peers, especially the youngest. When the lockdown began, children went from having very structured schedules, frequent changes of environment, academic and extracurricular activities, and regular contact with peers and adults, to spending all day at home, with fewer structured activities and no social relationships or interpersonal skills development. This social impoverishment and loss of routines added to the decrease in physical activity and shared play and may explain the increase in attention problems and ADHD traits. This effect was also seen in other reviews of children and adolescents,10,11 as well as in studies of children diagnosed by ADHD,13,14 in which there were reports of increased difficulties in concentrating.
The youngest children were more irritable, anxious and afraid of coronavirus and death. Some of them showed an increased dependency on their primary caregivers and more opposition compared to before. Previous studies support the thesis that in times of crisis, regressive behaviour and externalized symptoms can be observed in children; however, the psychological impact in adolescents may be more discreet and internalized: sleep disturbances, problems with peers, isolation, and depression.23 Since the lockdown did not permit any physical proximity with people outside the household, social communication was limited. It is well-known that anxiety disorders are more likely to occur and worsen in situations where there is little interpersonal communication.24 Furthermore, it has been reported that exposure to an excess of information about COVID-19 in social media increased worry and anxiety in adults and children.14 It is also reasonable to hypothesize that the use of masks and increased cleaning with disinfectant, together with the abundance of sensationalist and fake news, may have fomented worry, fear and anxiety as appropriate adaptive responses to the threat posed by COVID-19.
The deterioration in sleeping and eating habits was consistent with previous research,10,11 which showed that a stable and structured environment with varied activities, such as attending school, help regulate sleeping patterns and eating habits. School attendance also limits the use of electronic devices and reduces their influence on night-time rest.25
The diagnostic groups that showed the most increase in their own psychopathological symptoms were autism disorders (ASD) and behaviour disorders. The home confinement and physical and social distancing measures were especially harmful for patients with a diagnosis of ASD. The implicit learning of social skills through contact with peers should form part of the evidence-based treatment (CBT) to improve socialization, according to the National Institute for Health and Care Excellence guidelines.26 A significant relationship was observed between interpersonal relationships and the quality of life of patients with autism.27 In this respect, this current study also highlights the close relationship between social impoverishment, the interruption of specific treatments and an increase of stereotyped and obsessive-compulsive behaviours.28 Previous research conducted during the COVID-19 outbreak showed that children with ASD that did not maintain routines during confinement had higher mean levels of anxiety than children with ASD that maintained routines.16 A recent study has also shown that the reduced therapeutic support during the lockdown produced an increase in children's externalizing behaviours in children with neurodevelopmental disorders.17
Unexpectedly, outpatients who suffered from eating disorders showed less general worsening in the sample of this current study. The adherence to physical exercise and healthy routines may have acted as protective factors. These results are not in consonance with other studies that showed a significant worsening in eating symptomatology as well as in the general psychopathology for both Anorexia and Bulimia Nervosa patients during the COVID-19 confinement.18,19
Males in the sample of the current study showed a greater increase in symptoms and a general worsening during the COVID-19 lockdown. Specifically, they spent significantly more time on electronic devices, acted with greater negativism and defiance, showed more regressive behaviours, were more socially isolated from their peers, and manifested more stereotypical behaviours and motor tics compared to females; however, in contrast, they also tended to have a more optimistic attitude than girls during this health crisis. This result is in line with previous research: while girls generally develop higher rates of PTSD than boys and suffer from more symptoms in all types of trauma,29,30 boys tend to cope with acute stress through more dysfunctional emotion regulation strategies, such as passivity, avoidance, suppression and sadness inhibition.31
The results of this current study also reflected the relation between the caregivers’ loss of income during the COVID-19 pandemic and their level of psychological distress, and the relation of this second aspect with the psychological impact of the lockdown on the children and adolescents of the sample. Sprang and Silman (2013) previously observed a strong relation between the level of symptoms of post-traumatic stress disorder of parents in quarantine during the H1N1 influenza pandemic and the level of these symptoms in their children. As other authors have already stated, the financial problems and lifestyle changes caused by the COVID-19 confinement had an impact on mental health, increasing levels of psychosocial stress in adults. Those higher levels of stress in adults could then further aggravate harmful effects on their children's physical and mental health.6,32 According to Cao et al.,9 having a relative or an acquaintance infected with COVID-19 was a risk factor for anxiety among a sample of Chinese undergraduate students. Among the 7143 participants in their survey, they found that living in urban areas, family income stability and living with parents were protective factors against anxiety.
The authors of this study think it is important to analyze how the ending of lockdown affected the symptomatology of patients. Since June 2020, authorities have permitted an increase in social contact and the partial reopening of schools, along with a degree of domestic travel and summer camps. These factors reduce stress in families. The total return to schools will mark another inflection point in the pandemic, as children and adolescents adapt to a new situation after six months without attending school. It is also important to take into account the Emotional Curve of the epidemic, so named by some authors, as they try to build a conceptual model (Emotional Epidemic Curve – EEC) to represent the possible changes in emotional behaviour in the different phases.33 The authors of this study think that it is essential to be aware of possible fluctuations in the mental health of young people.
Limitations and strengthsAlthough the findings of this study are promising, they are not without their limitations. Regarding the sample, respondents were selected from a specific region with specific sociodemographic characteristics (considerable presence of middle to upper-middle class participants and university graduates) that differ from other districts or regions of the city and country. Another limitation of the sample was that the survey was mostly completed by parents of pubescents and adolescents, which is unrepresentative of the outpatient population that attended the CAMHS over the last year, with higher rates of younger people. In addition, the online participation procedure required a technological capability that some families may have lacked. Thirdly, the way in which the diagnostic was collected – from the same caregivers via an electronic survey – could be imprecise, potentially invalidating results for the relevant diagnostic group.
ECIPNA had the advantage of being specific to the situation for which it was designed. However, for this same reason, it did not allow participants to go deeper into issues or provide more information than asked. There were no standardized measures regarding the clinical evaluation made and the only informants were the patient's parents/caregivers.
A stratified or quota sample selection method would have provided more representative results not only for the sociodemographic characteristics of the district but also for the age, gender and diagnosis groups that attended the CAMHS. Such a method was not used.
Nonetheless, the focus on vulnerable and often forgotten populations, on people with current mental disorders, and on children and adolescents, together with the size of the sample, may be considered as strengths of the study.
ConclusionsThe COVID-19 pandemic has had an impact on the mental health of children and adolescents. Both previous and present studies indicate an increase in symptoms and risk behaviours among young people. The results obtained from the present study show that young people with a history of psychiatric psychopathology may have been affected by the COVID-19 pandemic and the concomitant lockdown measures implemented by authorities. The early detection of mental disorders in young people is important. Understanding the symptoms of emotional discomfort helps mitigate the risk of deterioration.
Future lines of researchThis study is part of a broader investigation whose objective is to identify the fluctuation in symptoms of patients during confinement and relaxation phases in order to be able to intervene more precisely in risk groups and learn how young people are adapting to the return to school after 6 months of non-attendance.
The authors of this paper think it is essential to identify the groups most at risk during and after lockdown; such information will help authorities, health professionals and caregivers to take into account the needs of the most vulnerable sections of the population in further outbreaks of SARS-CoV-2 or other similar epidemics that may occur in the future.
FundingNone declared.
Authors’ contributionsAll authors contributed to the study's conception and design. Material preparation, data collection and analysis were conducted by Jara López-Serrano, Sara Lera-Miguel and Rosalía Díaz-Bóveda. Data analysis was conducted by Laura Gonzalez-Vallespí and Sara Lera-Miguel. The first draft of the manuscript was written by Jara López-Serrano and Sara Lera-Miguel. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflicts of interestWe have no conflicts of interest to disclose.