Disorganization is a crucial domain in affective psychoses. However, it has received poor research attention, especially at the illness onset. The aims of this study were: (a) to monitor the longitudinal course of disorganization in young people with first episode affective psychosis (FEAP) across 2 years of follow-up, and (b) to investigate any relevant correlation of disorganized symptoms with psychopathology, functioning and the specific treatment elements of an “Early Intervention in Psychosis” (EIP) protocol along the follow-up period.
Materials and methodsSeventy-five FEAP participants (aged 12–35 years) completed the Positive And Negative Syndrome Scale (PANSS) and the Global Assessment of Functioning (GAF). Spearman's rank correlation coefficients were calculated.
ResultsDuring the follow-up, disorganized symptoms showed significant enduring positive correlations with PANSS items representing delusional thought content and uncooperativeness, as well as a persistent negative association with the GAF score. Across the 2-year follow-up period, FEAP individuals also had a relevant reduction in disorganization levels. This symptom decrease was specifically related with the combination of antipsychotic medication with the specific psychosocial components of our EIP intervention offered to FEAP patients during the first 12 months of treatment.
ConclusionsDisorganization is relevant in FEAP subjects already at their enrollment in specialized EIP protocols. However, it decreases over time, together with the delivery of specific, combined (person-tailored) EIP interventions.
In recent years, disorganization obtained increasing attention in psychosis research, due to its detrimental effect on daily functioning and social interactions.1,2 Disorganized dimension is frequent in patients with severe bipolar disorder (especially during manic episodes), in which it has been considered as an index of a core biological defect in information processing involving selective attention.3 Specifically, the ability to select/discard trivial sensory input appears to be lost in severe mania, resulting in the experience of flight of ideas, racing thoughts and “confusion”, also typically described by interviewers as a pressure of speech extending to thought incoherence and disorganization.4 Moreover, impaired ability to think, concentrate or make decisions is commonly reported by patients with major depressive episodes (especially in agitated depression).5 Recent empirical evidence also found that disorganized symptoms are common in adolescents and young people with early-onset bipolar disorder (especially in both first manic and first depressive episodes with psychotic features), where they are associated with more hospitalizations, lower inter-episodic functioning and poorer prognosis.2,6
However, despite assessing disorganized features in early-onset bipolar disorder has been considered a crucial issue in both research and clinical setting, reliable investigations on disorganization in first episode affective psychosis (FEAP) are still currently relatively scarce.7 This relatively lack of interest can be traced back to the relevance of disorganized symptoms within the traditional conceptualization of schizophrenia psychopathology.8 Moreover, another possible reason may be due to the fact that most of the widely used measures of disorganized symptoms in psychosis were primarily extracted with factor analysis methods using psychometric instruments specifically developed on the traditional, dichotomic (negative vs. positive) model of psychosis psychopathology.9 These scales were not calibrated for the specific assessment of disorganized features and the statistically extracted “Disorganization” factors often included items not typically representing disorganized symptoms (e.g. the “Disorientation” item of the Positive And Negative Syndrome Scale [PANSS]).10
Another critical area concerns whether disorganization and impairment in cognitive functions are discrete constructs. The nature of this link is still currently unclear.11 An important issue is the potential overlap between neurocognitive functioning and specific items commonly used for assessing disorganized symptoms in patients with psychosis (e.g. the PANSS “Difficulty in Abstract Thinking”, “Stereotyped Thought” and “Poor Attention” items).12
Finally, studies on disorganization have been mainly conducted in clinical samples of subjects with prolonged psychosis. To date, research in the early stages of illness (especially in FEAP individuals) is relatively scarce. Moreover, most of these investigations had a cross-sectional design. A lack of knowledge still affects the longitudinal course of disorganization in FEAP and its related treatment response. An in-depth knowledge on disorganization at the psychosis onset may also have the potential to inform specialized person-tailored interventions and to improve their effectiveness (also on long-term outcome and daily functioning).13
Starting from this background, the aim of this research was two-fold:
- (a)
to monitor the longitudinal stability of disorganization in young patients with FEAP along a 2-year follow-up period;
- (b)
to examine any relevant association of disorganization with functioning, psychopathology and sociodemographic characteristics, as well as with the specialized treatment components of an “Early Intervention in Psychosis” (EIP) program in FEAP individuals across the 2 years of follow-up.
To the best of our knowledge, no longitudinal study specifically investigating disorganized symptoms in young FEAP patients has been reported in the literature to date. We hypothesized a longitudinal decrease in disorganization severity during the follow-up period, together with the provision of specialized, evidence-based EIP interventions specifically targeting on functioning and major psychopathological aspects.
Materials and methodsSetting and participantsAll the participants were recruited within the “Parma-Early Psychosis” (Pr-EP) program between January 2013 and May 2019. Pr-EP is an EIP protocol implemented in all adolescent and adult mental healthcare centers of the Parma Department of Mental Health, in Northern Italy (for details on the Pr-EP program, see Leuci et al., 2019).14 All FEAP subjects were in a subacute phase of the current illness episode and were under pharmacological treatment (i.e. antipsychotics, antidepressants or mood stabilizers []if necessary) for less than 2 months.
Inclusion criteria of the present research were: (a) age between 12 and 35 years; (b) specialist help-seeking request; (c) presence of FEAP within the DSM-IV-TR criteria for affective (bipolar or major depressive) psychosis (APA, 2000); and (d) a Duration of Untreated Psychosis ([DUP] defined as the time interval [in weeks] between the onset of psychotic symptoms and the first antipsychotic intake)15 of <2 years. Specifically, this DUP length was selected because it is usually considered the limit to start specific EIP interventions.16 In the present study, we decided to include FEAP patients with first psychotic episode of both mania and major depression because such psychopathological syndromes may alternatively characterize the early-onset of a bipolar disorder, especially in adolescence and young adulthood.17 Indeed, it has been reported that disorganization is relatively common in FEAP adolescents and young adults (i.e. in both first manic or first depressive episodes with psychotic features).2,6
Exclusion criteria were: (a) previous psychotic episodes within DSM-IV-TR diagnoses of both non-affective and affective psychosis18 or any other previous manic or major depressive episode without psychotic symptoms; (b) past exposure to antipsychotics (i.e. in a previous illness episode, before the Pr-EP recruitment) or first antipsychotic intake for more than 2 months in the current psychotic episode; (c) known intellectual disability (i.e. Intelligence Quotient <70); (d) current DSM-IV-TR substance dependence; and (e) neurological disorders or any other medical condition with psychiatric symptoms. Specifically, we considered past exposure to antipsychotic medication as an equivalent of past psychotic episode, in line with what was proposed by Yung and colleagues,19 who defined the psychosis threshold as essentially that at which antipsychotics would probably be started in the common clinical practice.
All subjects (and their parents, if minors) gave their informed consent prior to their inclusion in this study. Local relevant ethical approvals were obtained for the research (AVEN Ethics Committee: protocol n. 36102/09.09.2019). The present study has been also carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments including humans. The data that support the findings of the current research are available on request from the corresponding author. The data are not publicly available due to privacy/ethical restrictions.
AssessmentPsychopathological evaluation of this research included the PANSS and the Global Assessment of Functioning (GAF) scale.18 These instruments were administered by trained Pr-EP team members both at baseline and every 12 months during the 2-year follow-up period. Regular supervision sessions were used to ensure the inter-rater reliability (for details on the Pr-EP assessment battery, see also Landi et al., 2020).20
The PANSS is a widely used 30-item clinical interview for evaluating the severity of psychosis psychopathology. In accordance with what proposed by Shafer and Dazzi21 in a recent meta-analysis on the PANSS factor structure, the “Disorganization” dimension specifically included the following eight PANSS items: P2 “Conceptual Disorganization”, N5 “Difficulty in Abstract Thinking”, N7 “Stereotyped Thinking”, G5 “Mannerisms and Posturing”, G10 “Disorientation”, G11 “Poor Attention”, G13 “Disturbance of Volition” and G15 “Preoccupation”. The PANSS showed good psychometric properties in clinical populations of young Italian patients with first episode psychosis.22
The GAF is a widely used scale to specifically rate socio-occupational and clinical functioning in patients with mental disorders. Scores range from 1 (“severely impaired functioning”) to 100 (“extremely high functioning”). This instrument showed good validity and reliability in Italian clinical samples with early psychosis.23,24
Procedures and data analysisAt baseline, the axis-I diagnosis was made by at least two trained Pr-EP team members using the Structured Clinical Interview for DSM-IV-TR axis I Disorders (SCID-I).25 Subsequently, all FEAP individuals were then assigned to a specialized, multi-professional team (including a clinical psychologist, a psychiatrist and a case-manager for early rehabilitation), generally within 3 weeks from the enrollment in the Pr-EP protocol.26 To all FEAP participants, it was then offered a 2-year comprehensive intervention program including a psychopharmacological treatment (based on their symptom severity) and a multi-component psychosocial intervention (combining psychoeducational sessions for family members, individual psychotherapy oriented on cognitive-behavioral principles and a recovery-oriented case management), in accordance with current guidelines on the topic.27 Specifically, low-dose atypical antipsychotics were used as first-line treatment.28 Antidepressants, benzodiazepines and mood stabilizers were also used to treat anxiety, insomnia, depression and mood elevation.
Data were analyzed using the Statistical Package for Social Science (SPSS) for Windows, version 15.0.29 All tests were two-tailed with a significance level set at 0.05. In the FEAP total sample, Spearman's correlation coefficients were calculated to investigate any relevant association of disorganization with sociodemographic characteristics, functioning and psychopathology (both at baseline and across the 2-year follow-up period), as well as with the specific treatment components provided within the Pr-EP program. In accordance with a conventional approach proposed by Schober and colleagues,30 we defined the strength of the Spearman's correlation values as follows: 0.90–1.00=very strong correlation, 0.70–0.89=strong correlation, 0.40–0.69=moderate correlation, and 0.10–0.39=weak correlation. The Mann–Whitney U test was performed to compare continuous parameters in inter-subgroup analyses. The Wilcoxon test for repeated measures was used to investigate the longitudinal stability of disorganization along the 2-year follow-up period. The Holm–Bonferroni p value correction was performed to control the problem of multiple comparisons.31
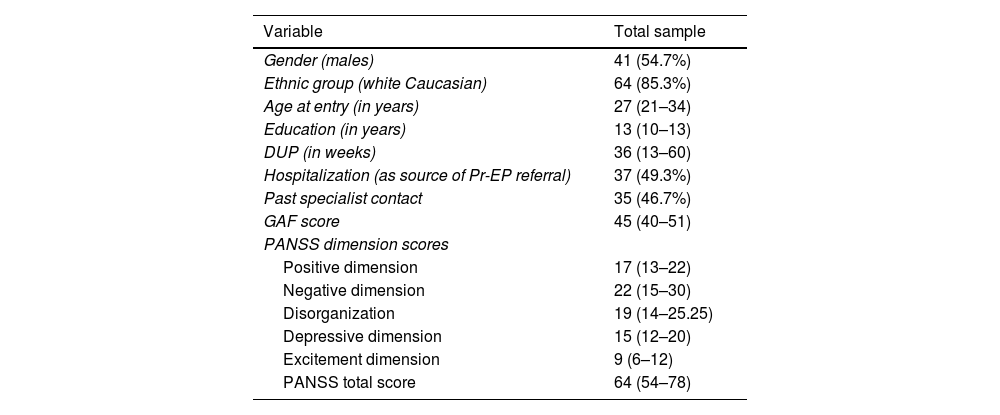
ResultsOver the course of this research, 75 FEAP patients (41 [54.7%] males; 64 [85.3%] white Caucasian) entered the Pr-EP protocol. According to the DSM-IV-TR criteria, 49 (65.3%) of them had a manic episode with psychotic features, while 26 (34.7%) had a major depressive episode with psychotic features. Sociodemographic and clinical features of the FEAP total sample at entry are shown in the Table 1. No difference in PANSS “Disorganization” dimension scores was found between FEAP patients with manic episode and those with major depressive episode both at baseline and at the end of the 2-year follow-up period (baseline: median [interquartile range]=21 [16–25] vs 18 [14–27], z=−0.704, p=0.481; 2-year assessment time=13 [9.50–16.50] vs 11 [8–15], z=−0.726, p=0.468).
Clinical, sociodemographic and psychopathological characteristics of the FEAP total sample (n=75) at baseline.
| Variable | Total sample |
|---|---|
| Gender (males) | 41 (54.7%) |
| Ethnic group (white Caucasian) | 64 (85.3%) |
| Age at entry (in years) | 27 (21–34) |
| Education (in years) | 13 (10–13) |
| DUP (in weeks) | 36 (13–60) |
| Hospitalization (as source of Pr-EP referral) | 37 (49.3%) |
| Past specialist contact | 35 (46.7%) |
| GAF score | 45 (40–51) |
| PANSS dimension scores | |
| Positive dimension | 17 (13–22) |
| Negative dimension | 22 (15–30) |
| Disorganization | 19 (14–25.25) |
| Depressive dimension | 15 (12–20) |
| Excitement dimension | 9 (6–12) |
| PANSS total score | 64 (54–78) |
Legend: Frequencies (percentages) and median (interquartile range) are reported. FEAP=First Episode Affective Psychosis; DUP=Duration of Untreated Psychosis; Pr-EP=“Parma-Early Psychosis” program; GAF=Global Assessment of Functioning, PANSS=Positive And Negative Syndrome Scale.
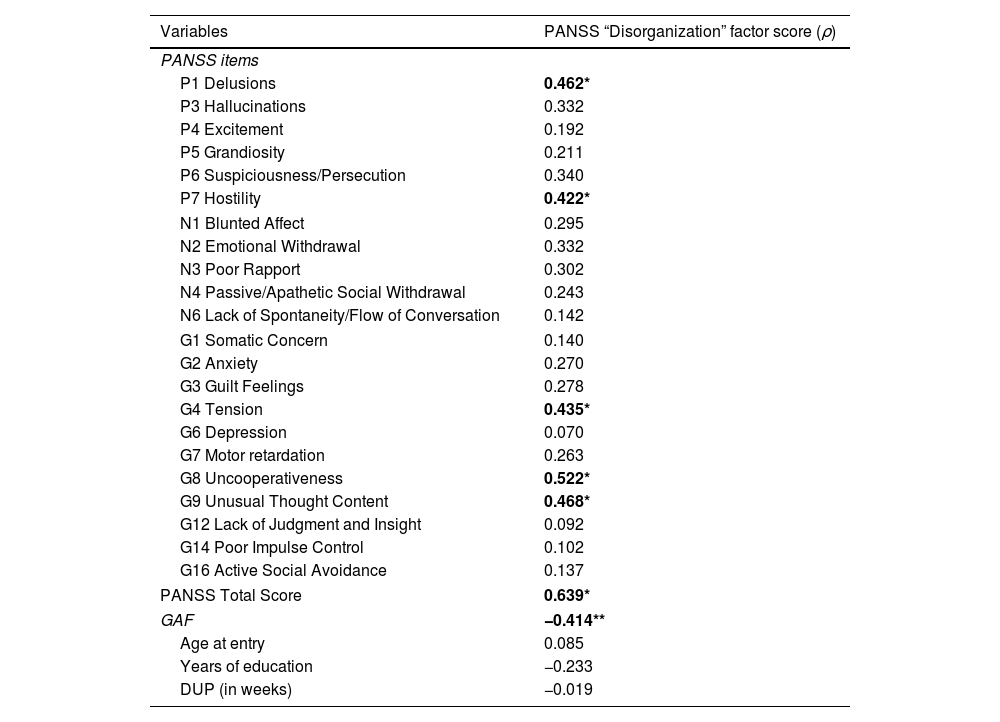
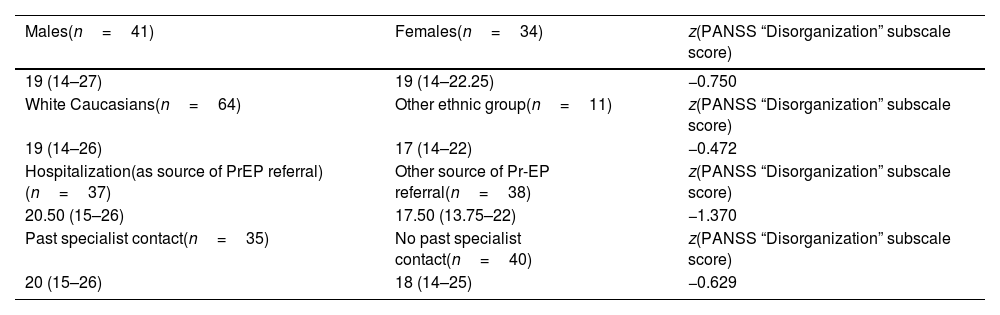
At the initial assessment (T0), PANSS “Disorganization” dimension subscore had significant positive correlations with PANSS total score and PANSS “Delusions”, “Unusual Thought Content”, “Hostility”, “Uncooperativeness” and “Tension” item subscores (Table 2). Moreover, it showed a statistically relevant negative correlation with the GAF score, regardless of the severity of manic and depressive symptoms, Indeed, also controlling for PANSS “Depression” and “Excitement” dimension subscores, negative correlation between disorganization and GAF score remained statistically significant (controlling for PANSS “Excitement” dimension subscore: ρ=−0.326, p=0.005; controlling for PANSS “Depression” dimension subscore: ρ=−0.385, p=0.001). Furthermore, no baseline associations of disorganization with negative symptoms, depression and excitement item subscores, sociodemographic and clinical characteristics (including hospitalization as source of Pr-EP referral and past specialist contact [i.e. in previous illness episodes, before the Pr-EP enrollment]) were observed (Table 3).
Baseline associations of PANSS “Disorganization” dimension score with psychopathology, functioning, sociodemographic and clinical features in the FEAP total group (n=75).
| Variables | PANSS “Disorganization” factor score (ρ) |
|---|---|
| PANSS items | |
| P1 Delusions | 0.462* |
| P3 Hallucinations | 0.332 |
| P4 Excitement | 0.192 |
| P5 Grandiosity | 0.211 |
| P6 Suspiciousness/Persecution | 0.340 |
| P7 Hostility | 0.422* |
| N1 Blunted Affect | 0.295 |
| N2 Emotional Withdrawal | 0.332 |
| N3 Poor Rapport | 0.302 |
| N4 Passive/Apathetic Social Withdrawal | 0.243 |
| N6 Lack of Spontaneity/Flow of Conversation | 0.142 |
| G1 Somatic Concern | 0.140 |
| G2 Anxiety | 0.270 |
| G3 Guilt Feelings | 0.278 |
| G4 Tension | 0.435* |
| G6 Depression | 0.070 |
| G7 Motor retardation | 0.263 |
| G8 Uncooperativeness | 0.522* |
| G9 Unusual Thought Content | 0.468* |
| G12 Lack of Judgment and Insight | 0.092 |
| G14 Poor Impulse Control | 0.102 |
| G16 Active Social Avoidance | 0.137 |
| PANSS Total Score | 0.639* |
| GAF | −0.414** |
| Age at entry | 0.085 |
| Years of education | −0.233 |
| DUP (in weeks) | −0.019 |
Legend: PANSS=Positive And Negative Syndrome Scale; FEAP=First Episode Affective Psychosis; GAF=Global Assessment of Functioning scale; DUP=Duration of Untreated Psychosis; * Holm–Bonferroni corrected p value <0.001; ** Holm–Bonferroni corrected p value <0.01. Spearman's rank correlation coefficient (ρ) values are reported. Statistically significant correlations are in bold. Strength of the Spearman's correlation values are defined as follows: 0.90–1.00=very strong correlation, 0.70–0.89=strong correlation, 0.40–0.69=moderate correlation, and 0.10–0.39=weak correlation.
Baseline associations of PANSS “Disorganization” dimension score with sociodemographic and clinical features in the FEAP total group (n=75).
| Males(n=41) | Females(n=34) | z(PANSS “Disorganization” subscale score) |
|---|---|---|
| 19 (14–27) | 19 (14–22.25) | −0.750 |
| White Caucasians(n=64) | Other ethnic group(n=11) | z(PANSS “Disorganization” subscale score) |
| 19 (14–26) | 17 (14–22) | −0.472 |
| Hospitalization(as source of PrEP referral)(n=37) | Other source of Pr-EP referral(n=38) | z(PANSS “Disorganization” subscale score) |
| 20.50 (15–26) | 17.50 (13.75–22) | −1.370 |
| Past specialist contact(n=35) | No past specialist contact(n=40) | z(PANSS “Disorganization” subscale score) |
| 20 (15–26) | 18 (14–25) | −0.629 |
Legend: PANSS=Positive And Negative Syndrome Scale; FEAP=First Episode Affective Psychosis; Pr-EP=Parma early Psychosis program. Median (interquartile range) and Mann–Whitney U test (z) values are reported.
Additionally, also exclusively considering FEAP participants with manic episode, no significant baseline correlation of PANSS “Disorganization” subscale score with PANSS item subscores representing specific excitement features was found (PANSS “Excitement” item score: ρ=0.246; p=0.089; PANSS “Grandiosity” item score: ρ=0.309; p=0.097). Similarly, only considering FEAP patients with major depression, no baseline association of disorganization with PANSS item subscores capturing specific depressive characteristics was observed (PANSS “Depression” item score: ρ=−0.227; p=276; PANSS “Guilt Feelings” item score: ρ=0.183; p=0.379).
In the FEAP total group at entry, we notably found high prevalence rates of previous specialist contact (n=35; 46.7%) and hospitalization (n=37; 49.3%) (Table 1). Specifically, the most frequent DSM-IV-TR diagnoses in previous specialist contact were depressive disorders (n=14; 40%), conduct disorder (n=8; 22.8%), anxiety disorders (n=7; 20%) and learning disabilities (n=4; 11.4%).
Follow-up resultsAll FEAP subjects concluded the 2-year follow-up period. After the first year of treatment (T1), the median of individual psychotherapy sessions was 13.50 (interquartile range=9–19.75), the median of psychoeducational sessions for family members was 5 (interquartile range=2.50–8.50) and the median of case management sessions was 16 (interquartile range=9–24). At entry, 70 (93.3%) out of 75 FEAP participants were taking antipsychotics (mean equivalent dose of chlorpromazine=162.18±120.54mg/day). At the 1-year follow-up assessment time, antipsychotic medication was still prescribed to 53 (70.7%) FEAP patients (mean equivalent dose of chlorpromazine=123.35±114.88mg/day).
At the end of the 2-year follow-up period (T2), the median of individual psychotherapy sessions was 23 (interquartile range=15–30.25), the median of psychoeducational sessions for family members was 8.50 (interquartile range=7–12.75) and the median of case management sessions was 30 (interquartile range=15.17–46). At the T2 assessment, antipsychotic medication was still prescribed to 39 (52%) FEAP individuals (mean equivalent dose of chlorpromazine=162.50±122.96mg/day).
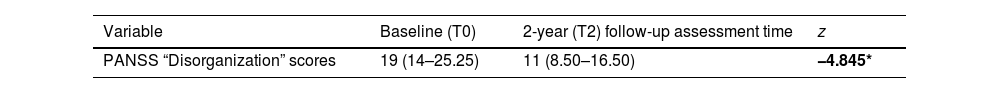
Across the 2 years of follow-up, a significant decrease in the PANSS “Disorganization” subscale score was observed (Table 4). Furthermore, the difference (delta) between T0 and T2 PANSS “Disorganization” dimension scores (i.e. the longitudinal improvement in disorganization levels) maintained statistically relevant positive correlations with deltas in T0 and T2 PANSS total scores and PANSS “Uncooperativeness” and “Tension” item subscores, as well as a significant negative correlation with the delta in T0 and T2 GAF scores. No longitudinal associations of PANSS “Disorganization” domain scores with negative symptoms, positive symptoms, depression and excitement item subscores, baseline clinical and sociodemographic features were found.
PANSS “Disorganization” dimension subscores and their associations with specialized treatment components of the Pr-EP program, functioning, psychopathology, clinical and sociodemographic characteristics along the 2-year follow-up period in the FEAP total sample (n=75).
| Variable | Baseline (T0) | 2-year (T2) follow-up assessment time | z |
|---|---|---|---|
| PANSS “Disorganization” scores | 19 (14–25.25) | 11 (8.50–16.50) | −4.845* |
| Variables(T0-T2 Delta PANSS scores) | T0-T2 Delta PANSS “Disorganization” score(ρ) |
|---|---|
| PANSS items | |
| P1 Delusions | 0.372 |
| P3 Hallucinations | 0.299 |
| P4 Excitement | 0.327 |
| P5 Grandiosity | 0.306 |
| P6 Suspiciousness/Persecution | 0.243 |
| P7 Hostility | 0.402 |
| N1 Blunted Affect | 0.428 |
| N2 Emotional Withdrawal | 0.360 |
| N3 Poor Rapport | 0.200 |
| N4 Passive/Apathetic Social Withdrawal | 0.157 |
| N6 Lack of Spontaneity/Flow of Conversation | 0.159 |
| G1 Somatic Concern | 0.215 |
| G2 Anxiety | 0.389 |
| G3 Guilt Feelings | 0.272 |
| G4 Tension | 0.459** |
| G6 Depression | 0.195 |
| G7 Motor retardation | 0.415 |
| G8 Uncooperativeness | 0.428** |
| G9 Unusual Thought Content | 0.405 |
| G12 Lack of Judgment and Insight | 0.179 |
| G14 Poor Impulse Control | 0.176 |
| G16 Active Social Avoidance | 0.094 |
| PANSS Total Score | 0.700* |
| GAF | −0.433** |
| Variables | T0-T1 Delta PANSS “Disorganization” score(ρ) |
|---|---|
| T0 equivalent dose of Chlorpromazine (mg/day) | 0.228 |
| T1 equivalent dose of Chlorpromazine (mg/day) | 0.124 |
| T1 number of individual psychotherapy sessions | 0.085 |
| T1 number of family psychoeducational sessions | 0.228 |
| T1 number of case management sessions | 0.097 |
| Pr-EP combined interventions | 0.401*** |
| Variables | T0-T2 Delta PANSS “Disorganization” score(ρ) |
|---|---|
| T0 equivalent dose of Chlorpromazine (mg/day) | 0.026 |
| T1 equivalent dose of Chlorpromazine (mg/day) | 0.154 |
| T2 equivalent dose of Chlorpromazine (mg/day) | 0.102 |
| T2 number of individual psychotherapy sessions | −0.232 |
| T2 number of family psychoeducational sessions | 0.090 |
| T2 number of case management sessions | 0.009 |
| Pr-EP combined interventions | 0.202 |
| Age at entry | −0.042 |
| Education (in years) | −0.124 |
| DUP (in weeks) | 0.066 |
| T2 days of hospitalization | −0.227 |
| Males(n=41) | Females(n=34) | z(T0-T2 Delta PANSS “Disorganization” score) |
| 6.50 (2–10.50) | 7 (3.75–10) | −0.288 |
| White Caucasian(n=64) | Other Ethnic Group(n=11) | z(T0-T2 Delta PANSS “Disorganization” score) |
| 6 (2–10) | 9 (4.75–9.50) | −0.775 |
Legend: PANSS=Positive And Negative Syndrome Scale; Pr-EP=Parma-Early Psychosis Program; FEAP=First Episode Affective Psychosis; T0=baseline; T1=1-year follow-up assessment time; T2=2-year follow-up assessment time; Pr-EP combined interventions=antipsychotic therapy+psychosocial treatments; median (interquartile range), Wilcoxon test (z), Sperarman's rank correlation coefficient (ρ) and Mann–Whitney U test (z) values are reported; ** Holm–Bonferroni corrected p value <0.001; ** Holm–Bonferroni corrected p value <0.01; *** Holm–Bonferroni corrected p value <0.05. Statistically significant results are in bold. Strength of the Spearman's correlation values are defined as follows: 0.90–1.00=very strong correlation, 0.70–0.89=strong correlation, 0.40–0.69=moderate correlation, and 0.10–0.39=weak correlation.
However, exclusively considering FEAP patients with manic episode, statistically relevant longitudinal correlations of the difference in T0 and T2 PANSS “Disorganization” subscale scores with deltas in T0 and T2 PANSS item subscores describing specific clinical characteristics of excitement were found (T0-T2 Delta PANSS “Excitement” item score: ρ=0.512; p=0.002; T0-T2 delta PANSS “Grandiosity” item score: ρ=0.513; p=0.002). Differently, only considering FEAP participants with major depression, no longitudinal associations of disorganization with deltas in T0 and T2 PANSS item subscores representing describing specific depressive features were observed (PANSS “Depression” item score: ρ=0.014; p=0.276; PANSS “Guilt Feelings” item score: ρ=0.133; p=0.610).
Finally, the delta in T0 and T1 PANSS “Disorganization” dimension scores had a statistically relevant positive correlation with the simultaneous delivery of the specific treatments (i.e. antipsychotic therapy+psychosocial intervention) offered to FEAP patients during the first year of the Pr-EP program (Table 4). However, this significant association was not confirmed at the end of the 2-year follow-up period.
DiscussionOur results showed a significant baseline correlation between disorganization levels and PANSS total score in FEAP patients. This suggests that disorganized symptoms may be overall considered as early psychopathological indices of global clinical severity in young people with FEAP already at their enrollment in specialized EIP programs.32,33 This finding is also in line with previous evidence on association between high baseline levels of disorganization and later transition to overt psychosis in individuals with at-risk mental states.34,35 In the present research, the link between disorganized symptoms and PANSS global severity was also enduring over time.
Psychopathological suggestionsWe found significant enduring correlations (i.e. both at baseline and along the 2-year follow-up period) between disorganization and delusional thinking (specifically, PANSS “Delusions” and “Unusual Though Content” item scores [but not with the PANSS “Grandiosity” item subscore]). This supports that disorganized and positive symptoms may be considered as salient, comorbid psychopathological characteristics also in early-onset affective psychosis (i.e. in adolescents and young adults with early psychosis outside schizophrenia spectrum disorders).36,37 Therefore, differential diagnosis with schizophrenia should be routinely formulated in case of early-onset first episode psychosis.38 It remains to be clarified in our young FEAP population how commonly psychotic depression may precede psychotic mania. Indeed, depressive episodes are frequent at the onset of bipolar disorder, with incidence rates that vary from 50% to 80% in different studies.39
Furthermore, in the FEAP total group, no relevant correlations of disorganization with PANSS items specifically describing core features of excitement, depressive and negative symptom dimensions were observed. Only an enduring association between disorganized symptoms and PANSS “Tension” subscore (typically depicting a specific somatic characteristic of anxiety)10 was also found. Therefore, disorganization, negative symptoms, excitement and depression seem to be independent domains in the psychopathology of young FEAP patients. As the only exception, exclusively considering FEAP individuals with manic episode, persistent associations of severity in disorganized features with excitement and grandiosity were reported over time.
Our results also showed relevant baseline correlations of disorganized symptoms with some PANSS items representing clinical aspects involved in treatment resistance (i.e. hostility and uncooperativeness). In line with what has been previously reported in individuals with prolonged psychosis,40 this finding seems to suggest that severity in disorganization levels could play a negative role in treatment adherence in FEAP patients, already at their first specialist contact with specific EIP programs. Our evidence of an enduring relationship between disorganization and uncooperativeness also suggests that a longitudinal improvement in disorganized symptoms may contribute to increase compliance with specialized, evidence-based EIP interventions over time.
Moreover, results of this study showed a significant, persistent correlation between disorganization and decline in daily functioning, right from the patient's recruitment in a dedicated EIP program. This reduction seems to be independent from the baseline severity of manic or depressive symptoms. Longitudinal association between disorganization and functioning deterioration is in line with what was observed in previous research on individuals with prolonged bipolar disorder or chronic psychosis, suggesting that the most severely disorganized subjects have greater difficulties in real-world functioning.1,11 However, our evidence of a longitudinal improvement in disorganized symptoms matched an overtime increase in patient's daily functioning.
Finally, no associations of disorganization with hospitalization (as source of Pr-EP referral), DUP and sociodemographic features at entry were also found. On the contrary, Buoli and colleagues39 recently observed that duration of untreated illness in bipolar disorder resulted to be longer in individuals with early-onset psychotic symptoms (also including disorganized features). In this respect, Moller41 also found that high levels of disorganization in young people with first-episode psychosis were associated to a shortened DUP and could reduce treatment delay. However, as observed in our previous studies,20,42 the median DUP in young subjects with first episode psychosis decreased during the first six years of Pr-EP clinical activity. This could partially affect the difference in DUP results.
Treatment suggestionsOur results showed a decrease in disorganized dimension across a 2-year follow-up period. In the first year of treatment, this symptom reduction was significantly correlated with the simultaneous delivery of the psychosocial components of the Pr-EP program (i.e. family psychoeducation+individual psychotherapy+case management) and antipsychotic medication (although no specific Pr-EP intervention alone appeared to individually play a key role in the longitudinal decrement of disorganization levels). This seems to suggest the relevance of integrating specialized psychosocial treatments with antipsychotic therapy already at the onset of FEAP,43 together with the need of including specific therapeutic modules on disorganization in psychosocial interventions within EIP services, especially for better managing the severity of disorganized symptoms and other related, critical clinical dimensions (e.g. functioning deterioration, compliance with treatment, engagement in mental healthcare pathways),44 and to favor patients’ clinical and functional recovery, right from the FEAP onset. The intensity of EIP treatment sessions in the first years of intervention also seems to be a crucial parameter for improving patient's resilience and reducing the “drop-out” phenomenon.45 However, this interesting finding was not confirmed at the end of our follow-up. Considering that most of the Pr-EP psychosocial treatment sessions were provided within the first year of intervention,20 maintaining the same intensity of engagement in mental healthcare pathways at least still along 2–3 years of our Pr-EP protocol could further consolidate the longitudinal decrease in disorganized symptoms and the clinical/functional recovery of young FEAP patients.
LimitationsA first limitation was related to the assessment of the PANSS “Disorganization” dimension, which it has been mainly validated in patients with schizophrenia spectrum disorders. Although using this meta-analytic factor could be reasonable, it should be administered with caution across non-schizophrenia diagnostic groups. Further research is needed to determine the extent to which this structure model can be accurately applied outside schizophrenia spectrum disorders.
Moreover, another limitation involves the longitudinal stability of the disorganized construct along the illness course. Indeed, it has been reported a potential change in the PANSS “Disorganization” dimension structure overtime. In this respect, Amoretti and co-workers46 observed that disorganization factor did not have the same item composition at baseline and after a 2-year follow-up period in a clinical population of young patients with first episode psychosis. This potential factor instability could partially interfere with our longitudinal findings. Third, even if a strength of this research could be to have participants with FEAP within a “real-world” setting mainly engaged in providing optimal mental healthcare pathways within public, community psychiatric services, it should also be noted that our results are not also generalizable to individuals in different illness course (e.g. patients with prolonged affective psychosis and long-term medication).
Fourth, the current study was developed within an EIP protocol not specifically focused on disorganization. Indeed, psychometric assessment of major psychopathology in our research used the PANSS, which is a clinical instrument commonly administered in clinical populations with early psychosis, but not originally developed for disorganization. However, despite the lack of scales specifically centered on disorganization in young people with first episode psychosis and given the widespread use of the PANSS to assess psychopathology in such clinical samples, our findings have the potential to be replicated in other FEAP populations and offer a lead to further investigate disorganized symptoms in the early phases of affective psychosis. This is of crucial importance, since empirical studies on this topic are still relatively scarce and disorganized dimension has a detrimental effect on daily functioning and is predictive of poor prognosis.
Another weakness of this research is that we could not evaluate the potential link between neurocognitive functioning and disorganized symptoms (even if recent studies reported that they seem to be separate dimensions).8 Therefore, further investigations examining this relationship also in FEAP patients are needed. However, known intellectual disability was an exclusion criterion in this research.
Finally, another limitation was also the relatively small sample size. Thus, further research in larger clinical populations with FEAP to confirm our promising results are needed.
ConclusionsDisorganization is a relevant psychopathological dimension in young patients with FEAP already at their enrollment in specialized EIP programs, where it seems to be a stable, longitudinal index of psychopathological severity. Specifically, disorganized symptoms in FEAP patients show persistent correlations with decline in daily functioning and poor treatment adherence. However, improvement in disorganized features appears to be responsive to the simultaneous delivery of antipsychotic medication and specific psychosocial interventions provided to FEAP subjects in the first year of our EIP treatment.
FundingThis research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interestNone declared.
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sectors. The Pr-EP program was partly financed through a special, treatment-oriented regional fund: “Progetto Esordi Psicotici della Regione Emilia Romagna”.
For their facilitating technical and administrative support in the Pr-EP program, the authors gratefully acknowledge the “Early Psychosis Facilitators Group” members (Sabrina Adorni, Andrea Affaticati, Anahi Alzapiedi, Paolo Ampollini, Patrizia Caramanico, Maria Teresa Gaggiotti, Tiziana Guglielmetti, Mauro Mozzani, Matteo Rossi, Lucilla Maglio, Matteo Tonna, Fabio Vanni and Matteo Zito) and the “Quality Staff Group” members (Patrizia Ceroni, Stefano Giovanelli, Leonardo Tadonio) of the Parma Department of Mental Health and Pathological Addictions. The authors also wish to thank all the patients and family members who actively participated to the Pr-EP program.