Clozapine has superior characteristics among other antipsychotics.1 Evidence and experience support clozapine as the best treatment in terms of efficacy, effectiveness and well-being, the gold standard for treatment resistant schizophrenia (TRS).2–4 It has also shown efficacy in differential psychopathological dimensions: negative, cognitive or affective symptoms.5 It has been demonstrated its results in terms of overall mortality and suicide.6 Despite its superiority, its use has been limited by the possibility of presenting lethal adverse effects.7 The risk of associated neutropenia (number of leukocytes less than 3.0×103/μL or absolute neutrophil count less than 1.5×103/μL) described reaches between 3.8% and 1% depending on studies.9
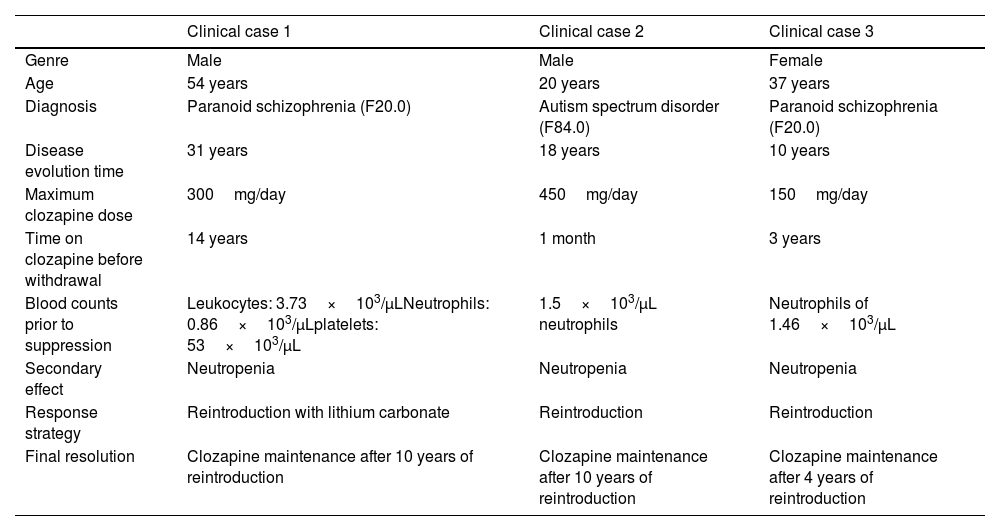
Rechallenging clozapine after neutropenia is a tough decision and each case should be analyzed individually.11 We present three clinical cases in which, after presenting neutropenia, clozapine was reintroduced, as well as the evolution of years later, in the first and the second ten and in the third four (Table 1).
Summary of the three clinical cases.
| Clinical case 1 | Clinical case 2 | Clinical case 3 | |
|---|---|---|---|
| Genre | Male | Male | Female |
| Age | 54 years | 20 years | 37 years |
| Diagnosis | Paranoid schizophrenia (F20.0) | Autism spectrum disorder (F84.0) | Paranoid schizophrenia (F20.0) |
| Disease evolution time | 31 years | 18 years | 10 years |
| Maximum clozapine dose | 300mg/day | 450mg/day | 150mg/day |
| Time on clozapine before withdrawal | 14 years | 1 month | 3 years |
| Blood counts prior to suppression | Leukocytes: 3.73×103/μLNeutrophils: 0.86×103/μLplatelets: 53×103/μL | 1.5×103/μL neutrophils | Neutrophils of 1.46×103/μL |
| Secondary effect | Neutropenia | Neutropenia | Neutropenia |
| Response strategy | Reintroduction with lithium carbonate | Reintroduction | Reintroduction |
| Final resolution | Clozapine maintenance after 10 years of reintroduction | Clozapine maintenance after 10 years of reintroduction | Clozapine maintenance after 4 years of reintroduction |
A 55-year-old patient was diagnosed with paranoid schizophrenia since 1990. He started clozapine in 1998, maintaining psychopathological stability with a sustained dose of 300mg/24h. Active consumption of 30 cigarettes per day. In August 2012, neutropenia was detected with numbers of neutrophils: 0.86×103/μL, leukocytes: 3.73×103/μL, and platelets: 53×103/μL. After reducing clozapine and starting aripiprazole (15mg/d), the neutrophil counts normalized in December. The patient presented signs of psychopathological decompensation. Subsequently, intestinal injury in response to imposing auditory hallucinations was described. This caused the need for urgent surgery in January 2013 with a diagnosis of acute abdomen. Different antipsychotic drugs were tested at appropriate doses and in combination, quetiapine, aripiprazole, olanzapine, haloperidol, risperidone; with little response. It was decided restarting treatment with clozapine at a dose of 50mg/day associated with lithium carbonate (600mg). The patient presented progressive psychopathological improvement with no repercussions on haematological figures: plasma lithium levels: 0.54mEq/l; clozapine plasma levels: 191ng/mL; neutrophils: 3.77×10[3]/μL, Leukocytes: 5.98×10[3]/μL; Platelets: 149×10[3]/μL. Subsequently, they normalized, remaining in this way during the ten years of follow-up, also presenting psychopathological stability.
Clinical case 2A 21-year-old patient with coagulation factor V and VII deficiency and follow-up in Neurology for suspected epilepsy. He has been going to mental health since January 2003, with a diagnosis of autism spectrum disorder. In 2009, the start of clozapine was evaluated after different antipsychotics that had been insufficient for the behavioural control of the patient, starting in December. In January 2010, neutrophils of 1.5×103neutrophils/μL appeared. One month after clozapine withdrawal, neutrophil levels returned to normal. At this time, treatment with clozapine was discontinued, starting with quetiapine, risperidone, olanzapine, aripiprazole, psychostimulants and clonazepam, which was insufficient. Finally, in September 2013, clozapine was reintroduced with close analytical monitoring. In the ten years of evolution in which the patient continues with clozapine, no analytical alterations have been observed.
Clinical case 3A 38-year-old woman began her mental health follow-up in 2011. She attended urgently due to the presence of commentator-type auditory hallucinations and insomnia. No evidence of previous diseases of interest or consumption of substances of abuse. Start of treatment with risperidone; later changes to aripiprazole (30mg/day). In 2014, she was diagnosed with paranoid schizophrenia. A switch was made to olanzapine (20mg/day), later to paliperidone (15mg/day) and ziprasidone (8mg/day). In January 2016, a clozapine regimen was started, presenting an improvement in the patient's positive and negative symptoms with a 150mg/day dose. In 2019, a progressive decrease in neutrophils appeared again with minimum levels of 1.46×103/μL, requiring a reduction in the dose of clozapine until its withdrawal in August 2019. In October, neutrophil levels were 3.02×103/μL, delusional ideation reappearing of reference and control, pseudo-perceptions and negative symptomatology. Clozapine was rechallenge in November 2019. Serial tests have been performed since the reintroduction without a decrease in neutrophil levels.
A review of three clinical cases from our Mental Health management area in which clozapine was reintroduced after discontinuation of treatment due to an episode of neutropenia has been carried out. The importance of these cases lies both in the rechallenge and in the positive evolution that they have had years later. It is recommended to restart clozapine in TRS if it was interrupted due to moderate leukopenia or neutropenia but not with the presence of agranulocytosis.10 According to the bibliography, the tendency to reintroduce should be different depending on the adverse effect presented. The normalization of haematological values and the study of the cause of neutropenia are essential before reintroduction. It is recommended to monitor haematological values every two weeks for at least 3 months after reintroduction.