COVID-19 spreads between people in close contact. Social isolation, which is linked with increased suicide risk, prevents COVID-19 from spreading. Suicide and COVID-19 may therefore represent two antagonistic phenomena. Specifically, we tested whether previous cross-national suicide rates inversely correlate with COVID-19 cases and deaths across countries.
Material and methodsWe ran unadjusted bivariate correlations between the most updated (2016) cross-national Age-Standardised suicide rates and COVID-19 cumulative cases and deaths (as of: 30/08/2020, 11/10/2020 and 30/05/2021) across countries; and we controlled for WHO Income group, WHO region, suicide data quality, and urbanicity.
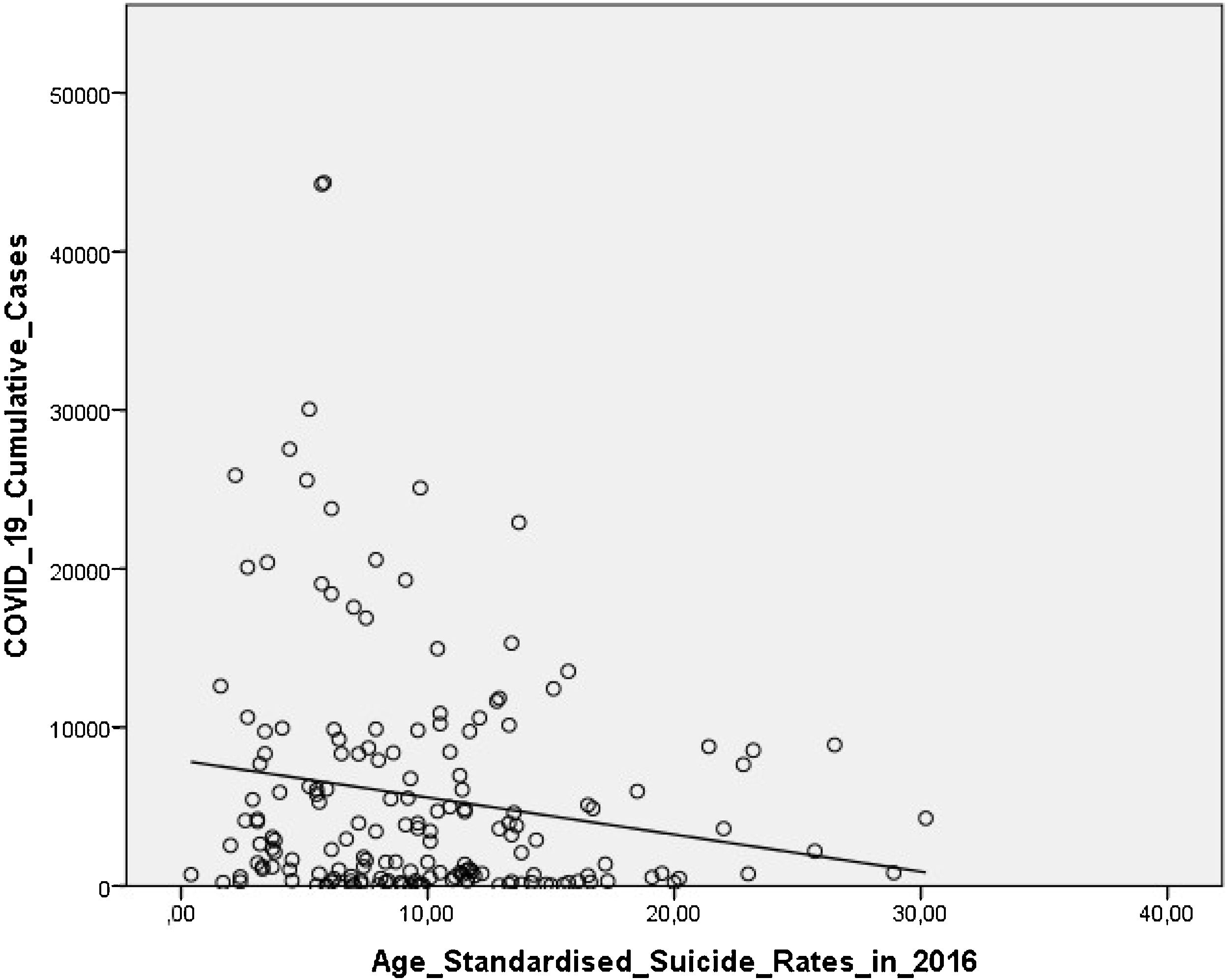
ResultsSuicide rates negatively correlated with COVID-19 cumulative cases up to 30/08/2020 (r=−0.14, P=.064) and up to 11/10/2020 at an almost significant level (r=−0.149, P=.050) across 174 countries. As of 11/10/2020 this correlation became significant when controlling for WHO region (r=−0.17, P=.028), data quality (r=−0.181, P=.017) and urbanicity (r=−0.172, P=.039); and as of 30/08/2020 when adjusting for WHO region (r=−0.15, P=.047) and data quality a (r=−0.16, P=.036). No significant correlations between suicide rates and COVID-19 deaths were found.
ConclusionsThere seems to be an inverse correlation between previous cross-national suicide rates and COVID-19 cumulative cases across countries. Suicide and COVID-19 appear to behave, to some degree, as antagonistic phenomena, which challenges their prevention.
Suicide has become a major public health issue, which accounts for approximately 800,000 deaths every year across the world.1 Of concern, suicide rates have significantly increased worldwide since the 2007 economic recession.2 However, cross-national suicide rates vary significantly1 due to relevant between-country differences in well-established suicide risk factors, such as gender,3 marital status,4 socioeconomic inequalities and education level,5 ethnicity and migration,6,7 culture and religion,8 and social integration and rurality.9,10
The sociology of suicide was put forward by Émile Durkheim's 1897 seminal contribution entitled ‘LeSuicide’.11 Since then, objective social isolation (e.g., living alone or rurality) and subjective feelings of loneliness have been consistently linked with increased suicide risk.9
The coronavirus disease (COVID-19) outbreak began in December 2019 in China and has spread across the globe ever since, which accounts for over four millions deaths.12 The COVID-19 is caused by the SARS-CoV-2 virus, which most commonly spreads between people in close contact (2 arm's length) through respiratory droplets produced when an infected person coughs, sneezes, or talks.12 As a result, very restrictive measures based on ensuring physical distancing, such as working from home, school closures, curfew, quarantine, and confinement, have been implemented,12 all of which may lead to negative mental health outcomes,13,14 including increased suicide risk,15,16 although some measures17,18 may mitigate this.
Hence, the COVID-19 pandemic spread and suicide may represent, to some degree, two antagonistic phenomena. While social cohesion/integration – low suicide rates countries – may favour the COVID-19 spread, countries with higher levels of social isolation – higher suicide rates – will be less severely affected by COVID-19. More specifically, this exploratory study aimed to test two hypotheses: (i) that previous cross-national suicide rates will be inversely associated with the spread of COVID-19 across countries; and (ii) that Region, wealth, data quality, and urbanicity will affect the above relationship. Of note, we did not intend to examine the impact of the COVID-19 pandemic on suicide rates since 2020 suicide mortality data are currently unavailable and COVID-19 pandemic may persist for several years.19 Rather, our research question focused on whether previous suicide rates inversely correlate with the impact of COVID-19 across countries, which may have crucial implications on preventing suicide, COVID-19, and future epidemics/pandemics ahead.
Material and methodsData sourcesWe extracted data from two large WHO-based open-access datasets on suicide mortality and COVID-19 data across countries. In particular, we made a linkage between the most up-to-date (2016) suicide mortality data from the 2019 WHO ‘Suicide in the world: Global Health Estimates’ report1 and three WHO weekly situation reports on COVID-19 cases and deaths across countries published on: (i) 31/08/2020, that is, data as of 30/08/202020; (ii) 12/10/2020, that is, updated as of 11/10/202012; and (iii) on 1/6/2021, i.e., data updated up to 30/05/2021.21 Thus, we included COVID-19 data on the first wave (30/08/2020), the first and second waves (11/10/2020), and up to 01/06/2021, although the end date of the first and second COVID-19 waves varied across the globe.22,23
VariablesAge-Standardised suicide rates (per 100,000 inhabitants/year in 2016) across WHO Member States (MSs, i.e., ‘countries’) were taken.
We retrieved data on COVID-19 cumulative cases and deaths per 100,000 people across countries from three WHO weekly reports on 31/08/2020,20 12/10/2020,12 and on 1/06/2021,21 that is, including data as of 30/08/202020 (first wave), 11/10/202012 (first and second waves) and as of the 30/05/2021.21
Additional variables included: WHO suicide data quality (which ranged from 1, very high, to 4, very poor), WHO region (Africa, Americas, Eastern-Mediterranean, European, South-East Asia and Western-Pacific), WHO Income group (Low, Lower-Middle, Upper-Middle and High), density – number of people per square kilometre of the total surface area – and urbanicity – the proportion of people living in urban areas (i.e., with ≥100,000 inhabitants) – according to the United Nations.24
StatisticsFirst of all, for descriptive purposes we reported the relationship between five variables of interest, namely WHO region, WHO Income group, data quality, density and urbanicity, all of which have been described above, and: (i) 2016 cross suicide rates (Table 1), (ii) COVID-19 cumulative cases (Table 2) and iii) COVID-19 cumulative deaths (Table 3). Specifically, for nominal variables – WHO region, WHO Income group and quality of data – we performed chi-square tests, while for continuous variables, such as density and urbanicity, non-parametric bivariate correlations were conducted. Second, unadjusted bivariate non-parametric correlations (i.e., Spearman's test) examined the relationship between Age-Standardised suicide rates and COVID-19 cumulative cases and deaths as of 30/08/2020, 11/10/2020 and 30/05/2021 since these variables did not follow a normal distribution according to the Kolmogorov–Smirnov test, thus testing the first hypothesis. Third, we also conducted these correlations adjusted for four variables individually, namely WHO Region, WHO Income group, WHO suicide data quality, and urbanicity to test the second hypothesis, i.e., the potential individual contribution of each of these variables to the above correlation between Age-Standardised suicide rates and COVID-19 cumulative cases as of 30/08/2020, 11/10/2020 and 30/05/2021.
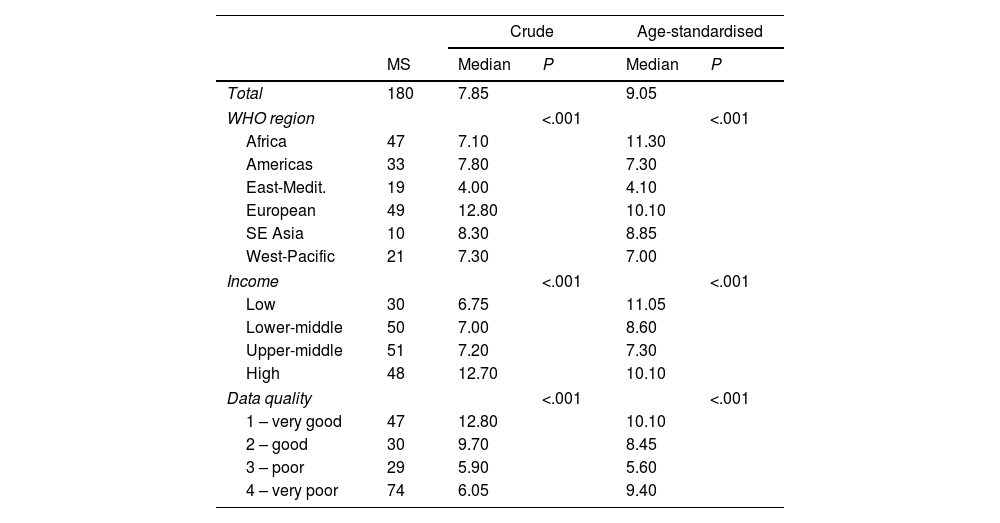
Relationship between 2016 suicide rates (per 100,000 inhabitants) and descriptive variables.
| Crude | Age-standardised | ||||
|---|---|---|---|---|---|
| MS | Median | P | Median | P | |
| Total | 180 | 7.85 | 9.05 | ||
| WHO region | <.001 | <.001 | |||
| Africa | 47 | 7.10 | 11.30 | ||
| Americas | 33 | 7.80 | 7.30 | ||
| East-Medit. | 19 | 4.00 | 4.10 | ||
| European | 49 | 12.80 | 10.10 | ||
| SE Asia | 10 | 8.30 | 8.85 | ||
| West-Pacific | 21 | 7.30 | 7.00 | ||
| Income | <.001 | <.001 | |||
| Low | 30 | 6.75 | 11.05 | ||
| Lower-middle | 50 | 7.00 | 8.60 | ||
| Upper-middle | 51 | 7.20 | 7.30 | ||
| High | 48 | 12.70 | 10.10 | ||
| Data quality | <.001 | <.001 | |||
| 1 – very good | 47 | 12.80 | 10.10 | ||
| 2 – good | 30 | 9.70 | 8.45 | ||
| 3 – poor | 29 | 5.90 | 5.60 | ||
| 4 – very poor | 74 | 6.05 | 9.40 | ||
| r | P | r | P | |
|---|---|---|---|---|
| Density | −0.00 | .97 | −0.01 | .29 |
| Urbanicity | 0.25 | .002 | −0.00 | .97 |
MS: Member State (World Health Organization). WHO: World Health Organisation. East-Medit.: East-Mediterranean WHO region. SE Asia: South-East Asia WHO region.
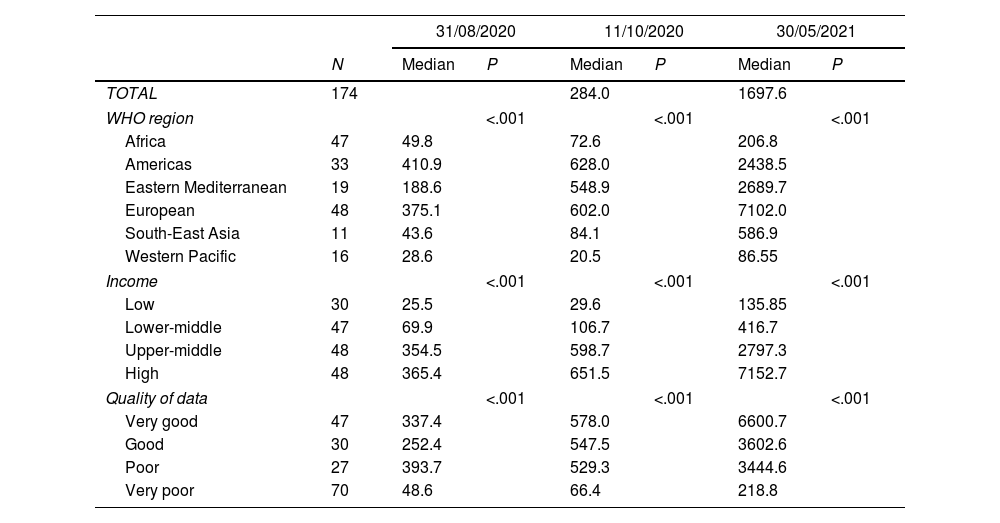
Relationship between COVID-19 cumulative cases (per 100,000 inhabitants) and descriptive variables.
| 31/08/2020 | 11/10/2020 | 30/05/2021 | |||||
|---|---|---|---|---|---|---|---|
| N | Median | P | Median | P | Median | P | |
| TOTAL | 174 | 284.0 | 1697.6 | ||||
| WHO region | <.001 | <.001 | <.001 | ||||
| Africa | 47 | 49.8 | 72.6 | 206.8 | |||
| Americas | 33 | 410.9 | 628.0 | 2438.5 | |||
| Eastern Mediterranean | 19 | 188.6 | 548.9 | 2689.7 | |||
| European | 48 | 375.1 | 602.0 | 7102.0 | |||
| South-East Asia | 11 | 43.6 | 84.1 | 586.9 | |||
| Western Pacific | 16 | 28.6 | 20.5 | 86.55 | |||
| Income | <.001 | <.001 | <.001 | ||||
| Low | 30 | 25.5 | 29.6 | 135.85 | |||
| Lower-middle | 47 | 69.9 | 106.7 | 416.7 | |||
| Upper-middle | 48 | 354.5 | 598.7 | 2797.3 | |||
| High | 48 | 365.4 | 651.5 | 7152.7 | |||
| Quality of data | <.001 | <.001 | <.001 | ||||
| Very good | 47 | 337.4 | 578.0 | 6600.7 | |||
| Good | 30 | 252.4 | 547.5 | 3602.6 | |||
| Poor | 27 | 393.7 | 529.3 | 3444.6 | |||
| Very poor | 70 | 48.6 | 66.4 | 218.8 | |||
| r | P | r | P | r | P | |
|---|---|---|---|---|---|---|
| Density | −0.00 | .99 | 0.04 | .63 | 0.12 | .16 |
| Urbanicity | 0.56 | <.001 | 0.59 | <.001 | 0.59 | <.001 |
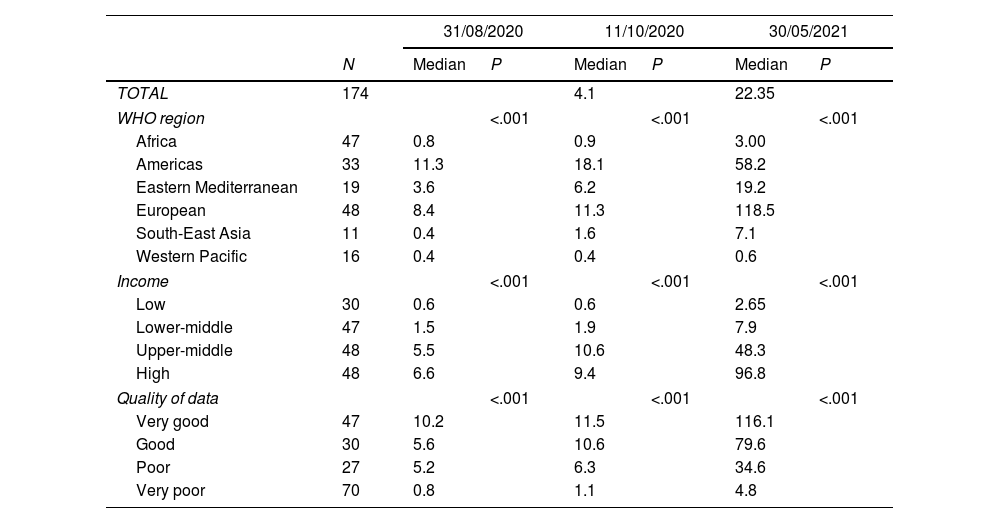
Relationship between COVID-19 cumulative deaths (per 100,000 inhabitants) and descriptive variables.
| 31/08/2020 | 11/10/2020 | 30/05/2021 | |||||
|---|---|---|---|---|---|---|---|
| N | Median | P | Median | P | Median | P | |
| TOTAL | 174 | 4.1 | 22.35 | ||||
| WHO region | <.001 | <.001 | <.001 | ||||
| Africa | 47 | 0.8 | 0.9 | 3.00 | |||
| Americas | 33 | 11.3 | 18.1 | 58.2 | |||
| Eastern Mediterranean | 19 | 3.6 | 6.2 | 19.2 | |||
| European | 48 | 8.4 | 11.3 | 118.5 | |||
| South-East Asia | 11 | 0.4 | 1.6 | 7.1 | |||
| Western Pacific | 16 | 0.4 | 0.4 | 0.6 | |||
| Income | <.001 | <.001 | <.001 | ||||
| Low | 30 | 0.6 | 0.6 | 2.65 | |||
| Lower-middle | 47 | 1.5 | 1.9 | 7.9 | |||
| Upper-middle | 48 | 5.5 | 10.6 | 48.3 | |||
| High | 48 | 6.6 | 9.4 | 96.8 | |||
| Quality of data | <.001 | <.001 | <.001 | ||||
| Very good | 47 | 10.2 | 11.5 | 116.1 | |||
| Good | 30 | 5.6 | 10.6 | 79.6 | |||
| Poor | 27 | 5.2 | 6.3 | 34.6 | |||
| Very poor | 70 | 0.8 | 1.1 | 4.8 | |||
| r | P | r | P | r | P | |
|---|---|---|---|---|---|---|
| Density | −0.05 | .58 | −0.04 | .59 | −0.01 | .92 |
| Urbanicity | 0.49 | <.001 | 0.53 | <.001 | 0.53 | <.001 |
A significant level of 5% was set for all the above correlations, which were performed using the Statistical Package for Social Science version 25.0 (SPSS, Inc., Chicago, IL, USA).
ResultsCross-national suicide ratesOf the current 194 WHO MSs, we retrieved the WHO suicide estimates for 2016 in 180 MSs (92.8%). In the supplementary material (Table S1), we have listed these 180 MSs according to the WHO Region group. Of these, only 76 MSs (42.2%) had very good or good quality of data. European (49 MSs) and African (47 MSs) WHO regions accounted for approximately half the WHO MSs. Only 48 MSs (26.7%) were classified as High Income, most of which (29 MSs, 60.4%) were in the European WHO Region.
2016 Age-Standardised suicide rates per 100,000 inhabitants in 2016 ranged from 0.4 (Barbados) to 30.2 (Guyana), with a global median of 9.05. Africa accounted for the highest suicide rate (11.30), while the WHO Eastern Mediterranean region had lowest regional suicide rate (4.10).
Suicide rates significantly (P<.001) differed in WHO region, WHO Income Group and data quality (Table 1).
COVID-19 cases and deaths across countriesUp to 30/05/2021 the WHO confirmed 169,604,858 cases in 176 MSs, in most of which (n=130, 74.3%) there was community transmission. Cumulative COVID-19 cases per 100,000 people ranged from 0.5 (Samoa) to 21,095.1 (Slovenia), with an overall median of 1697.6.
Up to 30/05/2021, 3,530,837 people died from COVID-19 across the world. In 6 WHO MSs (United Republic of Tanzania, Lao People's Democratic Republic, Samoa, Solomon Islands, Vanuatu, and Vietnam) cumulative deaths per 100,000 people were reported as 0, which peaked in Hungary (303.2). As of 30/05/2021, the overall median of cumulative COVID-19 deaths per 100,000 people was 22.35.
The Americas WHO Region accounts for almost half of total COVID-19 cumulative cases (N=67,178,933, 40%) and deaths (N=1,646,407, 47%). Between-WHO-region differences in COVID-19 cumulative cases and deaths reached significance (P<.001), as shown in Table 1. The High- and Upper-Middle Income groups had the highest medians for cumulative cases (7152.7 and 2797.3, respectively) and deaths (96.8 and 48.3, respectively), which significantly (P<.001) differed from the Lower-Middle (cases: 416.7; deaths: 7.9) and Low-Income groups (cases: 135.85; deaths: 2.65) (Tables 2 and 3).
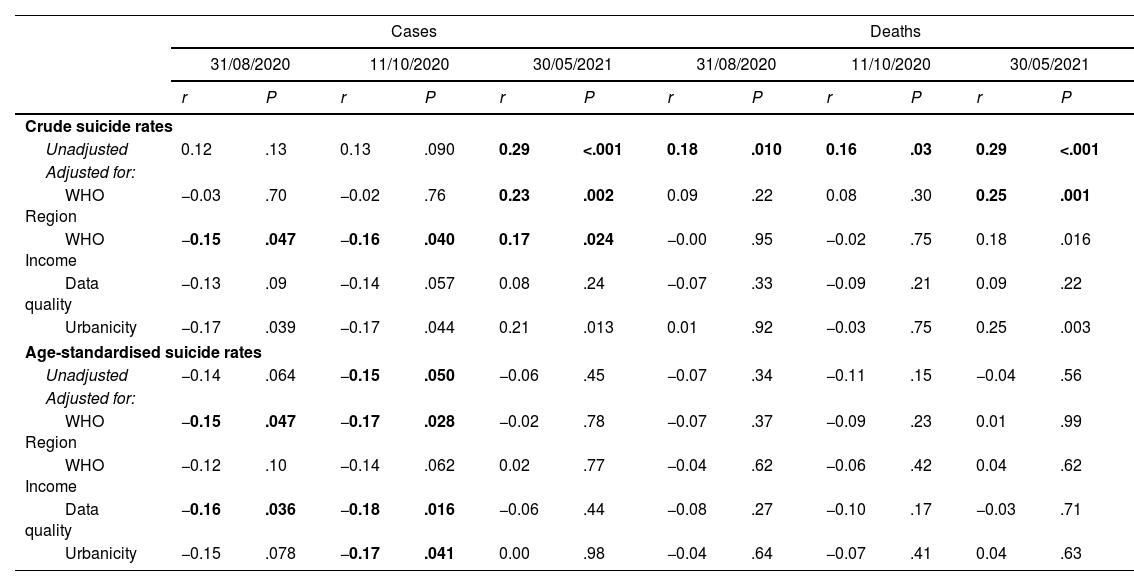
Bivariate correlations between cross-national suicide rates and COVID-19 dataSeveral associations between 2016 cross-national suicide rates and COVID-19 cumulative cases and deaths across countries emerged from the analyses (Table 4).
Bivariate correlations between 2016 suicide rates and COVID-19 cumulative cases and deaths.
| Cases | Deaths | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 31/08/2020 | 11/10/2020 | 30/05/2021 | 31/08/2020 | 11/10/2020 | 30/05/2021 | |||||||
| r | P | r | P | r | P | r | P | r | P | r | P | |
| Crude suicide rates | ||||||||||||
| Unadjusted | 0.12 | .13 | 0.13 | .090 | 0.29 | <.001 | 0.18 | .010 | 0.16 | .03 | 0.29 | <.001 |
| Adjusted for: | ||||||||||||
| WHO Region | −0.03 | .70 | −0.02 | .76 | 0.23 | .002 | 0.09 | .22 | 0.08 | .30 | 0.25 | .001 |
| WHO Income | −0.15 | .047 | −0.16 | .040 | 0.17 | .024 | −0.00 | .95 | −0.02 | .75 | 0.18 | .016 |
| Data quality | −0.13 | .09 | −0.14 | .057 | 0.08 | .24 | −0.07 | .33 | −0.09 | .21 | 0.09 | .22 |
| Urbanicity | −0.17 | .039 | −0.17 | .044 | 0.21 | .013 | 0.01 | .92 | −0.03 | .75 | 0.25 | .003 |
| Age-standardised suicide rates | ||||||||||||
| Unadjusted | −0.14 | .064 | −0.15 | .050 | −0.06 | .45 | −0.07 | .34 | −0.11 | .15 | −0.04 | .56 |
| Adjusted for: | ||||||||||||
| WHO Region | −0.15 | .047 | −0.17 | .028 | −0.02 | .78 | −0.07 | .37 | −0.09 | .23 | 0.01 | .99 |
| WHO Income | −0.12 | .10 | −0.14 | .062 | 0.02 | .77 | −0.04 | .62 | −0.06 | .42 | 0.04 | .62 |
| Data quality | −0.16 | .036 | −0.18 | .016 | −0.06 | .44 | −0.08 | .27 | −0.10 | .17 | −0.03 | .71 |
| Urbanicity | −0.15 | .078 | −0.17 | .041 | 0.00 | .98 | −0.04 | .64 | −0.07 | .41 | 0.04 | .63 |
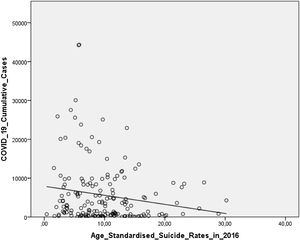
2016 Age-Standardised suicide rates inversely correlated with COVID-19 cumulative cases (r=−0.149, P=.050) and COVID-19 deaths (r=−0.110, P=.150) up to the 11/10/2020, which remained significant after adjusting for region (r=−.164, P=.031), data quality (r=−0.181, P=.017), and urbanicity (r=−0.172, P=.039), whilst adjusting for WHO Income Group made this association borderline (r=−0.140, P=.067). These results were mostly replicated for COVID-19 cumulative cases and deaths as of 30/08/2020, but not when analysing data up to 30/05/2021 (Table 4).
Fig. 1 graphically shows the unadjusted correlation between 2016 Age-Standardised suicide rates and COVID-19 cumulative cases across countries as of 11/10/2020.
DiscussionMain findingsThe way of transmission of COVID-19 between people in physical (hence, social) contact and the association of social isolation with suicide, as proposed by Durkheim over a century ago11 and replicated ever since,9 led us to postulation that suicide and COVID-19 may represent two antagonistic phenomena (hypothesis i). Consistent with this, analyses revealed an “almost significant” inverse correlation between previous (i.e., 2016) cross-national suicide rates and COVID-19 cumulative cases as of 30/08/2020 – first wave – (P=.067), which persisted as of 11/10/2020 – first and second waves – (P=.050) across 174 countries worldwide. Although we suggested other variables, such as urbanicity, region, data quality, and wealth, to affect this association (hypothesis ii), we did not find evidence of this. However, the above results were far from significance when analysing COVID-19 data as of 30/05/2021. This is likely to reflect the confounding effect of the ongoing vaccination campaign, including relevant between-country differences, and new variants of the virus, which have spread across countries very differently too, which is discussed further below.
Interpretation of the findingsSuicide researchers from all over the world are committed to establishing the impact of the COVID-19 pandemic on suicide rates in the years to come.15,16,19 However, this issue cannot be addressed at present since 2020 suicide mortality data are not available yet25 and the COVID-19 pandemic may persist for several years.12 This noted, preliminary data from 21 countries showed that the impact of the COVID-19 pandemic on suicide rates may be weaker than previously thought,26 although this finding should be taken cautiously. Indeed, previous epidemics, such as the 1918 Spanish Flu27 and the 2003 Severe Acute Respiratory Syndrome (SARS) epidemic outbreak in Hong-Kong28 and in Taiwan29 were linked with an increased suicide rate at a local-regional level, in which social isolation was thought to play a relevant role.28
From a different approach, this study examined the relationship between previous suicide rates and the COVID-19 spread across the globe. In particular, results showed an inverse association of previous (2016) suicide rates with COVID-19 cases and deaths across countries, that is, ‘the higher the suicide rates, the weaker the COVID-19 impact; and viceversa’, in line with our first hypothesis based on the Durkheim's sociological model of suicide11 and the way of transmission of the SARS-CoV-2. However, so far combatting the COVID-19 pandemic has focused on physical distancing-related measures, including quarantine and confinement,12 which may increase suicide risk due to social isolation. Indeed, individuals should be strongly encouraged to ‘keep socially (but not physically)connected’15 for preventing suicide in the COVID-19 era, which, in light of our results, seems to be a challenging goal. In other words, physical distancing-based measures may increase suicide risk in those ‘low suicide rates’ countries, which have been severely affected by COVID-19. Moreover, the anticipated rise in unemployment during the post-COVID-19 years30 may make us approach a perfect storm leading to an unacceptable increase in suicide rates all over the world,15,31 which may also remain high for years.29 Hence, physical distancing-based strategies for addressing the COVID-19 pandemic and future epidemics and pandemics, may need to be, somehow, reformulated. In addition, suffering COVID-19 appears to be associated with an increased risk of developing reactive psychoses characterised by suicidal ideation at first presentation.32
In keeping with this, it can be speculated that risk of the Durkheim's four types of suicidal behaviour may increase in the years ahead.33 First, physical distancing-based strategies may make individuals gradually lose the sense of belonging to the community, thus leading to frustration, depression, and hopelessness, i.e., Egoistic suicidal behaviours. Longer-term, development of a sense of entrapment and loneliness,34 that is, the feeling of “not belonging to the community anymore”, may result in so-called Anomic suicide. These two types of suicide according to Durkheim may predominantly affect those subjects who were more weakly bounded to the community. Second, healthcare workers and those affected by COVID-19 with fear (or too much awareness) of potentially spreading the infection to other members of the community may end up with Altruistic suicidal behaviours. Third, restrictive societal measures such as curfew and prolonged confinement may result in pessimistic thoughts about the future, thus making Fatalistic suicidal acts more likely.
In addition, these findings should warn us about the potentially stronger impact of future epidemics/pandemics across ‘low suicide rates’ countries, i.e., with higher levels of social cohesion/integration, which have been more severely affected by the COVID-19, as revealed by results. On the other hand, ‘high suicide rates’ countries, i.e., with higher levels of social isolation, may be, somehow, protected from epidemics/pandemics, which either have succeeded in defeating the COVID-19 (e.g., South Korea, China, or Japan) or just have been less severely affected by the pandemic (e.g., Lithuania). These findings are supported further by the strong association of urbanicity, as a proxy for social cohesion/integration, with COVID-19 cumulative cases and deaths across the globe (Tables 2 and 3).
Other variables, such as urbanicity, Region, wealth, or data quality did not alter the above association between age-standardised suicide rates and cumulative COVID-19 cases, which conflicted our hypothesis ii. However, this unexpected result would provide further support for the main contribution of this study (hypothesis i) to the field, namely the inverse association of previous suicide rates with COVID-19 cases, particularly during the first and second waves.
This inverse relationship between suicide rates and COVID-19 cumulative cases was not replicated when analysing COVID-19 data as of 30/05/2021, which may have been due to the ongoing vaccination campaign, with relevant between-country differences. Also, new variants of the virus, which may be associated with greater contagiousness and/or lethality, have predominantly spread across some regions. Future studies using updated suicide and COVID-19 data are therefore warranted.
Lessons for preventionDuring the post-COVID-19 years suicide rates are likely to increase worldwide due to an economic turndown and rise in unemployment,2 although active labour market programmes may mitigate this.35 Also, strategies for battling the COVID-19 pandemic based on reducing physical contact with others may result in higher levels of social isolation, a well-known risk factor for suicide.15,16,18,19 Can we really stop the COVID-19 pandemic (and future epidemics/pandemics ahead) from spreading without increasing suicide risk owing to higher levels of social isolation? More specifically, what can these study findings tell us about how to achieve this?
In short, coordinated multiagency approaches are warranted to ‘keep socially (but not physically) connected‘.15 Specific strategies include mental health promotion campaigns,18 new technologies and remote tele-health-based resources,36 and reducing social stigma,12 which was demonstrated to be a major suicide risk factor,37 which is of particular concern in older age people.17 However, the Internet and social media to ‘keep socially (but not physically)connected’15 may contribute to so-called Werther effect.38,39 Moreover, the extent to which social media-based relationships make people feel supported remains far from clear, as we sadly learnt from the “Facebook suicide woman”, which may promote suicidal events through direct media transmission,38 particularly in vulnerable people.40 In keeping with this, social media abuse was proposed to underlie the significant increase in adolescents and young adults suicide rates in the US from 2000 to 2017.41 Much attention should be paid to all these issues, particularly taking into account the expected duration of the COVID-19 pandemic and the potential outbreak of further epidemics/pandemics in the years to come. On the other hand, resilience and socialsupport reduced suicidal ideation risk after the COVID-19 lockdown in a general population-based longitudinal study.42
Strengths and limitationsTo our knowledge, this is the first study in examining the relationship between previous cross-national suicide rates and COVID-19 spread across the globe, which therefore makes a novel contribution to the field. We drew data from two large WHO datasets on 174 MSs and we demonstrated an inverse association between both phenomena, thus supporting hypothesis i, which could not be explained by other contributors, which conflicted hypothesis ii. As discussed above, these findings may have crucial implications on tackling suicide, COVID-19 and future epidemics to come.
However, this study has some limitations. First, the WHO datasets relied on information available from each WHO MS, which varied significantly, and quality of data was rated as poor/very poor for most countries. Second, 2016 suicide data were compared with 2020–2021 COVID-19 cases and deaths. Therefore, no causality conclusions can be drawn from these associations, which may also change over time, although this study did not aim to investigate the effect of the COVID-19 pandemic on suicide rates. Third, this study was exploratory and other non-tested variables, such as healthcare services provision and access and per capita Gross Domestic Product (GDP), may have affected the results. In keeping with this, countries within the same region and comparable in terms of income, such as Spain, France, United Kingdom, or Germany, do not appear to have replicated the above inverse relationship between suicide rates and COVID-19 impact, which requires further investigation.
ConclusionsResults showed an inverse relationship between 2016 cross-national suicide rates and COVID-19 spread across the globe, which was not due to other analysed variables, such as urbanicity, region, wealth, and quality of data. Hence, suicide and COVID-19 appear to represent two antagonistic phenomena, which challenges their prevention. In particular, defeating COVID-19 and future epidemics/pandemics cannot occur at the unacceptable price of increased suicide rates.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of interestsThe authors declare that they have no conflict of interest.
Authors acknowledge departmental/institutional support from their institutions detailed above for the preparation and medical writing of this article.
This study was not funded or sponsored by any specific funding source. All authors’ salaries came from their institutions detailed above, which had no role in hypothesis generation, study design, decision to publish, or the manuscript writing.
There are no conflicts of interest to declare in relation to this study's subject.